Nonalcoholic fatty liver disease (NAFLD) is a medical condition that may progress to end-stage liver disease. The spectrum of NAFLD is wide and ranges from simple fat accumulation in hepatocytes (steatosis), to fat accumulation plus necroinflammatory activity with or without fibrosis (steatohepatitis). In addition, NAFLD is the most common cause of abnormal liver-test results among adults with a prevalence of 13%-23%. This case report is an example of a patient with asymptomatic hypertransaminasemia and severe hepatic steatosis without inflammation in which the diagnosis was made by liver biopsy.
Nonalcoholic fatty liver disease (NAFLD) is a medical condition that may progress to end-stage liver disease.1 The spectrum of NAFLD is wide and ranges from simple fat accumulation in hepatocytes (steatosis) without biochemical or histological evidence of inflammation or fibrosis, to fat accumulation plus necroinflammatory activity with or without fibrosis (steatohepatitis), to the development of advanced liver fibrosis or cirrhosis (cirrhotic stage).2 NAFLD is the most common cause of abnormal liver-tests results among adults.3 Is well known that liver biopsy is the gold standard for NAFLD diagnosis.3,4 Some studies have evaluated radiological imaging for NAFLD diagnosis with variable results.5,6 Magnetic resonance imaging (MRI) has been the most trusted image study for NAFLD detection. None of the radiological imaging studies has proven to difference between NAFLD and NASH.5 This case report is an example of a patient with asymptomatic hypertransaminasemia and severe hepatic steatosis without inflammation in which the diagnosis was made by liver biopsy.
Case report
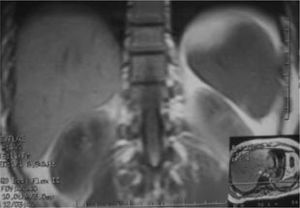
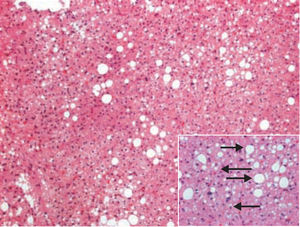
The patient, a 43 year old men, with family history of hypertension and diabetes mellitus and self history of hepatitis A virus infection at 20 year old without complications, initiate his disease as a discovery during check up with an asymptomatic high transaminase level (ALT 93 U/L). There are not any risk factors for liver disease (alcohol consumption, blood transfusion, intravenous drugs) and there were no abnormal signs in physical examination related with this finding. Anthropometric data was associated with overweight (body mass index 26.8 Kg/ m2). Serum glucose concentration was 105 mg/dL, insulin 6.9 μU/L, and HOMA index 1.8. Hepatitis B virus (HBV) and hepatitis C virus (HCV) infections were overruled by the detection of HBV antigens, anti-HBV antibodies and HCV-RNA which were negative. Other causes of liver disease like hemochromatosis, and autoimmune hepatitis were discarded detecting anti-mitochondrial antibodies, anti-smooth muscle antibodies, anti-microsomal antibodies were also negative, and iron serum levels (202 mg/ dL). Both abdominal ultrasound (US) and MRI (Figure 1) were reported normal. Laparoscopic liver biopsy was performed and analyzed by an expert pathologist who informed peripheric ischemic necrosis of central veins with parenchimal collapse areas with linphohystiocitic aggregates and grade 3 macro and microvesicular steatosis without inflammation data (Figure 2).
DiscussionNAFLD prevalence currently has increased, and ranges from 13%-23% in different studies among adults.6 In Mexico the estimated prevalence is 23.6%.7 In a study made by Skelly et al.,8 liver biopsy was made in 354 patients with sustained abnormal liver tests being NASH, fatty liver and cryptogenic hepatitis the most prevalent findings with 34%, 32% and 9% respectively.
Recent studies have shown a high incidence of NAFLD in patients with overweight and obesity having a strong association with metabolic syndrome. A study made by Saadeh et al.5 showed high performance between image studies; US and computerized tomography were 100% and 93% sensitive in detecting > 33% fat, with positive predictive values of 62% and 76% respectively: Joy et al.6 report the utility of MRI using this technique it is also possible to measure the fat fraction, and a good correlation has been shown between such magnetic resonance measurements and histological fat (r = 0.86), using calibration procedures, the technique of magnetic resonance spectroscopy also allows the determination of hepatic fat volume fractions with good histological correlation (r = 0.7). In this case although abdominal MRI and US were performed, none of them reported clear alterations being liver biopsy the only way to determine the presence of a high-grade hepatic steatosis.
The BAAT (body mass index, age, ALT, triglyceride) score has been useful as a prognosis factor to determine steatosis and hepatic lesion grade.9-13 This score will never substitute liver biopsy, which currently is the gold standard for NAFLD diagnosis. However, recently three factors, insulin resistance index, ALT level and hypertension (HAIR index), were found to have significant independent predictive effects.9
Steatosis alone is not injurious to the liver. Nevertheless, the accumulation of toxic levels of free fatty acids increases the oxidative stress with formation of free radicals, including hydrogen peroxide and superoxide. Abnormal lipid peroxidation ensues, resulting in direct hepatocyte injury, release of toxic byproducts, inflammation, and fibrosis.
In some cases image studies can detect hepatic steatosis in a form that can mimicking liver metastasis as reported by Castaño et al.,14 where with the use of US imaging they found multiples nodules that measured 0.5-2 cm in diameter, witch was discarded by liver biopsy that showed moderate steatosis with multiples microlipogranulomas. In conclusion sustained hypertransaminasemia is an important factor for liver disease evaluation. In this case high-grade hepatic steatosis diagnosed with liver biopsy that didn’t show any inflammation signs was detected in a patient with sustained hypertransaminasemia. This implicates the importance of liver biopsy in patients with sustained abnormal liver-tests results and that not all patients with high transaminases levels and high-grade steatosis always have liver inflammation.