The small intestine is a unique organ providing dietary and reabsorbed biliary cholesterol to the body. However, the molecular mechanisms whereby cholesterol is absorbed have not yet been fully understood. Recent research suggests that the newly identified ATP-binding cassette (ABC) transporters ABCG5 and ABCG8 are apical cholesterol export pumps that promote partial efflux of cholesterol and nearly complete efflux of plant sterols from enterocytes into the intestinal lumen after their absorption. This provides an explanation why cholesterol absorption is a selective process in that plant sterols and other non-cholesterol sterols are absorbed poorly or not at all. Furthermore, a putative cholesterol import protein has been proposed, but remains uncharacterized. The identification of such a gene should yield new insights into the mechanisms that potentially regulate the influx of cholesterol across the apical brush border membrane of the enterocyte. Combination therapy using a novel and potent cholesterol absorption inhibitor (ezetimibe) and an HMG-CoA reductase inhibitor (statins) offers an efficacious new approach to the prevention and treatment of hypercholesterolemia.
ABC, ATP-binding cassette (transporter)
ACAT, acylCoA:cholesterol acyltransferase
Mdr2, multidrug resistance gene 2
SR-BI, scavenger receptor class B type I
UDCA, ursodeoxycholic acid.
IntroductionCholesterol homeostasis is maintained by balancing intestinal cholesterol absorption and endogenous cholesterol synthesis with excretion of biliary cholesterol and bile acids. Since elevated plasma cholesterol is an independent risk factor for coronary heart disease1 and biliary cholesterol hypersecretion is an important prerequisite for cholesterol cholelithiasis,2 considerable interest has been focused on identifying biochemical, physical-chemical, and genetic determinants of intestinal cholesterol absorption. Furthermore, understanding the sequential steps in intestinal cholesterol absorption may lead to novel approaches to the treatment of these diseases that affect millions in Westernized societies.
Physiological mechanisms of intestinal cholesterol absorption“Absorption of cholesterol” is most accurately defined as the transfer of intraluminal cholesterol into intestinal or thoracic duct lymph. “Uptake of cholesterol” refers to entry of cholesterol into intestinal absorptive cells. According to these definitions, cholesterol absorption is a multistep process that is regulated by multiple genes.3,4
There are three sources for intestinal cholesterol: the diet, the bile, and intestinal epithelial sloughing. The average daily intake of cholesterol in the Western diet is approximately 300-500 mg. Bile provides 800-1,200 mg of cholesterol per day to the intraluminal pool. The turnover of intestinal mucosal epithelium provides a third source of intraluminal cholesterol, and estimates of this contribution are 300 mg of cholesterol per day. Although the entire length of the small intestine has the capability to absorb cholesterol from the lumen, main sites of absorption are the duodenum and proximal jejunum.
Cholesterol absorption begins in the stomach when dietary constituents are mixed with lingual and gastric enzymes. The stomach also functions to regulate the delivery of gastric chyme to the duodenum, where it is mixed with bile and pancreatic juice. This process continues within the lumen of the small intestine. Hydrolytic enzymes secreted by the pancreas and bile salts of bile solubilize the hydrolytic end products of intraluminal fat digestion, 5,6 and a variable proportion of dietary cholesterol is esterified to fatty acids.
Some of the lipolytic products, including cholesterol, are only minimally soluble in aqueous systems and are dependent on the solubilizing properties of bile salt solutions. 7,8 Bile salts are biological amphipathic detergents which, when present above a critical micellar concentration, spontaneously form aggregates that are able to dissolve lipids.9,10 Cholesterol is only sparingly soluble in bile salt solutions, in contrast to phospholipid, monoacylglyceride and free fatty acid that are readily soluble. The addition of phospholipid or monoacylglyceride to bile salt solutions markedly increases the solubility of cholesterol.11 Bile salts together with ionized and nonionized fatty acids, monoacylglyceride, (lyso) phospholipid, and unesterified cholesterol form mixed micelles.12 Excess lipids not dissolved in the micellar phase form a separate oil phase within the intestinal lumen,5,6 and may be maintained as a stable emulsion by bile salt, phospholipid, monoacylglyceride, and ionized fatty acid. In addition, during lipolysis, a liquid crystalline phase composed of multilamellar products of lipid digestion forms at the surface of an emulsion droplet.13,14 The liquid crystalline phase provides an accessible source of phospholipid, monoacylglyceride, fatty acid, and cholesterol for the formation of mixed micelles in the presence of bile salt.
