Mucinous cystic neoplasm of the liver (MCN-L) and intraductal papillary mucinous neoplasm of the bile duct (IPMN-B) are diagnoses that were classified by the World Health Organization in 2010 as mucin-producing bile duct tumors of the hepatobiliary system. The preoperative differential diagnosis between these two entities is difficult; the presence of a communication with the bile duct is usually considered as a typical sign of IPMN-B. However, the presence of an ovarian-like stroma (OLS) has been established to define the diagnosis of MCN-L. We present the case of a 33-year-old woman with a rapid progression of a cystic tumor of the liver. In 2 years, the lesion increased from 27 to 64 mm and a dilation of the left hepatic duct appeared. Percutaneous transhepatic drainage with a biopsy was performed. No malignant cells were found on biopsy. Because of the rapid progression of the cystic tumor and unclear malignant potential, left hemihepatectomy was performed. Even though tumor masses were present in the biliary duct, on the basis of the presence of OLS, histology finally confirmed MCN-L with intermediate-grade intraepithelial dysplasia to high-grade intraepithelial dysplasia. The patient is currently under oncologic follow-up with no signs of recurrence of the disease. We present a rare case where MCN-L caused a dilation of the left hepatic duct, a sign that is usually a characteristic of IPMN-B.
In 2010, the World Health Organization (WHO) classified mucin-producing bile duct tumors of the liver into two distinct entities: mucinous cystic neoplasm of the liver (MCN-L) and intraductal papillary mucinous neoplasm of the bile duct (IPMN-B).1,2
