Chronic hepatitis C is a major cause of liver-related morbidity and mortality. Epidemiological data regarding this infection in developing countries is scanty. Methods: Prevalence of hepatitis C (HCV) infection was investigated in a random sample of Chilean general adult population older than 20 years of age. Additionally, frequency of HCV infection was assessed in group of native Chilean Amerindians (Mapuche Indians) living in an isolated locality of the Southern Chile. Incidence of HCV infection was estimated using serum samples separated by 7 years (1993-2000). Results: Among 959 subjects, prevalence of anti-HCV antibodies was 1.15% (95% CI 0.48-1.82%) and 0.83% when only RIBA-confirmed cases were considered. Among these subjects, 62.5% had detectable HCV RNA in serum and 40% of them had a history of blood transfusion. Age distribution of cases showed a steadily increasing prevalence with age. Estimated incidence of new HCV infections was 15 per 100,000 subjects per year in the period 1993-2000. No cases were detected among the 145 Mapuche subjects studied. Conclusions: HCV infection is a prevalent disease in the Hispanic population of Chile with a low incidence in the last decade, whereas it was not detected in an isolated Mapuche Indian community. Age distribution of prevalence suggests that the peak of infection in Chile occurred 30 to 50 years ago.
Ever since its discovery and characterization in 1989, the hepatitis C virus (HCV) has become a worldwide health issue.1 The World Health Organization (WHO) has estimated that 170 million persons are chronically infected globally with HCV, and 3 to 4 million persons are newly infected each year.2 In Europe, prevalence vary from 0.01% up to 5%. In Africa, rates up to 51% have been reported.1,3 HCV is the first cause of post-transfusion hepatitis, and its progression to liver cirrhosis and hepatocellular carcinoma is well documented.4-6 HCV infection is mostly asymptomatic, and is detected occasionally due to elevation of aminotransferases levels or routine screening of donated blood. However, the disease is also frequently detected in advanced stages due to appearance of its chronic complications.6-8 Nowadays, HCV is the most frequent indication for liver transplantation in many countries,9 this being also the case in Chile.10
The epidemiology of HCV infection in Latin American countries has not been completely characterized. Available data from Chile indicate that prevalence of HCV infection among blood donors is between 0.2 to 0.5%.11-13 Infection rates have also been studied in specific demographic groups, such as patients undergoing hemodialysis,14 pregnant women,15 patients with porphyria cutanea tarda16 and hepatocellular carcinoma.13 However, there is no available data reporting the prevalence of HCV infection in our general population. Thus, the aim of this study was to determine the incidence and prevalence of HCV infection in the Chilean population assessing HCV serology in two ethnically and geographically dissimilar groups: urban Hispanic population and rural Mapuche Indians.
MethodsStudy design and demographics: This study was approved by the Institutional Review Board for Human Studies of the School of Medicine, Pontificia Universidad Católica de Chile. Prevalence of positive anti-HCV serology was determined in serum samples of subjects 20 years of age or older who participated in a cohort study (two periods of time with a 7-year interval) designed to determine the natural history of gallstone disease in Chile.17 Two ethnically different populations were studied in two separate regions of the country. Firstly, a sample of Chilean Hispanics was enrolled from households located in La Florida district in Santiago. This was carried out using a software that randomly selected blocks with a proportional representation of the different neighborhoods of the area, according to previously described methods.17 Secondly, a group of Mapuche Indians was recruited from Huapi Island in the Southern part of Chile. Both groups were studied in 1993 and 2000. All subjects were interviewed by the authors and anthropometric characteristics, data from physical examination and a set of laboratory tests were performed. Additionally, an abdominal ultrasound was carried out in all subjects.