Cholesterol is absorbed by the small intestine solely as monomers. The unstirred water layer, a series of water lamellae at the interface between the bulk water phase of the lumen and the mucosal cell membrane, and the cell membrane form two barriers through which a cholesterol molecule in the bulk phase must pass in order to be absorbed. 15 Diffusion through the unstirred water layer is a relatively slow process for cholesterol that is nearly insoluble in a pure aqueous system. These micelles function as a concentrated reservoir and transport vehicle for cholesterol across the unstirred water layer toward the brush border of the small intestine to facilitate uptake of monomeric cholesterol by the enterocyte.13,14 Once monomers are taken up by enterocytes from the bile salt-rich reservoirs of intraluminal contents, the latter, in turn, are replete the intermicellar water with cholesterol monomers by their desorption from mixed micelles. As individual molecules of cholesterol are taken up into the cell membrane, other molecules of cholesterol move from the micelles into monomolecular solution and become available for uptake by the intestinal absorptive cells. However, it is not known how cholesterol within the intestinal lumen moves from the lumen into the intestinal absorptive cells, i.e., the entry of cholesterol molecules into cell membranes. We will further discuss it below (see Searching for intestinal cholesterol transporters).
During the absorption of cholesterol, there is little increase in the cholesterol content of the small intestine, indicating that cholesterol can be rapidly processed and exported from the mucosal cells and into the intestinal lymph.3,4 Studies have shown that following an intragastric dose of cholesterol mass and radioactivity, the transport of both in intestinal lymph rapidly increases and peaks after 6-8 hours.3,4 Upon entering the enterocytes, approximately half the cholesterol molecules move to the endoplasmic reticulum, where they are esterified by acyl-CoA:cholesterol acyltransferase (ACAT) before incorporation into nascent chylomicron particles. Of note is that essentially all cholesterol that moves from the intestinal lumen into the intestinal mucosal cells is unesterified; however, cholesterol secreted into intestinal lymph following a cholesterol-rich meal is approximately 70-80% esterified. The cholesterol esterifying activity of the mucosa may be an important regulator of cholesterol absorption, since re-esterification of absorbed free cholesterol within the mucosal cell would enhance the diffusion gradient for free cholesterol into the cell. Further, transmucosal transport of cholesterol is reduced in rats with inhibition of mucosal ACAT.16,17 It is found that ACAT1 is expressed in many tissues; however, the second enzyme, ACAT2 is localized specifically to liver and small intestine, and is most likely responsible for esterification of cholesterol absorbed from the intestine.18 Also, the inhibition of intestinal 3-hydroxy-3-methylglutaryl-CoA reductase by pharmacological intervention with “statins,” decreases intestinal cholesterol absorption in animals and humans.19-21 Moreover, cholesterol absorption is significantly inhibited in apolipoprotein B-48 deficient mice22 because of a failure in the assembly and/or secretion of chylomicrons, suggesting that this final step in the absorption process is critically important. Although intestinal microsomal triglyceride transfer protein and APOA1/ C3/A4 have been considered to possibly play some roles in the regulation of cholesterol absorption,23-25 their effects will need to be further studied.
Finally, cholesterol and bile salts that escape intestinal re-absorption and are excreted as fecal neutral and acidic sterol represent the major route for sterol elimination from the body.
