Shunts between the superior mesenteric vein (SMV) and the right renal vein (RRV) are very rare. Here, we describe and depict the rare case of a liver transplant (LT) in the setting of shunt between SMV and RRV. A 67-year-old white man presenting with Child C cirrhosis secondary to hemochromatosis and persistent encephalopathy was listed for LT. Preoperative abdominal angiotomography revealed the presence of a large spontaneous shunt between the SMV and the RRV. The patient underwent LT by receiving a liver from a 17-year-old brain-dead deceased donor victim of trauma. A large shunt between the SMV and the RRV was confirmed intraoperatively. Although there was no portal vein (PV) thrombosis, the PV was atrophic and had a reduced flow. PV pressure was 22mmHg (an arterial line was inserted inside the PV stump, and this line was connected to a common pressure transducer, the pressure readings was expressed in the anesthesia monitor). After shunt ligation PV pressure increased to 32mmHg. There were no post-transplant vascular complications, and the patient was discharged home in good health. Preoperative study of all LT candidates with angio CT scan is mandatory. Whenever there is PV thrombosis, an attempt to remove the entire thrombus is warranted. After thrombectomy or whenever there is not PV thrombosis, all large shunts should be ligated. PV pressure and flow should be measured before and after shunt ligation. In the absence of PV thrombosis, ligation of the shunt should enable an increase in PV flow and pressure, as reported herein.
Portal vein (PV) thrombosis may trigger the occurrence of spontaneous portosystemic shunts.[1,2] However shunts between the superior mesenteric vein (SMV) and the right renal vein (RRV) are very rare.[3] We were not able to find any operative picture of this rare shunt. Here, we describe and depict the rare case of a LT in the setting of shunt between SMV and RRV.
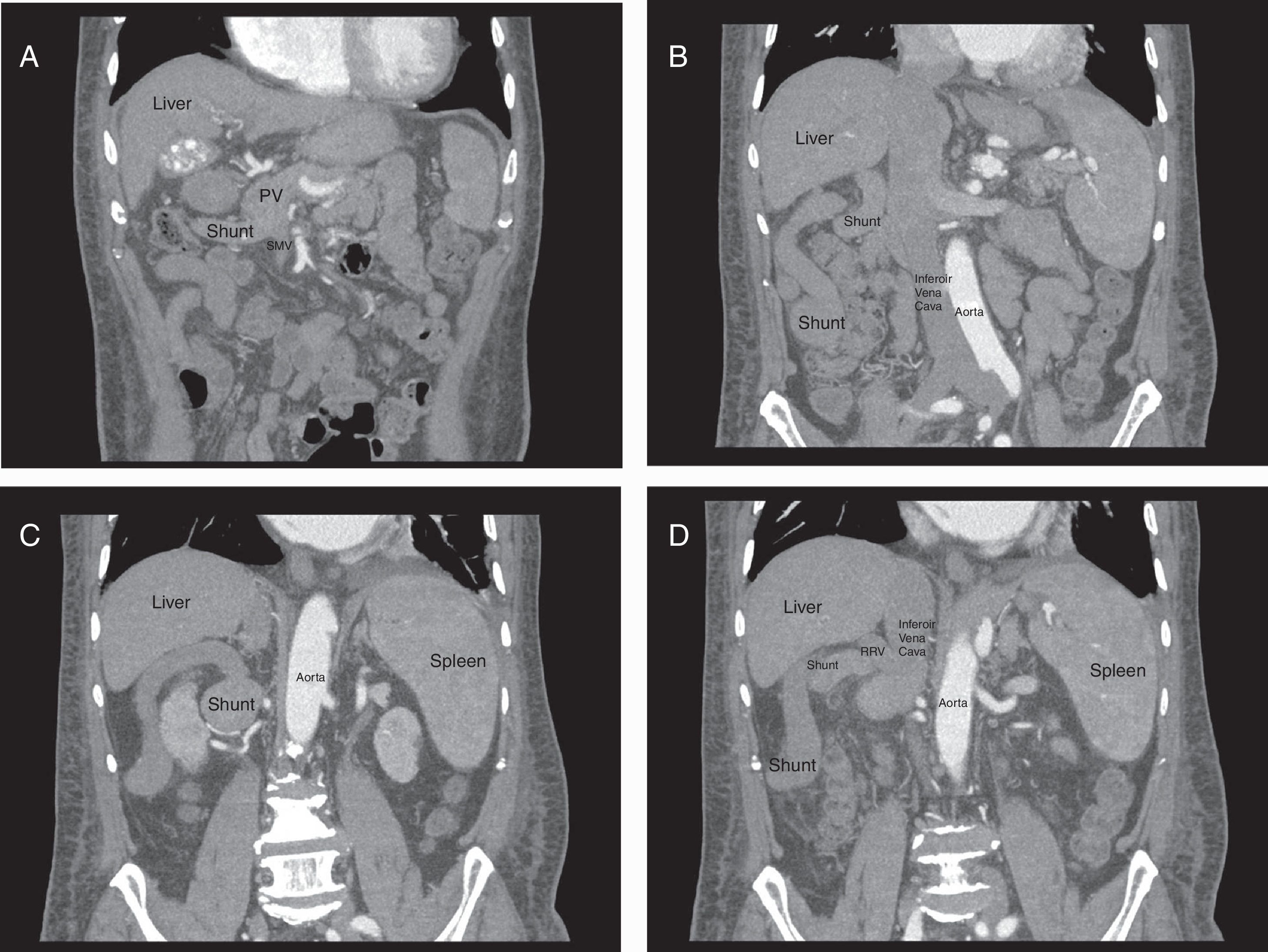
A 67-year-old white man presenting with Child C cirrhosis secondary to hemochromatosis and persistent encephalopathy was listed for LT. He was prioritized for LT due to persistent Grade 4 encephalopathy: his appealed Model for End Stage Liver Disease (MELD) score was 29. Preoperative Doppler-ultrasound showed absence of blood flow in the intrahepatic PV system, portoportal venous collateral network, hepatopetal flow into the PV with low velocity and cavernomatous transformation of PV. Abdominal angiotomography confirmed the presence of cavernomatous transformation of the PV, and identified a large spontaneous shunt between the SMV and the RRV (Fig. 1). The diameter of the SMV at the confluence level for formation of the PV was 1.4cm. The patient underwent LT by receiving a liver from a 17-year-old brain-dead deceased donor victim of trauma. The liver was preserved in IGL-1 storage solution. A large shunt between the SMV and the