Ethnic characterization of subjects: The subjects were classified as Hispanics or Mapuches based on a statement of race in a questionnaire that included the presence of specific ethnic surnames and skin color. An estimation of the aborigine genetic pool present in the Hispanic and Mapuche populations was obtained by calculating the Amerindian Admixture Index (AAI) from the ABO blood group distribution, assuming a hybrid population of biparental origin.18,19 The Amerindian maternal origin was defined by the determination of the mitochondrial DNA polymorphisms in all Mapuche Indians and in a selected sample of 350 unrelated Hispanic individuals. For this purpose, genomic DNA was isolated from each subject.20 The four Amerindian founder haplotypes and sequencing analysis of the hypervariable D-loop region were performed in DNA samples of the two populations, as described previously.20-22
Serology: Anti-HCV antibodies were detected using a third-generation ELISA assay (Abbot Labs. Chicago, IL) in samples obtained during the year 2000. Positive samples were confirmed using a third-generation recombinant immunoblot assay (RIBA, Chiron Corporation, Emeryville, CA). Patients testing positive for both methods were considered true positives and HCV RNA presence was determined in their plasma samples. In addition, serological testing was performed on stored samples from 1993 for those patients testing positive in 2000.
HCV-RNA determination: HCV RNA was detected by polymerase chain reaction (PCR), using two groups of starters for the non encoding 5' region (Amplicor Test Version 2.0, Roche, Geneva, Switzerland).
Statistical methods: Demographic characteristics were described with proportions and means with standard deviations (SD). Differences among subjects positive and negative for HCV infection were calculated using Fisher’s exact test and Student’s t test as appropriate. Prevalence ranges were calculated with a 95% confidence interval. Crude incidence and prevalence were calculated.
ResultsDuring 1993, 1581 subjects from La Florida and 182 from Huapi Island were enrolled in a study on prevalence, natural history and risk factors for cholelitiasis.17 In the year 2000 the same population was reassessed, gathering information on 71% (1,117) of all patients from La Florida and 61% (145) of all patients from Huapi Island. Of all 1,117 pa-tients studied in La Florida in 2000, 964 were evaluated since 153 patients died during the period 1993-2000. From those 964 subjects, 959 individuals were studied, since 5 had a Mapuche family background. From a group of 145 individuals living in Huapi Island, 117 were enrolled during March 2001, since 28 subjects died in the previous seven years. Data concerning demographics features of both population included in this study is shown in table I
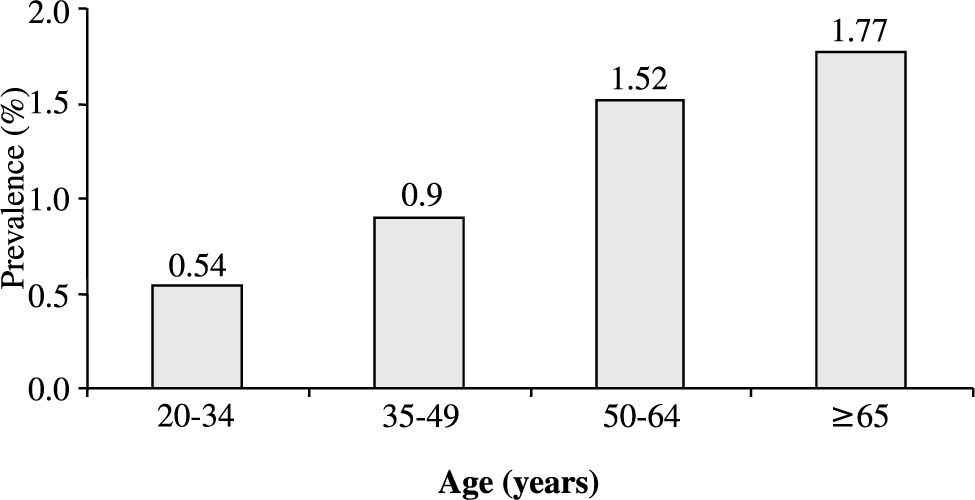
Analysis of serum samples obtained from subjects living in La Florida County, showed that 11 individuals tested positive for anti-HCV antibodies by third-generation ELISA indicating a seroprevalence of HCV infection of 1.15% (95% CI 0.48-1.82%) in Chilean Hispanic population. On the other hand, no positive samples were detected in Huapi Island. Table II shows individual results of ELISA and RIBA as well as PCR status for HCV positive patients. When only cases confirmed by RIBA were considered, the estimated HCV infection prevalence was 0.83%. Circulating HCV RNA using PCR was detectable in 62.5% of subjects with positive anti-HCV antibodies (0.52% of the entire sample). Abnormal alanine aminotransferase levels were present in 4 out of 5 (80%) patients with positive HCV viremia, none of which showed clinical or ultrasonographic signs of cirrhosis. Analysis of age distribution in individuals who tested positive for HCV (Figure 1) indicates that prevalence of infection increases progressively with age. Individuals older that 50 years old exhibit a prevalence of 1.5%. No statistically significant differences in gender were found in the prevalence of HCV infection, being 1.49% in men and 0.96% in women (p=NS).