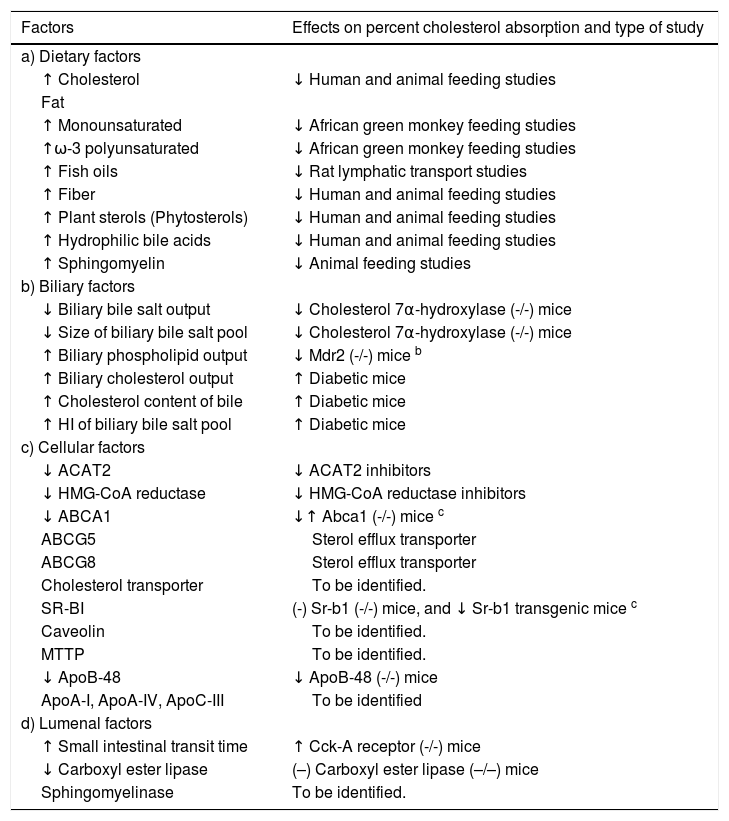
Factors influencing intestinal cholesterol absorption efficiencyAs cholesterol absorption is a multistep process, any factor that changes the transportation of cholesterol from the intestinal lumen to the lymph may influence intestinal cholesterol absorption efficiency. Table I summarizes dietary, including administered therapeutic agents, biliary, cellular, and luminal factors that could influence intestinal cholesterol absorption. Despite these findings, it remains poorly understood which step(s) in the absorption process are rate-limiting, as well as differ inherently among individuals in any population to explain variations in intestinal cholesterol absorption efficiency.
Possible factors influencing intestinal cholesterol absorption.
| Factors | Effects on percent cholesterol absorption and type of study |
|---|---|
| a) Dietary factors | |
| ↑ Cholesterol | ↓ Human and animal feeding studies |
| Fat | |
| ↑ Monounsaturated | ↓ African green monkey feeding studies |
| ↑ω-3 polyunsaturated | ↓ African green monkey feeding studies |
| ↑ Fish oils | ↓ Rat lymphatic transport studies |
| ↑ Fiber | ↓ Human and animal feeding studies |
| ↑ Plant sterols (Phytosterols) | ↓ Human and animal feeding studies |
| ↑ Hydrophilic bile acids | ↓ Human and animal feeding studies |
| ↑ Sphingomyelin | ↓ Animal feeding studies |
| b) Biliary factors | |
| ↓ Biliary bile salt output | ↓ Cholesterol 7α-hydroxylase (-/-) mice |
| ↓ Size of biliary bile salt pool | ↓ Cholesterol 7α-hydroxylase (-/-) mice |
| ↑ Biliary phospholipid output | ↓ Mdr2 (-/-) mice b |
| ↑ Biliary cholesterol output | ↑ Diabetic mice |
| ↑ Cholesterol content of bile | ↑ Diabetic mice |
| ↑ HI of biliary bile salt pool | ↑ Diabetic mice |
| c) Cellular factors | |
| ↓ ACAT2 | ↓ ACAT2 inhibitors |
| ↓ HMG-CoA reductase | ↓ HMG-CoA reductase inhibitors |
| ↓ ABCA1 | ↓↑ Abca1 (-/-) mice c |
| ABCG5 | Sterol efflux transporter |
| ABCG8 | Sterol efflux transporter |
| Cholesterol transporter | To be identified. |
| SR-BI | (-) Sr-b1 (-/-) mice, and ↓ Sr-b1 transgenic mice c |
| Caveolin | To be identified. |
| MTTP | To be identified. |
| ↓ ApoB-48 | ↓ ApoB-48 (-/-) mice |
| ApoA-I, ApoA-IV, ApoC-III | To be identified |
| d) Lumenal factors | |
| ↑ Small intestinal transit time | ↑ Cck-A receptor (-/-) mice |
| ↓ Carboxyl ester lipase | (–) Carboxyl ester lipase (–/–) mice |
| Sphingomyelinase | To be identified. |
a ↑ represents decrease, ↓ increase, and (-) no effect.
b Abbreviations: Mdr2, multidrug resistance gene 2; HI, hydrophobicity index; ACAT2, acyl-CoA:cholesterol acyltransferase, isoform 2; HMG, 3-hydroxy-3-methyglutaryl; ABC, ATP-binding cassette (transporter); SR-BI, sacavenger receptor class B type 1;MTTP, microsomal triglyceride transfer protein; Apo, apolipoprotein; CCK, cholecystokinin.
c Contradictory results were reported by different groups (see Text for details). Modified from Wang, Paigen, and Carey4 with permission.