MCN-L, or the hepatic mucinous cystic neoplasm, has previously been known as biliary cystadenoma or cystadenocarcinoma.3 Terms such as biliary papillomatosis, mucin-hypersecreting cholangiocarcinoma or mucin-hypersecreting bile duct tumor are currently referred to as IPMN-B4 or the biliary intraductal papillary mucinous neoplasm.
MCN-L is a rare entity that constitutes less than 5% of all cystic liver lesions.2,3,5,6 They are mostly located in the left lobe of the liver (in approximately 75% of cases).1,7 MCN-L predominantly appears in females (incidence rate varies from 85% to 100% according to previous studies).1,4,7 MCN-L is clearly histologically defined as a cystforming epithelial neoplasm composed of mucin-producing epithelium associated with ovarian-like stroma (OLS).2 MCN-L is histologically graded as low-, intermediate-, and high-grade intraepithelial dysplasia; carcinoma in situ; or an associated invasive carcinoma.1,2,8
IPMN-B is recognized as a biliary counterpart to papillary intraductal mucinous neoplasm of the pancreas (IPMN-P). Similar to IPMN-P, according to the type of tumor-cells, IPMN-B is classified into 4 subtypes: gastric type, intestinal type, pancreaticobiliary type, and oncotic type.1,4,10 IPNM-B has typical characteristics of the absence of OLS and the presence of communication with a bile duct,3,4,7,9 and it may produce a large amount of mucin resulting in an extensive dilation of the bile ducts.5 IPMN-B is histologically described as a mucinous and papillary neoplasm, with a clear origin in the biliary epithelium and a solitary or diffuse intraductal growth.9
