Well established complications of essential thrombocythemia are multiple thrombohemorrhagic phenomena in various abdominal organs. We describe the case of a 22 year old man with essential thrombocythemia and thrombosis of the mesenteric and splenic veins as well as cavernomatous transformation of the portal vein. The patient also had a splenic infarction and a subphrenic hematoma. Additionally, he developed signs and symptoms of acute cholecystitis which in turn led to an open cholecystectomy. The gallbladder had a markedly thickened wall due to multiple recent and recanalized thrombi predominantly in subserosal veins. Only a few arteries were occluded by thrombi. A marked vascular proliferation in the subserosal connective tissue mimicking a hemangioma was most likely the result of collateral circulation. There was also a mild acute and chronic inflammatory infiltrate and edema in the lamina propria of the gallbladder. Hyperplasia of interstitial cells of Cajal in the lamina propria and between smooth muscle cells and proliferation of nerve trunks in the subserosal connective tissue adjacent to the thrombosed veins and arteries was also noted. To our knowledge this unique gallbladder thrombotic complication of essential thrombocythemia has not been previously reported.
Essential thrombocythemia (ET) is a rare myeloproliferative neoplasm that involves primarily the megakacaryocytic lineage.1 It is characterized by ex-cessive platelet production, sustained thrombocytosis in the peripheral blood and recurrent thrombohemorragic phenomena in arteries and veins of various tissues and organs.2–4 Thromboses of mesenteric, splenic and portal veins, with or without cavernomatous transformation of the portal vein are well documented complications of ET.3–9 However, the development of thrombosis of large subserosal veins and arteries in the wall of the gallbladder causing acute cholecystitis has not been recorded to date.
We describe here the case of a 22 year old man who presented with signs and symptoms of acute cholecystitis caused by thrombosis of subserosal gallbladder veins and arteries. The patient had a history of ET of 5 years duration complicated with thrombosis of mesenteric and splenic veins, cavernomatous transformation of the portal vein, a splenic infarction and a subphrenic hematoma.
Clinical HistoryA 22 year old man presented with intense right upper quadrant abdominal pain of several hours duration and a 5 year history of ET with splenic vein thrombosis followed by splenic infarction, a subphrenic hematoma and splenectomy. Additionally, the patient experienced a minor cerebrovascular accident from which he recovered fully. He also had a history of left brachial monoparesis, paresthesias, frontal headache and right amaurosis. On physical examination there was intense pain on palpation of the right hypochondrium and right upper quadrant abdominal pain.
An abdominal ultrasound and angiography revealed an enlarged gallbladder and cavernomatous transformation of the portal vein. Laboratory data showed normocytic hypochromic anemia (Hb 11.6 g/dL; MCV 83.8 mm, MCHC 27.1 g/dL), leukocytosis (19,000/mm) and thrombocytosis (2,060,000/mm). Serum glucose and aminotransferases were within normal values.
The bone marrow karyotype was normal. The fluorescent in situ hybridization did not show t (9; 22). A JAK2 V617F mutation test is not available in our institution and therefore, was not performed in the patient. A bone marrow biopsy showed a hypercellular marrow due to a marked proliferation of megakaryocytes most of which were large or giant with abundant eosinophilic cytoplasm and lobulated or multilobulated nuclei. There was no increase in the number of erythroid precursors, reticulin or collagen fibers. A few days after admission to the hospital, the patient underwent an open cholecystectomy.
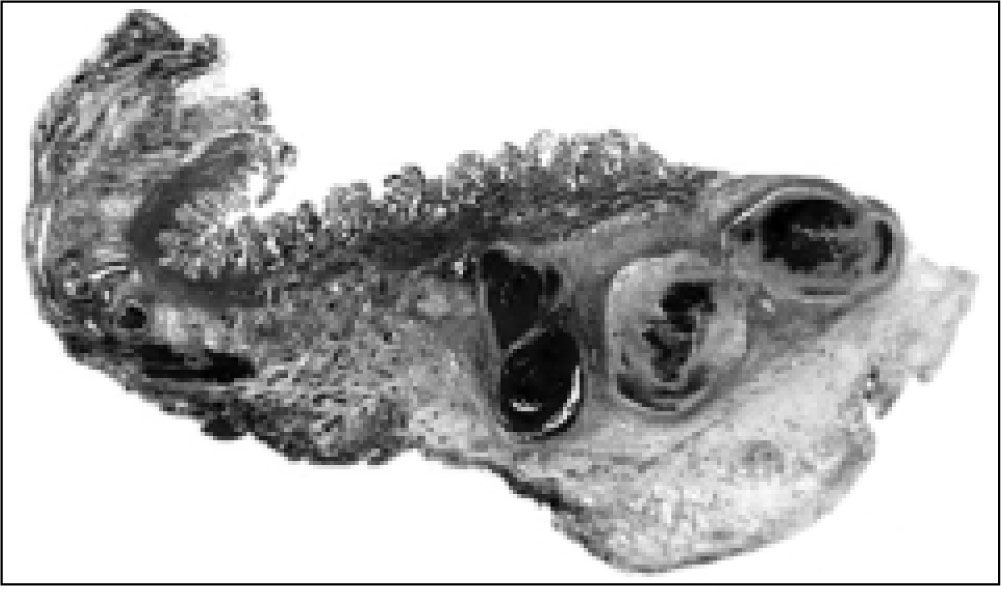
Gross and microscopic pathologyThe gallbladder showed a markedly thickened wall but no gallstones (Figures 1 and 2). Grossly, the mucosa was edematous but otherwise appeared normal. However, on microscopic examination most of the mucosal folds had an expanded lamina propria by edema, a mild predominantly acute inflammatory infiltrate and numerous small blood vessels, some with recanalized thrombi (Figures 3 and 4).