When the dietary conditions are controlled, biliary factors such as secretion rates of biliary lipids (bile salt, cholesterol, and phospholipid), and cholesterol content of bile, as well as size, molecular composition, and hydrophilic-hydrophobic balance of the bile salt pool,9,10 could together exert major influences on the efficiency of intestinal cholesterol absorption. Any of these could explain, in part, the inter-individual and inter-strain differences in cholesterol absorption efficiency. For example, knockout of multidrug resistance gene 2 (Mdr2) inhibits biliary secretion of phospholipid, and curtails intestinal cholesterol absorption efficiency.26,27 Studies in homozygous and heterozygous Mdr2 deficient mice suggest that physiological phospholipid outputs are necessary for normal intestinal cholesterol absorption.27 In cholesterol 7α-hydroxylase knockout mice,28 biliary bile salt pool sizes and biliary bile salt outputs are reduced markedly and the animals absorb only trace amounts of cholesterol because of bile salt deficiency. However, cholesterol absorption is reversed readily by feeding a diet containing 0.2% cholic acid. This confirms that biliary bile salt pool size and biliary bile salt output play a crucial role in cholesterol absorption via intraluminal bile salt micellar concentrations. Changes in the hydrophilic-hydrophobic balance of the bile salt pool also influence cholesterol absorption.9
In addition, it is observed29 that the higher cholesterolabsorbing C57L mice have significantly higher secretion rates of all three major biliary lipids (bile salts, cholesterol, and phospholipids) and elevated cholesterol content of bile compared with the lower cholesterol-absorbing AKR mice. These results show a positive relationship between high intestinal cholesterol absorption and augmented biliary cholesterol outputs, as well as high gallstone prevalence rates, suggesting that the effect on bile is secondary to increased intestinal cholesterol absorption.3,4
Several studies in humans and animals suggest that rapid small intestinal transit time reduces cholesterol absorption. Ponz de Leon et al30 produced evidence in humans by pharmacological intervention that acceleration of small intestine transit is consistently associated with decreased cholesterol absorption. Also, Traber and Ostwald31 found that in guinea pigs resistant to the plasma effects of dietary cholesterol, intestinal transit times are more rapid than in other guinea pigs with hypercholesterolemia. Furthermore, cholecystokinin-A receptor deficient mice display significantly higher intestinal cholesterol absorption rates which correlate with slow small intestinal transit rates; this in turn induces biliary cholesterol hypersecretion and cholesterol gallstone formation.32 However, it is surprising to find that small intestinal transit time and the length and weight of small intestine among low, middle, and high cholesterol-absorbing mouse strains are essentially identical.4 Taken together, these studies reveal that under the physiological conditions, luminal factors are not responsible for the differences in intestinal cholesterol absorption efficiency in these diverse mouse strains. In addition, intestinal cholesterol absorption efficiency increases markedly with aging33,34 and there are gender differences in cholesterol absorption efficiency,33-35 suggesting that aging and female sex hormones could have some effects on cholesterol absorption.