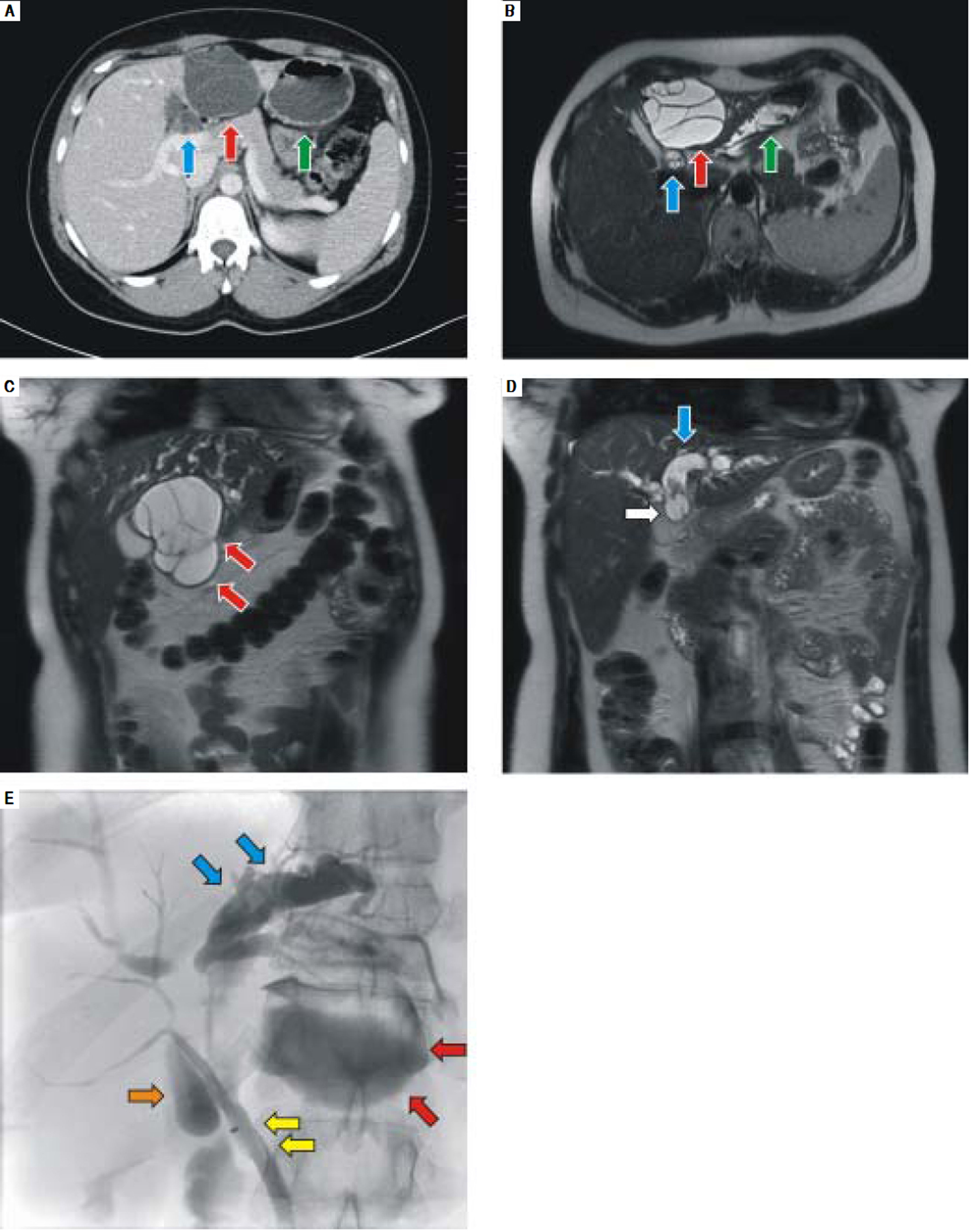
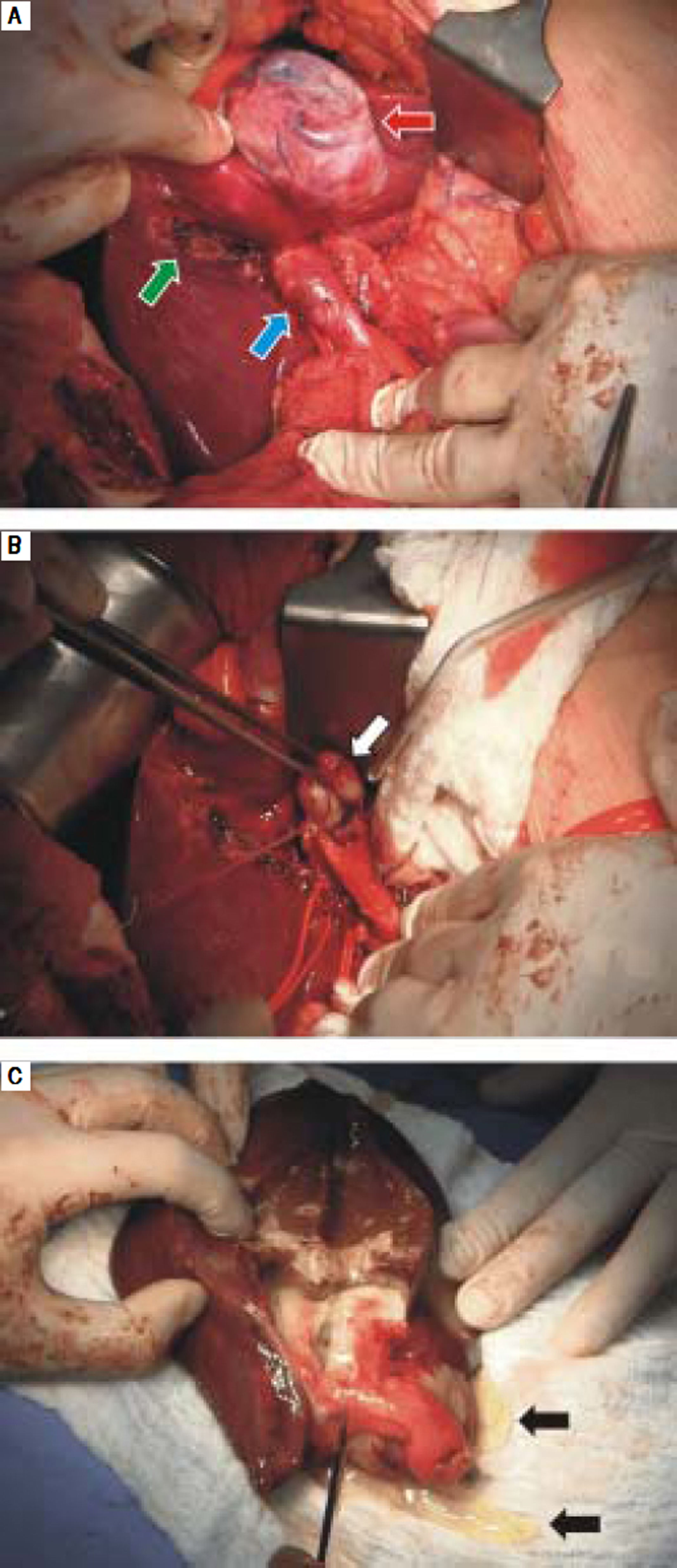
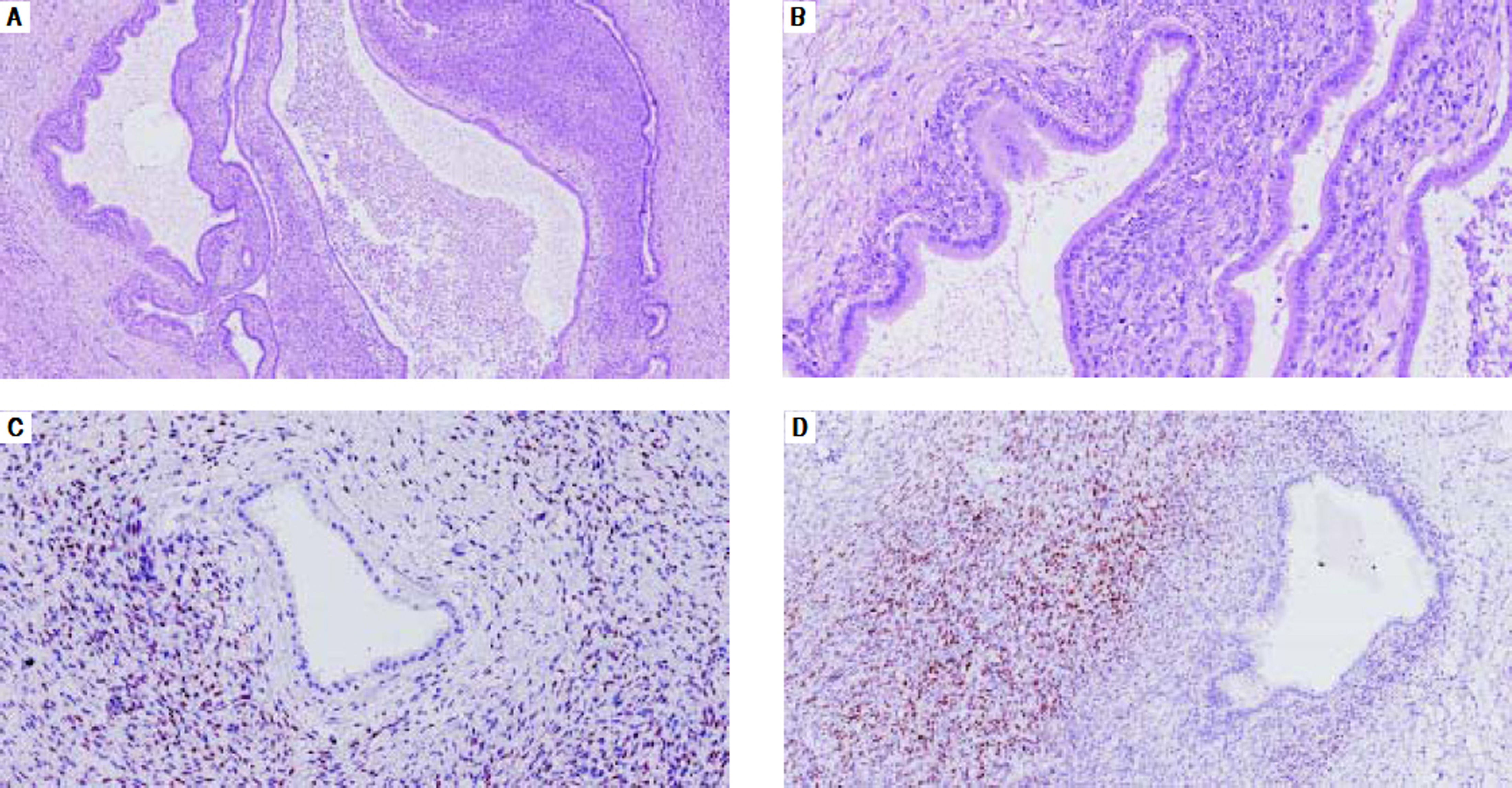
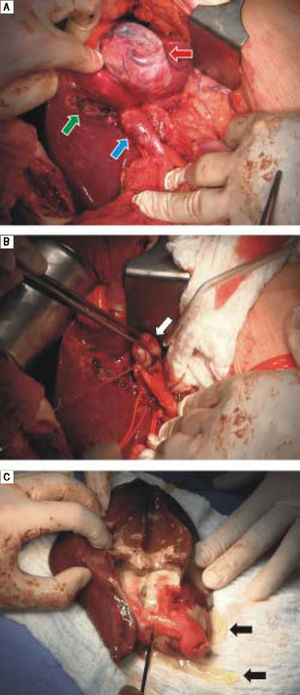
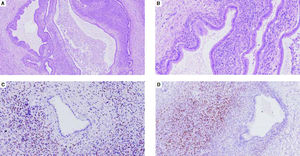
Case ReportA 33-year-old woman was diagnosed to have slight elevation in the level of liver enzymes and a benign-like cystic lesion of 27 mm in size in the left liver lobe. After 2 years, the control CT (Figure 1A) and MRI (Figure 1B, 1C, 1D) confirmed a rapid progression of the multilocular cyst to 64 mm in size and a dilation of the left hepatic duct. An insignificant elevation of CA 19-9 (103 kU/l) was detected; other tumor markers were within the normal limits. Both hepatitis B surface antigen and hepatitis C virus antibody tests were negative. The patient also had a negative alcohol consumption history. Percutaneous transhepatic drainage with biopsy was performed (Figure 1E). The biopsy did not prove the presence of any malignant cells; however, because of a rapid progression of the lesion, the malignant potential of the lesion could not be excluded, and a decision to perform surgery was made. A cystic tumor of the liver, situated in segment 4, with its appearance slightly mimicking the gallbladder and a dilated left extrahepatic bile duct was present (Figure 2A). Tumor masses that caused this dilation were spread up to the left extrahepatic bile duct (Figure 2B). Left hemihepatectomy, resection of the left bile duct, and cholecystectomy were performed. The specimen after resection is shown in figure 2C. The patient recovered without any complications