Elevated enzyme activities in plasma may sometimes be due to the presence of macroenzymes.1,2 Macroenzymes are high molecular mass complexes of plasma enzymes with immunoglobulins (IgG, IgA or IgM) or other plasma components with reduced plasma clearance and prolonged half life, resulting in elevated serum activities due to the “trapping” of the enzymes in serum.3 These results may thus be erroneously considered as pathologic. Macro-aspartate aminotransferase (macro-AST) has rarely been reported as a benign cause for increased plasma aspartate aminotransferase (ASAT) activities.4,5-8
Case ReportWe report here the case of a 32 year old female patient with an isolated chronic asymptomatic elevation of the plasma ASAT. Our patient had no relevant past medical history and no family history of liver pathologies. Anamnestically, abnormal liver function tests with a ten fold elevation of the tran-saminases were measured when she was 14, at the time of an acute Epstein Barr Virus (EBV) infection. No follow-up controls of the liver function tests after the healing from the EBV infection are available.
The first observation of an isolated elevation of the ASAT (400 IU/L) in this patient was made 11 years later’ at the time of a systematic medical check. Since then, several and regular controls of the liver function tests, over 7 years, confirmed the asymptomatic isolated elevation of the ASAT with values varying between 120 and 500 IU/L. During this period, all additional explorations failed to identify the cause of the ASAT elevation. The repeated several viral serologies for hepatitis A, hepatitis B and hepatitis C were always unremarkable. Iron ferritin, transferrin, anti-nuclear antibodies, anti-mitochondrial antibodies, anti-gliadin antibodies, anti-transglutaminase antibodies, coeruloplasmine, TSH and abdominal sonographic imaging were unable to identify any liver disease as a possible cause of the ASAT abnormality. During this period our patient was not taking any medication except an oral contraception with an oestroprogestative pill she has been taking since the age of 16. Stopping the oestro-progestative contraception for 1 year in 2004 didn’t lead to any normalisation of the ASAT values. The patient denied taking any herbal preparations or any other potentially liver toxic substances. So that a toxic or drug associated liver damage was also considered as rather unlikely. Before performing a liver biopsy and further investigations the patient was referred to our outpatient clinic.
At this point and considering the unremarkable findings, the negative physical examination, the normality of the other liver function tests and the chronicity of the condition, a macroenzyme was suspected and the ASAT activity was measured before and after the addition of protein-A-sepharose, according to the method described by N. de Jonge, et al.1 The decrease in our patient’s ASAT activity from 459 to 57 IU/L after the incubation with pro-tein-A-sepharose whereas no significant changes were measured in the ASAT activity of a healthy control (24 vs. 30 IU/L) treated by the same method comforted the diagnosis of macro-AST.
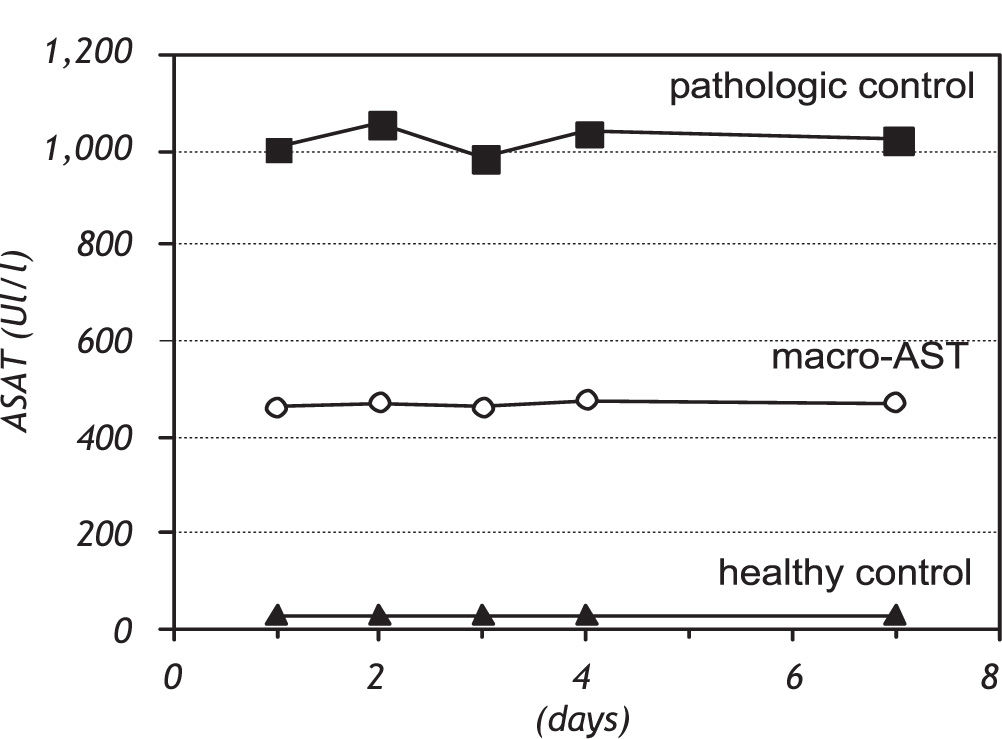
Furthermore, a blood sample was collected on heparin tube, and the ASAT activity was measured in the central laboratory of our university hospital and plasma was stored at 4°C during one week for repeated measurements.
