We present the first case of hepatic actinomycosis requiring both medical and surgical intervention due to liver dissemination from a primary colonic abscess. A 52-year-old white male had a computerised (CT) abdominal scan following an episode of collapse and was found to have peri-colonic and hepatic abscesses. Prior to this episode, he suffered with a two month history of fever, unexplained weight loss, and anaemia suggesting possible malignancy. He was treated with both radiological and surgical drainage of the abscesses, alongside the antibiotic cover and underwent an anterior colonic resection with primary anastomosis. There have been no previous reports of an actinomycotic liver abscess complicating colonic diverticular abscess. A multi-team approach is recommended when disseminated actinomycotic infection is encountered.
Actinomycosis is most frequently caused by Actinomyces israelii and usually involves the oral cavity, the digestive tract, or the respiratory system. Actinomyces genus is a gram positive, anaerobic or facultatively anaerobic micro-organism which belongs to the actinobacteria class and typically affects males between 20 and 60 years of age.1 Chronic Actinomycosis is characterised by granulomatous inflammation, contiguous spread and the formation of abscesses and sinus tract fistulae. Treatment is usually with antibiotics that offer good gram positive and anaerobic cover; however, occasionally surgical intervention is needed if a collection forms.
Case HistoryA 52-year-old male was referred to our hospital following an episode of collapse.
He had previously been treated by his GP for night sweats. On admission he was tachycardic, hypotensive and had a haemoglobin level of 6.6g/ dL. He was complaining of fever, drenching night sweats and extreme fatigue. Over a period of two months he had lost >12 kg in weight. There was no recent history of gastrointestinal blood loss, abdominal or chest pain, bruising, vomiting or any change of his bowel habit. There was no evidence of cervical lymphadenopathy or jaundice. He had a tender and palpable liver edge 1-2 cm below the costal margin.
Blood investigations showed anaemia and a cholestatic liver function tests profile (ALP 386 IU/L, Gamma-GT 189 IU/L, aminotransferases and bilirubin within normal range). Inflammatory markers were raised (WCC 25.3 x109/L, Neutrophils 23.6 x109/L) but his renal function, and platelets were within normal range.
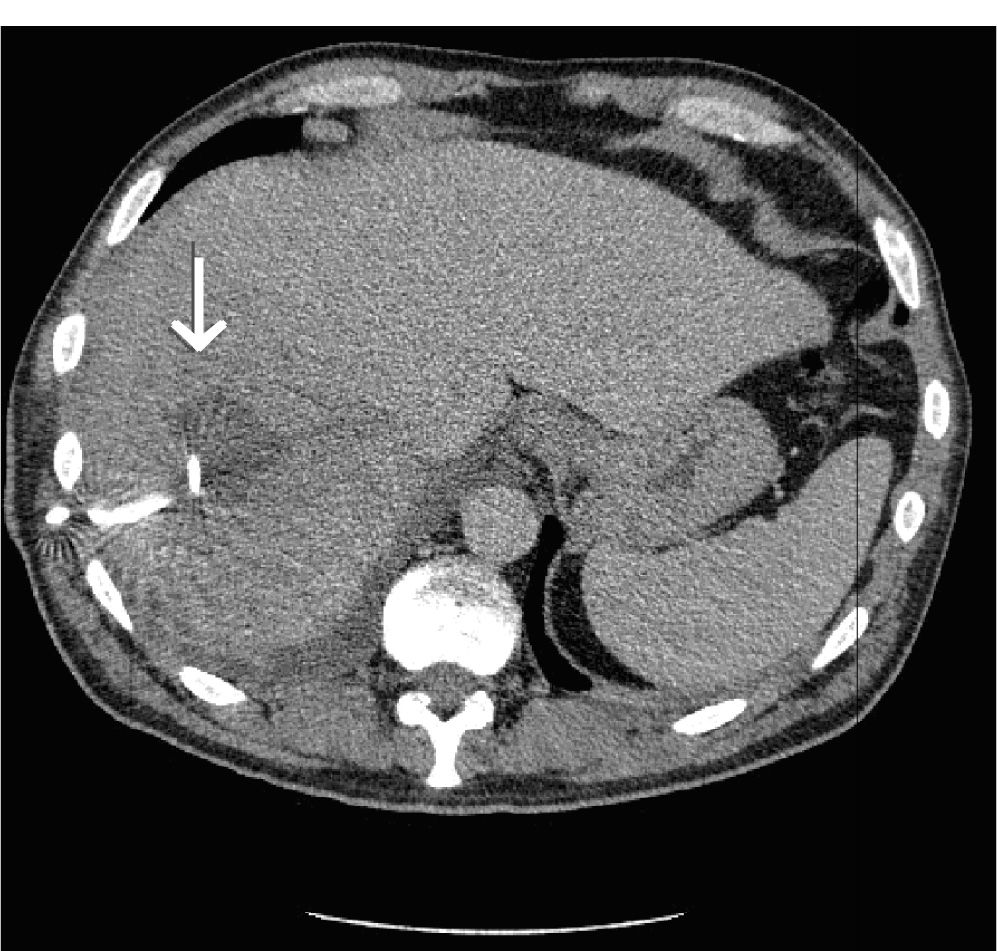
He was resuscitated with intravenous fluids and blood transfusion. Working on a diagnosis of haematological malignancy, a bone marrow aspirate and biopsy were performed; there were both normal. An abdominal CT scan though showed a 5.7cm in diameter hypodense lesion in the right lobe of the liver, suggestive of a liver abscess (Figure 1). An area of thickening was noted in the pelvis, together with a right side basal effusion and a dilated left ureter.