and was dismissed on the 12th day after the surgery. A definitive histology (Figure 3A-3D) confirmed a mucinous cystic neoplasm of the liver with intermediate-grade intraepithelial dysplasia to high-grade intraepithelial dysplasia, ovarian-like stroma cells, with negative distal resection margin of the bile duct (Figure 3A-3D). The patient did not receive any further oncologic therapy. The control CT scan 6 months after the surgery did not reveal any signs of recurrence of the disease and another control follow-up was set at a one-year interval.
CT, MRI and cholangiography images. A. CT (contrast enhanced, transversal scan) and B. MRI (T2-weighted, transversal scan) -Cystoid multilocular formation in left hepatic lobe S4 (red arrow), with a dilation of the left intrahepatic bile ducts (blue arrow), in close proximity to the stomach (green arrow). C,D. MRI (T2-weighted, coronal scan) showing the same multilocular formation in left hepatic lobe S4 (red arrows), with a dilation of the left intrahepatic bile ducts (blue arrow) and intraluminal tumor masses (white arrow). E. Percutaneous transhepatic cholangiography and drainage - dilation of the left intrahepatic bile ducts (blue arrows), with irregular stenosis centrally and narrow common bile duct (yellow arrows); contrast is also visible in the cystoid formation (red arrows) and the gallbladder (orange arrow).
A. Perioperative image showing a cystic lesion of the liver in S4 (red arrow), slightly mimicking the gallbladder in its appearance. Gallbladder fossa after cholecystectomy (green arrow). Dilation of the left hepatic bile duct caused by tumor masses (blue arrow). B. View after the incision of the bile duct: prolapse of the tumor masses to the left hepatic bile duct (white arrow). C. Specimen after incision of the cyst and flowing mucin (black arrows).
A,BB. Cyst is lined by cuboidal columnar epithelium with low-grade dysplasia. The epithelium shows mucin secretion and lies on an OLS (A. HE staining, 50x, B. HE staining, 200x). C,D. The OLS is immunoreactive for progesterone and estrogen receptors (C. Estrogen receptor staining, x200, D. Progesterone receptor staining, x100).
The preoperative differential diagnosis between MCN-L and IPMN-B is challenging. Although there are generally recognized signs such as no bile duct communication, no bile duct dilation or multilocular shape in MCN-L, it seems that these generally established signs may not always be decisive to define the diagnosis. However, the presence of OLS in the histopathological section has been established by the WHO as a diagnostic criterion of MCN-L.
MCN-L and IPMN-B share some common characteristics such as rare incidence or mucin production. Still, there are some clinicopathological features that are more typical of each neoplasm. MCN-L predominantly occurs in females. Kubota, et al.1 published a study on the clinicopathological features of mucin-producing tumors of the bile duct, and all patients with MCN-L in this study were females. Zen, et al.7 published similar results with all the patients being females in 2011, while in his later study in 2014, the female gender constituted 93% of all patients diagnosed with MCN-L.11 Our present patient was also a female.
