The COVID-19 pandemic has pushed the healthcare system to its limits worldwide. Consequently, many resources were mobilized to guarantee care for patients with SARS-CoV-2 infection, relegating many other healthcare programs. Argentina remains one of the most affected countries by the pandemic, with over 116,000 deaths and a dramatic economic situation. In this scenario, management of other pathologies has been reduced, including solid organ transplantation. Indeed, the number of transplants has substantially decreased across the world [1]. During the first year of the pandemic, Argentina faced a significant reduction in liver donation and transplantation rates, of 59% and 55%, respectively [2]. However, the impact of all the restrictive healthcare policies on liver transplant (LT) outcomes has scantly been described. Thus, we aimed to evaluate the severity of liver disease at the time of LT and analyze the outcomes of those patients transplanted during the COVID-19 pandemic. We conducted a retrospective review of the LT database at the Austral University Hospital in Buenos Aires, Argentina. The analysis was stratified into two time periods: pre-COVID included patients from August 1, 2019 to March 19, 2020; and COVID-era included patients undergoing LT from March 20, 2020 to March 19, 2021. We analyzed demographic data and transplant-related variables. Kaplan–Meier method was used to compare survival between groups. Significance was declared for P < 0.05.
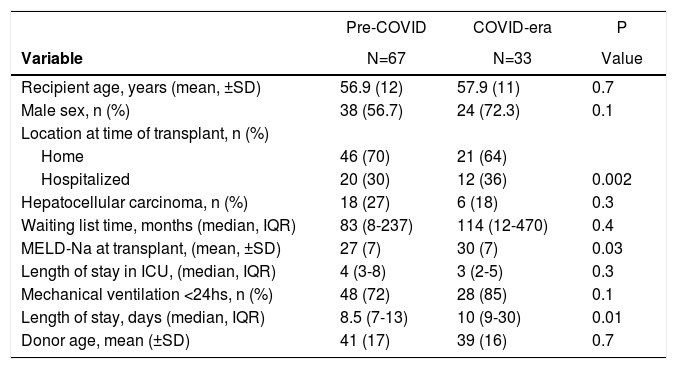
Overall, we included 100 patients, 67 patients underwent LT in the pre-COVID period and 33 subjects in the COVID-era. The immunosuppression regimen was similar in both eras. In Table 1, we describe the most important findings. Briefly, patients transplanted in the COVID-era were more likely to be hospitalized at the time of LT, with higher MELD-Na scores and longer length of hospital stay after LT. However, 90-days survival was similar when comparing transplanted patients in the pre-COVID group (89%) with those in the COVID-era (90%) (P=0.7). No deaths were COVID-related.
. Baseline characteristics of the study cohort.
Abbreviations: ICU, intensive care unit; IQR, interquartile range; MELD, model for end-stage liver disease; Na, sodium; SD, standard deviation
We believe our findings are the consequence of a prolonged strict lockdown implemented by the Argentinean authorities. The government mandated the restructuring of many public hospitals to prioritize the care of patients with SARS-CoV-2 infection. In many Latin American countries, most of the organ procurement activity is performed in public hospitals [3]. These political actions can partially explain the dramatic fall in organ procurement. Moreover, intensive care units struggled with COVID-19 patients limiting organ donation given the risk of transmission of SARS-CoV-2 infection. Patients with cirrhosis are at increased risk of developing severe COVID-19, so many of them did not attend their scheduled clinic visits [4]. Hence, the high number of cases seen during the pandemic in Argentina limited the LT procedures to only life-threatening situations. We understand these were the main reasons why patients who underwent LT were significantly sicker and had a longer hospital stay when compared with those transplanted in the pre-COVID period. The fact that the hospitalization time is longer negatively impacts the availability of beds, a very limited resource during the pandemic. Thus, our findings reinforce the idea of not neglecting other pathologies in case a new wave of COVID-19 emerges in our region.