Description of subjects with positive anti-HCV antibodies.
| Patient | Year 1993 | Year 2000 | Demographic and clinical characteristics | |||||||
|---|---|---|---|---|---|---|---|---|---|---|
| ELISA | RIBA | ELISA | RIBA | PCR | Age† | Sex | Drugs | Surgery | Blood transfusion | |
| 1 | (-) | (-) | (+) | (+) | (+) | 30 | M | (-) | (+) | (-) |
| 2 | (+) | (+) | (+) | (+) | (+) | 46 | M | (+) | (-) | (-) |
| 3 | (+) | (+) | (+) | (+) | (+) | 49 | F | (-) | (+) | (-) |
| 4 | (+) | (+) | (+) | (+) | (-) | 53 | F | (-) | (+) | (+) |
| 5 | (-) | (+) | (+) | (+) | (-) | 57 | M | (-) | (-) | (-) |
| 6 | (+) | (+) | (+) | (+) | (-) | 60 | F | (-) | (-) | (+) |
| 7 | (+) | * | (+) | (+) | (+) | 63 | F | (-) | (+) | (+) |
| 8 | (+) | (+) | (+) | (+) | (+) | 71 | F | (-) | (+) | (+) |
| 9 | (+) | (-) | (+) | (-) | (-) | 49 | M | (-) | (-) | (-) |
| 10 | (+) | (±) | (+) | (±) | (-) | 61 | F | (-) | (+) | (-) |
| 11 | (+) | (±) | (+) | * | (-) | 71 | M | (-) | (+) | (+) |
†: Age in year 2000 (+): Positive (-): Negative (±): Undetermined *: Sample not available M: Male F: Female
From a total of 8 patients with positive anti-HCV confirmed by RIBA, 4 (50%) had received blood transfusions, and 1 (13%) had a history of intravenous drug abuse. The 3 remaining patients did not have an established risk factor for HCV, although 2 of them had undergone surgery in the past.
We were able to estimate the incidence of HCV infection during the interval period of the study, by analyzing the samples stored during the period 1993-2000 which were obtained from the same patients. Table II shows that there was 1 documented case of appearance of anti-HCV antibodies (by ELISA and RIBA) during this period of time. This trans-lates to an annual incidence of 15 per 100,000 people.
DiscussionThe World Health Organization estimates that the worldwide prevalence of HCV infection is approximately 3%,23 with significant geographical and ethnical variations, possibly due to the presence and frequency of risk factors associated to the transmission of HCV inside a community.3
This is the first epidemiological study to determine the prevalence of HCV infection in the general population of Chile. ELISA tests are the most frequently used screening methods, due mainly to their availability and low cost. Sensitivity in immunocompetent population is higher than 95% using a third generation test. ELISA testing was positive in 11 of 959 individuals from La Florida (1.15%). No patients with positive serology were detected among the Mapuche population. Due to the existence of false positive results, particularly in populations with a low prevalence, or selected groups like blood donors, results must be confirmed with a second method. In our group, 8 out of 11 patients with positive ELISA (73%) had positive confirmation. Therefore, the prevalence of HCV infection in Hispanic population from Santiago in 2000 was 0.83%. This is approximately 2 to 4 times the described prevalence in blood donors in our country, probably due to the fact that blood donors are a highly selected group that does not represent the prevalence of infection in the general population. Similar situations have been reported in other countries. For example in the United States prevalence of HCV infection in voluntary blood donors is 0.6%, one third of what is described in the general population.24
The absence of positive HCV serology in Huapi Island can be explained by a relatively small sample size and by the characteristics of the small isolated rural community with little access to medical attention and procedures, and lower prevalence of certain behavioral patterns like intravenous drug abuse and sexual promiscuity. This supports also that HCV infection is not an endemic infection in Chilean Amerindians.