The primary MCN-L location is in the left liver lobe, mostly in S4,1,7,10 although the reason for this tendency remains unknown. In radiological findings, MCN-L showed mostly as multilocular cysts with septation, in contrast to IPMN-B that is characterized by a multicystic appearance.7 In our case, the patient had a multilocular cyst in the left lobe.
A dilation of the bile duct, the presence of intraluminal masses1,5,9 and the presence of intraductal nodules1,7,11 are radiologic signs for the diagnosis of IPMN-B. However, in 2015, Takano, et al.10 published two cases of MCN-L that showed the presence of prolapsed tumor masses in the left hepatic duct and common bile duct which caused their dilation. Our patient also had dilation of the bile duct, and the final diagnosis based on histology was MCN-L because of OLS. This amplifies a speculation that dilation and communication with the bile duct may not be a typical sign of IPMN-B and can even occur in the case of MCN-L.
In 2014, Budzynska, et al.5 published a unique case of a simultaneous MCN-L and IPMN-B in a single patient. In this case, a dilation of the biliary tract was also present. The tumor from the main hepatic duct was histologically confirmed as IPMN-B and the intrahepatic tumor was diagnosed as MCN-L on the basis of the presence of OLS (OLS was confirmed by positive immunostaining for progesterone and estrogen receptors).
MCN-L can be difficult to differentiate from hepatic simple cysts. Generally, a large cyst (> 100 mm) at initial presentation, an increase in size during follow-up, and manifestation of symptoms are indications for resection.3,11 Surgery is the first choice of treatment for patients with IPMN-B if no distant metastases are present.9 Patients with IPMN-B mostly underwent surgery on the basis of radiological findings suggestive of cystic neoplasm, intraductal tumor or cholangiocarcinoma.11 IPMN-B is known to manifest as a radiologically detectable nodule in the bile duct, which is an indication for surgery.11 The watch-and-wait strategy is not an option for IPNM-B because of high probability of malignancy.11
A complete resection of IPMN-B or MCN-L has a good prognosis,1 although a prognosis of IPMN-B seems to be slightly worse than in the case of MCN-L.1,4 The 5-year survival rate for patients with MCN-L and IPMN-B was 100% and 82% as published by Li, et al.4 in 2009. Quite similar results were published by Kubota, et al.1 in 2014, where in the 5-year survival rate for patients with MCN-L and IPMN-B was 100% and 84%, respectively. Wang, et al.9 also reported in his group of 19 patients with IPMN-B a good survival rate after a complete resection of the tumor. Our patient, after a complete resection (negative margins of the liver and the bile duct) and the final diagnosis of MCN-L, is radically cured with a good prognosis. An oncologic follow-up was initiated, with the first radiologic control 6 months after surgery and then subsequent follow-ups every 12 months.
ConclusionWe present a case in which MCN-L causes a dilation of the left hepatic duct and communicates with the bile duct, which are signs usually typical for an IPMN-B.
However, current publications as well as our present case support the argument that a dilation of the hepatic duct and a communication with the bile duct (intraductal spreading) may not always be present in the case of IPMN-B, but may also occur in the case of MCN-L.
Abbreviations- •
IPMN-B: intraductal papillary mucinous neoplasm of the bile duct.
- •
IPMN-P: intraductal papillary mucinous neoplasm of the pancreas.
- •
MCN-L: mucinous cystic neoplasm of the liver.
- •
OLS: ovarian-like stroma.
- •
WHO: World Health Organization.
Lumir Kunovsky: writing, main author, conception and design of the work, literature search. Zdenek Kala: consultant, text editor, conception and design of the work, firures. Roman Svaton: consultant, text editor, literature search. Petr Moravcik. consultant, literature search. Jan Mazanec: literature search, figures. Jakub Husty: literature search, figures. Vladimir Prochazka: consultant, text editor, conception and design of the work, literature search.
All authors made a critical revision and gave their final approval for publishing.
Grants or Financial SupportNo grants or financial support were provided.
Conflict of InterestAll authors declare no conflicts of interest in relation to this article.