Introduction: Nodular regenerative hyperplasia (NRH) is a rare condition is associated to immune, neoplastic, vascular disorders, and certain drugs and toxins. Portal hypertension is the main complication. Aim: To report the case of a woman with NRH and aplastic anemia, association not previously described. Case: A 31-year-old hispanic female presented with pancitopenia and cholestasis. Bone marrow biopsy: aplastic anemia. Abdominal ultrasound revealed multiple liver nodules, without hepato-splenomegaly. No abnormalities were noted in hepatic vessels. Antimitochondrial (AMAs) were positive. Coagulation tests were normal. Liver biopsy: hepatocite nodules with central atrophy and sinusoidal dilatation in the absence of significant fibrosis. No arteritis, thrombosis or bile duct damage was found. Discussion: Pathogenesis of NRH remains unclear. The most accepted theory was developed by Wanless 24 years ago, and reinforced in 1997. It states that alterations in hepatic blood flow (portal obliterative venopathy) originate a specific response, initially consisting of apoptosis secondary to acute ischemia, with ensuing parenchymal atrophy and surrounding areas of liver regeneration and chronic ischemia. The common pathologic mechanism of all the diseases associated with NRH involves liver blood-flow abnormalities secondary to microthromboses, vascular congestion, or vasculitis. In the current case we were unable to document evidence of liver flow abnormalities. Noteworthy, there are previous descriptions of the association of NRH with primary biliary cirrhosis, and this patient was AMA positive, but without bile duct damage in liver biopsy. Conclusions: We cannot sustain Wanless’ theory, and this is the first description of the association of NRH with aplastic anemia.
Hepatic nodular regenerative hyperplasia (NRH) is a rare liver disease of unknown etiology that has been associated with immune, malignant and vascular diseases as well as with certain drugs and toxins. The disease is characterized by the presence of multiple regenerative nodules distributed throughout the liver parenchyma in the absence of fibrosis. It pathogenesis is thought to be related to the occlusion of intrahepatic portal vein radicals leading to inadequate blood flow resulting in local ischemia and atrophy with compensatory regeneration of surrounding hepatocytes with compression of adjacent lobules1. The main clinical manifestations are those related to portal hypertension, mainly upper gastrointestinal bleeding.
We report the case of a young female patient with NRH associated with aplastic anemia, of possible autoimmune etiology. To our knowledge this association has not been previously described in the literature.
Case reportA 31-year old Mexican female was referred to our institution for evaluation of pancytopenia and cholestasis. Her history was unremarkable except for having received anticonvulsive treatment for 4 years with phenytoin and valproic acid. Medical treatment had been discontinued 8 years prior to her admission and the patient had been seizure-free since then. At admission to our hospital the patient was pale and mildly jaundiced with generalized petechiae. Vital signs were normal and at physical exam mild eyelid and lower limb edema as well as mild ascites were noted. No stigmata of chronic liver disease, hepatomegaly or splenomegaly were present. Heart sounds and lungs were normal.
Her laboratory results revealed: hemoglobin 6.7 g/dL, white blood cells 2,700 cells/μ L, neutrophils 500 cells/ μ L, platelets 35,000/μ L with reticulocyte count of 0%. Serum glucose, creatinine and blood urea nitrogen were normal. Liver chemistries showed ALT 61 U/L, AST 70 U/L, total bilirubin 3.3 mg/dL, conjugated bilirubin 1 mg/ dL, alkaline phosphatase 203 U/L, albumin 3.7 g/dL, globulin 3.9 g/dL, prothrombin time 15.8“, INR 1.4, partial thromboplastin time 26.4”.