Genetic influences on variations in intestinal cholesterol absorption efficiencyIt has been observed that with similar dietary cholesterol intake, inter-individual and inter-strain variations in intestinal cholesterol absorption efficiency exist in primates, 36,37 including humans,38-41 as well as in inbred strains of rabbits,42,43 rats,44 and mice.4,45-47 This strongly suggests that intestinal cholesterol absorption is regulated by multiple genes since diet, a key environmental factor is controlled in these studies. Recently, it is found4 that there are variations in cholesterol absorption efficiency among 12 strains of inbred mice, and bile salt secretion rates and pool sizes are two key biliary factors in the regulation of intestinal cholesterol absorption. Of note is that neither molecular compositions of bile salt pool nor small intestinal transit times vary significantly among these mouse strains.4 Especially, when dietary factors are controlled by feeding chow (< 0.02% cholesterol), cholesterol absorption efficiency in C57L mice with intact enterohepatic circulation of bile salt is significantly higher compared with AKR mice as measured by four independent methods, i.e., the plasma dual isotope ratio method, the fecal dual isotope ratio method, the lymphatic transport of cholesterol, and the mass balance method.3,4 When these studies are repeated in mice with chronic biliary fistulae but in the setting of infusion of taurocholate and egg yolk lecithin, it is observed that the marked differences in cholesterol absorption efficiency still persist between AKR and C57L strains. Overall, these studies4 suggest that the genetic factors at the enterocyte level are crucial in determining the variations of intestinal cholesterol absorption efficiency. The question arises therefore, as to which cellular step(s) in the absorption of cholesterol might be inherently different. Furthermore, cholesterol absorption in (AKR´C57L)F1 mice mimics the higher-absorbing C57L parent, suggesting that high cholesterol absorption is a dominant trait in mice.
Searching for intestinal cholesterol transportersThe molecular mechanism by which cholesterol from the intestinal lumen is transferred across the apical brush border membrane into the mucosal cell still remains poorly elucidated. The prevailing view for the molecular mechanism of cholesterol absorption has been that luminal unesterified cholesterol is shuttled across the unstirred water layer in a bile salt-containing micelle. After reaching the cell surface of the enterocyte, individual cholesterol molecules are incorporated into the brush border membrane and enter the cell interior by simple passive diffusion. This process of cholesterol transfer has no requirement for a carrier molecule to mediate cholesterol absorption. However, for water-insoluble lipids with very low monomer solubility (=10-8 M) such as cholesterol, this mechanism is inefficient.
Although a simple passive diffusion process is widely assumed for intestinal cholesterol absorption, several lines of evidence support the existence of an energy-independent, protein-facilitated mechanism for cholesterol uptake by the enterocyte: (i) Transport of cholesterol from mixed micelles or small unilamellar vesicles to brush border membrane vesicles follows second order kinetics and is sensitive to protease;48,49 (ii) structurally related plant sterols such as β-sitosterol and campesterol that differ from cholesterol only in the degree of saturation of the sterol nucleus or in the nature of the side chain at carbon-24 are less efficiently absorbed than cholesterol; 50,51 (iii) sitosterolemia, a rare autosomal recessive disorder is characterized by excess plant sterol absorption, suggesting that the ability to discriminate between plant sterols and cholesterol appears to have been lost in this disease;52,53 (iv) intestinal cholesterol absorption can be specifically inhibited by cholesterol absorption inhibitors of different chemical structure: 2-azetidinones and sterol glycosides, each class showing profound structure-activity relationships.54,55
The in vitro study from Hauser and co-workers56 suggests the scavenger receptor class B type I (SR-BI) mediates intestinal cholesterol absorption. Their immunoblotting data demonstrated that SR-BI protein is expressed in brush border membrane preparations and Caco-2 cells and preincubation with anti-SR-BI antibody partially inhibits cholesterol and cholesteryl ester uptake by brush border membrane vesicles and Caco-2 cells compared with no antibody control incubations. Their results suggest that SR-BI may be involved in the absorption of dietary lipids, and might be a putative sterol transporter. However, knockout of the Sr-b1 gene in mice appears to have little effect on intestinal cholesterol absorption.57-59
Repa and colleagues60 showed that intestinal ATPbinding cassette (ABC) transporter ABCA1 serves to efflux cholesterol from the enterocyte back into the intestinal lumen, thereby modulating net cholesterol absorption efficiency,61,62 as well as cholesterol absorption and the transcriptional regulation of Abca1 gene expression are mediated by the RXR/LXR heterodimer. More recently, it is found that ABCA1 protein expression is not located at the apical brush border membrane of the enterocyte, but on the basolateral membrane.63,64 It is hypothesized therefore that transfer of cholesterol into lymph by ABCA1 may involve in HDL particles. Clearly, additional studies are required to pursue this tantalizing observation.