The subserosa was expanded and contained numerous medium sized and large veins with recent and old recanalized thrombi (Figures 5, 6 and 7). Only a few arteries were occluded by recent thrombi. There was also marked proliferation of small and medium sized blood vessels mimicking a hemangioma (Figure 8). Likewise, numerous nerve trunks adjacent to the veins and arteries and hyperplasia of interstitial cells of Cajal between smooth muscle cells and in the lamina propria were also present (Figure 9).
Thrombohemorrhagic phenomena are relatively common complications of ET.2–9 Mesenteric, splenic and portal vein thrombosis with or without cavernomatous transformation have been well documented in association with ET.3–4 However, to our knowledge, large vein and arterial thrombosis in the subserosa of the gallbladder causing acute cholecystitis, as in our patient, has not been previously reported.
The marked proliferation of blood vessels in the subserosa mimicking a hemangioma10 most likely resulted from collateral circulation, a compensatory mechanism to minimize tissue damage due to ischemia, which might have been caused by blockage of venous and arterial circulation. Likewise, the edema of the lamina propria and the mild acute inflammatory infiltrate was also the result of the vein thrombosis. In addition to the newly formed blood vessels in the subserosa, the open cholecystectomy performed soon after the appearance of symptoms of acute cholecystitis contributed to the lack of necrosis of the gallbladder wall.
We have no explanation for the hyperplasia of interstitial cells of Cajal10,11 and the proliferation of nerve trunks, a reactive change that has been docu-mented in inflammatory conditions of the gallbladder and extrahepatic bile ducts.12 Although characteristic, venous and arterial thromboses in the wall of the gallbladder are not specific of ET; they have also been reported in the catastrophic antiphospholipid syndrome.13 Acalculous cholecystitis and arterial thromboses due to vasculitis has been reported in patients with systemic lupus erythematosus and polyarteritis nodosa.14
Gangat, et al.6 reported a prevalence of 4% for abdominal vein thrombosis among 460 consecutive patients with ET. A possible risk factor for vein thrombosis in ET include elevated platelet counts. However, it has been recognized that vein thrombosis may occur at relatively low platelet counts. On the other hand, abdominal vein thrombosis has been identified as a risk factor for poor survival.6
The true incidence of ET is unknown. However, it has been estimated that the overall incidence rate varies from 0.6 to 2.5 per 100,000 person per year.7 The median age at diagnosis is 67 years with a female preponderance, which is in contrast with our patient. Of interest is that 52% of patients displayed no ET related symptoms and are diagnosed fortuitously by routine platelet count.
JAK2 is an obligatory kinase primarily for the proliferation and differentiation of erythroid cells and megakaryocytes.5 In recent years the JAK2 V617F mutation has been identified in patients with ET.15 This mutation was initially thought to be useful in the molecular diagnosis of ET. Unfortunately, it lacks specificity since it has also been detected in polycythemia vera and primary myelofibrosis.5,9,15 Moreover, only 50% of patients with ET have the mutation. Therefore, the diagnosis of ET should be based on clinicopathological features.
ConclusionAcute cholecystitis caused by recent and old thrombosis predominantly of large subserosal veins of the gallbladder should be added to the list of abdominal vein and arterial thrombotic phenomena which are relatively common complications of ET. The diagnosis of acute cholecystitis due to thrombosis of subserosal veins and arteries of the gallbladder should be suspected in patients with ET who develop intense right upper quadrant abdominal pain and the ultrasound reveals a thickened gallbladder wall but no gallstones. It is important to keep in mind that some patients with ET may have low platelet counts in the peripheral blood.