Our study, which was carried out in adult population (20 years or older), shows an increasing prevalence of infection with age. This distribution is similar to what is described in countries like Japan or Italy, where the estimated peak incidence of infection was 30 to 50 years ago. Age distribution of HCV infection may suggest possible means of transmission and patterns of complications for the following years. Our study suggests that HCV infection was due mainly to health related procedures, namely transfusions and administration of intravenous treatments by untrained personnel or under sub-optimal conditions, a frequent situation in our country a few decades ago. In the United States the highest prevalence is seen in young adults and decreases after the age of 50, suggesting a more recent peak of incidence, possibly associated to the increase in intravenous drug abuse between the 60s and 80s.
Regarding risk factors in the studied population, half of the infected individuals had a history of receiving blood transfusion and 13% had used intravenous drugs. The remaining 38% had no identified risk factors, except history of surgery in two thirds of them. This infection pattern is in accordance to the results of a clinical study of 147 Chilean patients with hepatitis C,25 and is similar to the pattern found in Japan and Italy, where the main means of transmission are medical procedures.
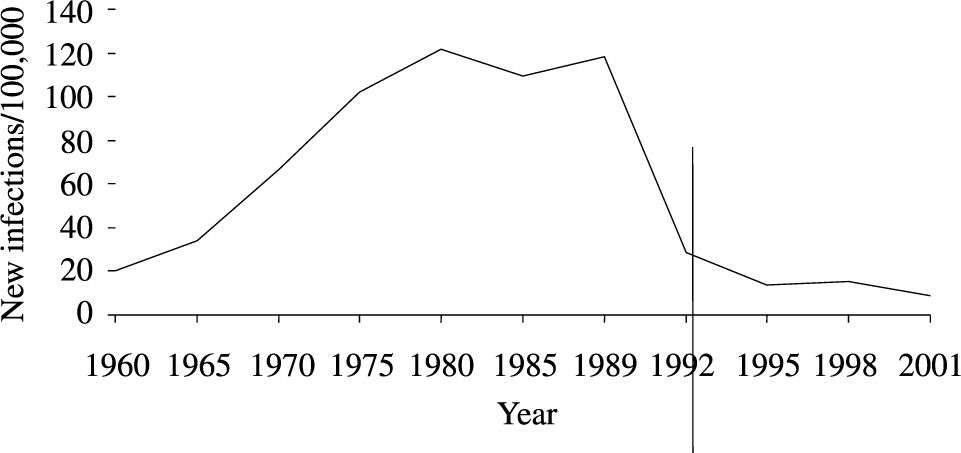
One of the most interesting aspects of this study was the possibility of analyzing serum samples obtained 7 years earlier from the same subjects. This allowed us to estimate the cumulative incidence of HCV infection during this period, resulting in 15 cases per 100,000 persons annually. This matches the estimated incidence during the same period of time in the United States (15.8 per 100,000).26Figure 2 shows the incidence of new HCV infections in the United States from 1960 to 2001, with the highest incidence during the mid-80s. In our population, given the age distribution of prevalence, we estimate this peak incidence to have happened between the 50s and 70s.
Estimated incidence of HCV infection in the United States.26
In summary, in a representative sample of the urban population of Santiago, the prevalence of HCV infection is 1.15%, with confirmed infection in 0.83%, among whom 62.5% had circulating HCV RNA. There were no cases of HCV infection in the studied Mapuche Indian population. The distribution of the infection according to age suggests that exposure to the virus occurred mainly in the setting of medical procedures (transfusion and therapeutic injections with unsafe techniques), estimating the period of maximal incidence of HCV infection 30 to 50 years ago.
Aknowledgments:Supported by a grant of the National Commission for Scientific and Technological Research (CONICYT), FONDECYT N° 1030744 to F.N and FONDECYT N° 1050782 to A.S. The authors thank Schering-Plough Chile for donating HCV ELISA assays.