Mutations in the genes for these two proteins, ABCG5 and ABCG8,65,66 result in sitosterolemia, a rare autosomal recessive disorder characterized by hyperabsorption of sitosterol and other plant sterols. Sitosterolemic individuals also absorb cholesterol more efficiently and are often hypercholesterolemic, implying a role of ABCG5 and ABCG8 in modulating the efficiency of cholesterol absorption. This suggests that cholesterol absorption is a selective process in which plant sterols and other non-cholesterol sterols are absorbed poorly or not at all. Recent research on the sterol efflux pumps ABCG5 and ABCG8 provides an explanation for this selectivity.67-72 These studies yield new insights into the mechanisms that ABCG5 and ABCG8 promote partial efflux of cholesterol and nearly complete efflux of plant sterols from the enterocyte into the intestinal lumen, and may play a critical role in modulating the amount of cholesterol that reaches the lymph from the intestinal lumen. One question that remains is whether ABCG5/G8 alone is sufficient and required or whether other proteins are integral to this process.
Over the past decade, several groups have been searching for a cholesterol transporter that is located at the apical brush border membrane of the enterocyte.48,49,73-76 More recently, Kramer and co-workers77 found that by photoaffinity labeling using photoreactive derivatives of cholesterol and 2-azetidinone cholesterol absorption inhibitor, an 80-kDa and a 145-kDa integral membrane protein are identified as specific binding proteins for cholesterol and cholesterol absorption inhibitor, respectively, in the brush border membrane of the enterocyte. The 80-kDa cholesterol-binding protein does not interact with cholesterol absorption inhibitor and vice versa, as well as cholesterol or plant sterols do not interfere with the 145-kDa molecular target for cholesterol absorption inhibitor. Both proteins show an identical tissue distribution and are exclusively found at the anatomical sites of cholesterol absorption: duodenum, jejunum, and ileum. Furthermore, both proteins are different from the hitherto described candidate proteins for the intestinal cholesterol transporters such as SR-BI, ABCA1, ABCG5, or ABCG8. Their results strongly suggest that intestinal cholesterol absorption is not facilitated by a single transporter protein but occurs by a complex machinery. Furthermore, a novel selective cholesterol absorption inhibitor ezetimibe decreases intestinal cholesterol absorption, but does not influence gene expression of intestinal Sr-b1, Abca1, Abcg5, and Abcg8, thus suggesting that this drug might curtail the activity of a putative sterol transporter at the brush border membrane of the enterocyte that actively facilitates the uptake of cholesterol.78
Pharmacological control of intestinal cholesterol absorptionThe use of cholesterol absorption inhibitors for treating hypercholesterolemia has a long history, with several classes of compounds having been developed. In this review, we will discuss bile salts, plant sterols, and ezetimibe, as well as their actions on intestinal cholesterol absorption because they has been shown to have marked effects on lowering plasma or biliary cholesterol levels in the human.
Bile salts. Ursodeoxycholic acid (UDCA) has been used to treat cholesterol gallstones for more than twenty years,79 and decreasing intestinal cholesterol absorption is one of its major therapeutic actions.80-82 Recently, Wang and colleagues9 explored the influence of the hydrophilichydrophobic balance of a series of natural bile acids on cholesterol absorption in the mouse. Because bacterial and especially hepatic biotransformations of specific bile acids occurr, hydrophobicity indices of the resultant bile salt pools differ from the fed bile acids. They9 observed a significant and positive correlation between hydrophobicity indices of the bile salt pool and percent cholesterol absorption. The principal mechanism whereby hydrophilic bile acids inhibit cholesterol absorption appears to be via the uptake step by curtailing micellar cholesterol solubilization intraluminally.9,83-85 Hence, decreasing the hydrophobicity index of the biliary bile salt pool reduces cholesterol’s bioavailability for absorption by enterocytes. Furthermore, gene expression of the intestinal sterol efflux transporters Abcg5 and Abcg8 is up-regulated by feeding cholic acid, but not by the hydrophilic β-muricholic acid nor by the hydrophobic deoxycholic acid.9 Their study9 suggests that natural hydrophilic bile acids efficiently suppress cholesterol absorption, and may act as potent plasma and biliary cholesterol-lowering agents, even more so than UDCA, for prevention of cholesterol deposition diseases in humans. An example of the latter is a recent study86 showing that β-muricholic acid efficiently prevents cholesterol gallstone formation in gallstonesusceptible C57L mice by chronically inhibiting intestinal cholesterol absorption.