DiscussionMacroenzymes were first reported by Wilding et al. in 1964.3 The prevalence of macro-AST is not clearly defined but seems to be less frequent than with other enzymes like amylase, or creatine kinase. Their presence doesn’t appear to be pathological in itself but macro-AST have been associated in some case-reports with several pathological conditions (malignant liver disease, acute and chronic hepatitis, autoimmune hepatitis, immunoblastic lymphadenopathy, gastrointestinal malignancy, colitis, infections, unspecified autoimmune diseases, etc…).2 Our patient was asymptomatic and the different investigations didn’t show any of these pathological conditions. However, in this case, the role of the healed EBV infection as a trigger for the development of the macro-AST might be a matter of debate.7
The pathogenesis is still unknown but immune reactions or a dysregulation of the immune tolerance seem to be involved in the building of these enzyme-immunoglobulin complexes as this condition has often been associated to autoimmune diseases.9
Several laboratory techniques were proposed for diagnosing macro-AST.1,4,6 Some require highly specialized chromatography or electrophoresis. Other have more simple procedures based on immunoprecipitation of the macroenzymes by polyethylene glycol (PEG) for example, with some reports of false positive results10 or by protein-A-sepharose precipitation1 as in our patient.
A simpler method was described by Davidson et al.4 In a patient with macro-AST, these authors reported a more than 90% loss of the ASAT activity (in plasma and serum) after 6 days of refrigerated storage (4°C). Castiella et al.,6 reported also a significant decrease in the ASAT activity when the samples were stored at 2 to 8°C with less than 35% of the ASAT activity remaining after 48 hours.
Our data did not confirm the progressive loss of ASAT activity in the course of time, after re-measurement and under the same previously described conditions. In our patient with macro-AST the ASAT activity remained at the same level, when stored at 4°C during 1 week. We also obtained a similar stability in the results of the re-measurements of our pathologic control (patient with high ASAT activity due to hepatitis C) as well as our healthy control (with ASAT activity within the normal laboratory range)(Figure 1).
This discrepancy between the data of the literature and our results may be due to the heterogeneity of the macro-AST: complexes with different sorts of immunoglobulins (IgA, IgG and/or IgM) or other proteins and plasma components.3 These differences in the structures of the complexes and probably also in their physico-chemical properties may thus explain their different behaviour and their different ability to precipitate spontaneously when stored at 4°C. The use of such methods should thus be avoided in the daily clinical practice for diagnosing macro-AST before a proper validation of this simple and attractive technique becomes available.
ConclusionPhysicians should be aware of macro-AST as a cause of plasma ASAT activity elevation. The long follow-up period in our patient (at least 7 years) underlines the benignity of the condition especially that all the further explorations were unremarkable towards liver pathologies or other associated diseases. However new, simple, attractive but not validated diagnostic methods should be used with caution as the heterogeneity of the macro-AST group could possibly account for a large variability in their results.