The hepatic abscess was aspirated and a drain was inserted under radiological guidance. Culture of this sample grew actinomycosis. The patient was started on intravenous antibiotics; teicoplanin, me-ropenem and metronidazole.
A repeat CT scan was performed eleven days later and showed that the liver abscess had decreased in size to 4 x 3cm (Figure 2). There was though marked left hydronephrosis. A paracolic diverticular abscess was also noted, which was believed to have been the primary source of the liver abscess as well as the cause of ureteric obstruction (Figure 3). Microbiology had confirmed the presence of actinomycosis within the abscess that had been drained.
The patient was referred for an anterior colonic resection with primary anastamosis. The liver abscess was confirmed to be successfully drained during laparotomy. A stent was also placed within the left ureter at the time of the operation. Histology of the resected sigmoid colon confirmed the presence of active diverticular disease
The patient remained well post operatively and was discharged a week later on a six-month course of amoxicillin.
DiscussionActinomycotic liver abscess is commonly associated with non-specific clinical and laboratory signs of infection. Imaging usually reveals a space occupying lesion, suggestive of either a hepatic tumour or inflammatory pseudotumour. Definitive diagnosis is by histopathology tests on samples obtained under radiological guidance.
Actinomycotic infection of the liver can either be due to primary infection or secondary to disseminated disease. Disseminated hepatic actinomycotic infection has been found to primarily originate from the abdominal cavity.2,3 Previous reports pointed that intrauterine device use in women is associated with actinomycotic infection within the pelvis, usually resulting in the formation of a collection or pseudotumour. Confirmation of the presence of actinomycosis is usually attained following cultures of either the pelvic or hepatic collection.4-7
Actinomycotic liver abscess secondary to a diverticular primary abscess is a rarity. Rarer associations include the use of pancreatic stents in the setting of long standing pancreatitis, which was suggested to have aided seeding of the bacteria into the liver.8 A case of abdomino-pelvic infection secondary to appendicetomy as also been described in literature, however, the infection remained within the bowel and did not spread to the liver.9
Brown et al. reported a case of actinomycosis presenting solely as a pelvic mass resulting in obstruction of the urinary system. The resulting hydronephrosis and hydro-ureter were self-limiting and ureteric obstruction resolved after 9 months following treatment.10
Samuel et al. described a case of actinomycosis complicating chronic sigmoid diverticulitis. Intramural colonic infection resulted in stricture formation and obstruction, however the infection was again localised to the colon. No hepatic seeding had occurred.11
Hepatic actinomycosis can be treated in several ways. Our review of cases thus far have shown that radiological/surgical drainage and antibiotics are sufficient to treat the infection.9 In only two case-series did patients have to undergo radical surgery, resulting in hepatic lobectomy.3,12 Pelvic collections are more likely to require surgical intervention to assist in the eradication of the primary infection.
This is the first case of hepatic actinomycosis resulting from a disseminated primary colonic diverticular collection. A combination of surgery, radiological drainage, and antibiotics proved to be beneficial in managing this rare presentation. We would therefore advocate that a multi-team approach would be ideal in any further encounters with disseminated actinomycotic infection.