Plant sterols (Phytosterols): Plant sterols have the same basic function in plants as cholesterol in animals; that is, they play a key role in cell membrane function. Over the past decade, the possibility of using plant sterols as ingredients in functional foods has led to numerous research studies87-89 in relation to their ability to reduce plasma cholesterol. The main conclusion is that the effective doses are between 1.5 and 3g/day, leading to a reduction between 8% and 15% in plasma LDL-cholesterol. Unlike cholesterol, plant sterols have a very low capacity for intestinal absorption,90 which, together with their high rate of biliary secretion by the liver, leads to an extremely low level of plant sterols in the plasma. Cholesterol absorption from the dietary and the biliary sources is strongly reduced in the presence of plant sterols, and the unabsorbed cholesterol is excreted in the feces. The commonly accepted, basic mechanism of action of these compounds is that, in appropriate conditions, they can become efficiently incorporated into the micelles in the intestinal lumen, displace the cholesterol, and lead to its precipitation with other, non-solubilized plant sterols.91-94 Furthermore, competition between cholesterol and plant sterols for incorporation into micelles, for transfer into the brush border membrane, as well as competition within the cell for ACAT, could explain the effect of large amounts of plant sterols to inhibit cholesterol absorption. This process reduces both the cholesterol and the triglycerides in the liver, which is compensated for by two different mechanisms: an increase in cholesterol synthesis, detected as an increase in its precursors lathosterol and desmosterol, and an increase in the LDL receptors. In contrast, cholesterol synthesis is strongly inhibited by the Δ22-sterols (stigmasterol), by the competitive inhibition of sterol Δ24-reductase, which is an interesting secondary mechanism for future research.
Ezetimibe: Ezetimibe (SCH 58235) and its analogs SCH 48461 and SCH 58053 are novel potent and selective inhibitors of cholesterol absorption,95,96 and markedly lowering plasma LDL-cholesterol levels at a very low dose range in the human is similar to that at which statins are routinely given. A daily dose of 10 mg of ezetimibe alone effects an average reduction of about 18% in plasma LDL-cholesterol levels.97
Ezetimibe is glucuronidated in the enterocyte during its first pass. Both ezetimibe and its glucuronide are circulated enterohepatically,98 repeatedly delivering the agent back to the site of action on the luminal surface of the enterocyte. This agent does not change the physicochemical nature of the intraluminal environment, nor does it increase the expression of proteins ABCG5/G8 that drive sterol efflux from the enterocyte. Furthermore, ezetimibe and its analogs are relatively small molecular structures that do not affect the enterohepatic flux of bile acids, but rather appear to act by disrupting the uptake of sterol across the microvillous membrane, i.e., inhibiting a putative sterol transporter that facilitates the movement of cholesterol into the intestinal cell. This mechanism remains to be the subject of intensive investigation. In addition, there is a marked compensatory increase in cholesterol synthesis in the liver, but not in the peripheral organs, and an accelerated loss of cholesterol in the feces with little or no change in the rate of conversion of cholesterol to bile salts. Recent studies99-101 show that the combination of ezetimibe with either atorvastatin or simvastatin offers a powerful new therapeutic approach to the control of LDL-cholesterol levels in the general population, as well as provides a complementary treatment strategy for patients with homozygous familial hypercholesterolemia, a high-risk population.
ConclusionsThe significant inter-individual differences found in the human and inter-strain variations observed in the inbred mouse strains strongly suggest that multiple genes are involved; however, the question as to which cellular step(s) in the absorption of cholesterol is inherently different remains unresolved. Cholesterol absorption is a selective process in that plant sterols are absorbed poorly or not at all, and recent research on the sterol efflux transporters ABCG5 and ABCG8 provides an explanation for this selectivity. Also, growing genetic and biochemical evidence suggests a sterol transporter that facilitates the movement of cholesterol into the intestinal cell, and the identification of such a gene is predicted to be elucidated in the near future, which should yield new insights into the mechanisms that potentially regulate the influx of cholesterol across the enterocyte. Understanding the molecular mechanisms whereby cholesterol is absorbed will provide a powerful novel strategy for the prevention and treatment of coronary heart disease and cholesterol gallstones.
AcknowledgementsDr. Wang is a recipient of a New Scholar Award from the Ellison Medical Foundation (1999-2003). This work is supported in part by a grant from the Ellison Medical Foundation and a research grant DK54012 from the National Institutes of Health (US Public Health Service).