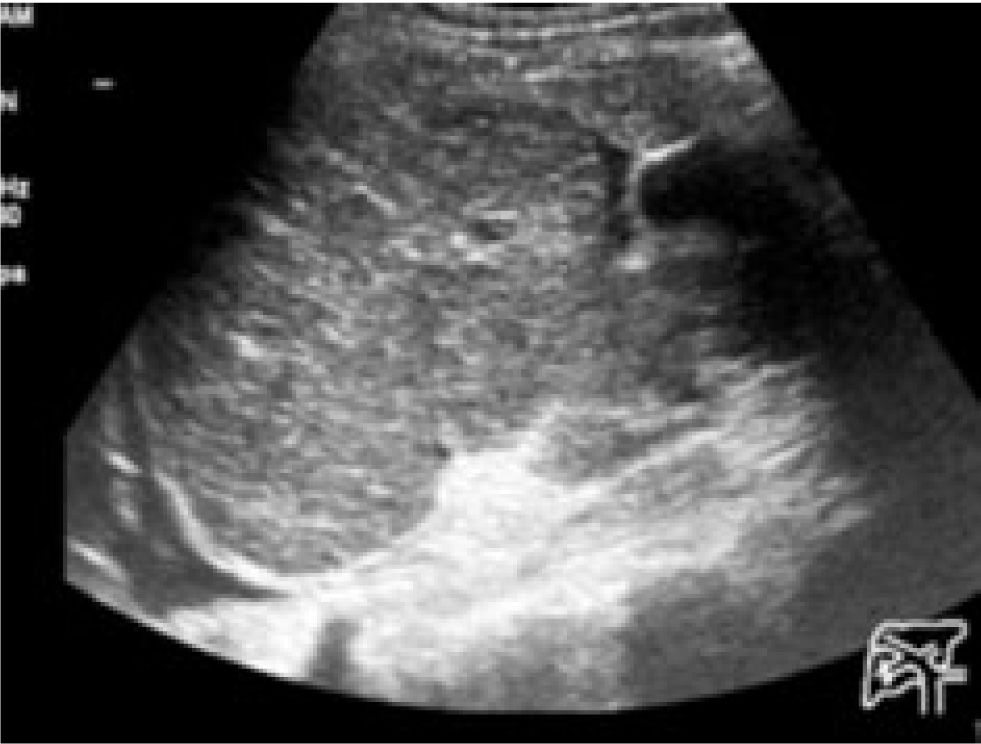
An abdominal ultrasound (Fugure 1) demonstrated the presence of multiple hepatic nodular lesions of several centimeters in diameter without evidence of portal hypertension, splenomegaly or thrombosis of intra-and extra-hepatic blood vessels. Mild ascites was noted. CT scan (Fugure 2) and MRI (Fugures 3,4) confirmed the presence of regenerative-looking nodular liver lesions. Serum markers for hepatitis B and C viruses were negative. Anti-mitochondrial antibodies were mildly positive (2.6, with normal range of 0-1), anti-nuclear antibodies with a titer of 1:80 were detected. Immunoglobulins IgA, IgG and IgM were within normal levels. Prothrombotic tests were normal or negative, including protein C, protein S, anti-thrombin III, anti-phospholipid antibodies and factor V Leiden mutation.
The patient underwent a bone marrow aspirate and bone biopsy that showed cellularity of 1% in the absence of myelofibrosis. A liver biopsy (Fugures 5,6) demonstrated the presence of multiple hepatocyte nodules in the absence of fibrosis with atrophy of intranodular hepato-cytes with sinusoidal dilatation. There was no sign of vascular damage or damage to bile ducts. These findings are compatible with NRH.
Treatment with anti-thymocyte globulin at a dose of 40 mg/kg and cyclosporine 10 mg/kg/day was started. Five weeks after treatment the patient had a partial response of her aplastic anemia (hemoglobin 9.9 g/dL, white blood cells 3,900 cells/* L, neutrophils 49% and platelets of 101,000/* L). One year after admission the patient is doing well with immunosuppressive treatment for aplastic anemia. She does not have evidence of liver dysfunction or portal hypertension.
DiscussionNodular regenerative hyperplasia is characterized by the presence of diffusely localized, well defined nodules in the liver. They seem to form as a response to some type of liver injury, mainly necrosis or disturbed intrahepatic blood flow. Of note is the absence of fibrosis between the nodules.2 This pathologic finding has been associated with several diseases, especially of autoimmune origin, such as rheumatoid arthritis and Felty’s syndrome.3-6 Other associations include hematologic diseases such as multiple myeloma, myelofibrosis, polycythemia vera and Celiac Disease.7-9 Other less frequent associations include the chronic use of oral contraceptives, steroids and chemotherapy; as well as disorders leading to vascular injury such as arteritis, thrombosis and organ transplantation.
NRH is generally an autopsy finding with a reported frequency of 2.5%.10 When clinical manifestation are present they are commonly related to the complications of portal hypertension, namely esophageal varices and upper gastrointestinal bleeding.8,9 Less frequently, the presence of intrahepatic cholestasis can be the sole marker of disease. The pathogenesis of NRH is unclear, but the most accepted theory is that by Wanless and colleagues published initially more than 25 years ago1 and updated more recently.11 This theory suggests that a state of decreased hepatic blood flow (initially called portal obliterative venopathy) results in a specific response from the affected liver. This response is characterized by hepatocyte apoptosis in the case of acute ischemia, followed by local atrophy surrounded by areas of regenerative hepatocytes (regenerative nodules) in response to chronic ischemia. The common pathogenic mechanism involved in the diseases with a well established association to NRH is the presence of a disturbed liver blood flow secondary to microthombosis, chronic venous congestion or vasculitis. In the present case we were unable to find clinical, biochemical or histological evidence of abnormal liver blood flow. Of interest, there have been previous descriptions of NRH associated with primary biliary cirrhosis and the patient we describe indeed had positive anti-mitochondrial antibodies, although no injury to the bile duct was evident on liver biopsy, which would not support the diagnosis of primary biliary cirrhosis in the present patient. Aside from the absence of previous reports of NRH associated with aplastic anemia, the present case would not support the pathogenesis of NRH proposed by Wanless, as no obvious disturbed hepatic blood flow was documented and no histological signs of thrombosis, ischemia or vascular injury were present in the liver biopsy. The patient did have a well documented, possibly autoimmune, mild aplastic anemia according to the Camitta12 classification. This hematological disease is very different from the myeloproliferative states in which microthrombosis or vasculitis can commonly cause disturbances in liver blood flow and ultimately result in NRH.