RRV was confirmed intraoperatively (Fig. 2). Neither PV thrombosis nor cavernomatous transformation of PV was detected intraoperatively. However, the distal segment of PV was atrophic and had a reduced flow. PV pressure was 22mmHg, and after shunt ligation PV pressure increased to 32mmHg. Recipient PV was shortened through removal of its atrophic distal segment. An end-to-end anastomosis between proximal (non-atrophic) segment of the recipient's PV and donor's PV was constructed.
Post-transplant, a bile leak occurred and demanded reoperation to convert biliary anastomosis to a Roux-en y hepaticojejunostomy. There were no vascular complications, and the patient was discharged home in good health.
Spontaneous portosystemic shunts are common findings in patients with PV thrombosis and/or cavernomatous transformation of the PV. Rarely, patients without PV thrombosis may develop large spontaneous portosystemic shunts secondary to portal hypertension. Those large spontaneous shunts usually communicate PV and left renal vein. In these cases, PV may present as atrophic due to a chronically low PV flow. We found only one prior report of a shunt between the SMV and the RRV.[3] This prior report only involved a radiologic image of the shunt. The case reported herein involves both the radiologic findings and also the operative approach with images.
Angio CT scan is mandatory to all LT candidates in order to rule out the presence of abnormalities in PV flow including thrombosis, atrophy and cavernomatous transformation of the PV. Intraoperatively, measurement of PV flow is mandatory if large shunts are identified. All spontaneous large shunts should be ligated during LT. After ligation of large shunts, measurement of the flow and the pressure of PV should be performed. As for PV pressure measurements (even in the absence of a flow monitor), before the creation of the PV anastomosis, an arterial line may be inserted inside the PV stump. This line is connected to a common pressure transducer, the pressure readings being expressed in the anesthesia monitor.
Ligation of the shunt (s) should enable an increase in the PV flow and pressure, as reported herein. In the absence of PV thrombosis, whenever shunt ligation does not lead to a satisfactory increase in flow and pressure of the PV, there might be additional shunts to be ligated. Alternatively, especially in pediatric patients, PV may be completely atrophic, and thus portal flow may not react adequately to shunt ligation. In such instances, the creation of a jump graft between anatomically normal SMV and PV of the liver graft may be necessary. Thus, preoperative and also intraoperative study of PV and the shunts is essential to identify spontaneous PV shunts, enabling successful LT.
FundingThis study was funded by FIPE of Hospital de Clinicas de Porto Alegre.
Conflicts of interestThe authors declare no conflicts of interest.