The hepatitis B virus (HBV) is one of the most frequently transmitted agents in dialysis units. Occult hepatitis B is characterized by HBV infection without detectable surface antigen (HBsAg) in the patient’s serum, a positive or negative HBV DNA marker result in the serum and a positive result in the liver tissue, which leads to the potential risk of transmission during renal replacement therapy service. There is variation in occult hepatitis B prevalence rates in this population across various studies that may be related to numerous factors. The presence of occult hepatitis B in individuals undergoing renal replacement therapy is important with regard to both the possibility of transmission and the consequences for the patient, especially the development of chronic liver disease and reactivation of the disease after renal transplantation.
The hepatitis B virus (HBV) is one of the most common infections in the world (it is estimated that there are over 360 million carriers of the chronic infection) and is a major cause of hepatic cirrhosis and hepatocellular carcinoma (HCC).1 HBV transmission by blood products originating from individuals with negative results for the virus surface antigen (HBsAg) has been demonstrated since the 1980s. These individuals are known as occult hepatitis B carriers (OHB).2 OHB has been linked to cases of cryptogenic cirrhosis and HCC.3,4 As patients with chronic renal failure (CRF) on dialysis are a population at risk for the parenteral transmission of pathogens, HBV infection is a continuing concern despite all of the measures used in its prevention, including mandatory vaccination for all susceptible individuals5–7 OHB can be a significant problem in this population, justifying this review of the topic.
Occult Hepatitis BThe definition of OHB was standardized in 2008 at a meeting of experts in the city of Taormina (Italy).8 The main definitions resulting from this meeting were as follows:
- •
OHB is a clinical entity in which the individual is positive for HBV DNA in liver tissue but has undetectable serum HBsAg by routinely used methods and positive or negative HBV-DNA in the serum, and
- •
When the HBV-DNA in the serum is positive, it often does not exceed 200 IU/mL.
This last point was added by the meeting participants to distinguish so-called false occult hepatitis B, in which HBsAg is not detected due to infection with the S gene escape mutant of the HBV genome, which prevents the production of HBsAg but has a high viral load that is consistent with loads that are manifested during classic chronic infection phases. There are still differences in the literature regarding the definition of this entity, as many authors consider the latter to be OHB.9
It is believed that most cases of OHB follow an acute HBV infection in which viral replication continues indefinitely after the disappearance of HBsAg or occurs after many years of chronic infection in which there was loss of HBsAg.10–14 These individuals can transmit HBV through transfusions of their blood derivatives or through donation of their organs for transplant and may, if subjected to immunosuppression, show reactivation of hepatitis B.8,14,15
Most OHB carriers show positivity for other serological markers of HBV (anti-HBc and/or anti-HBs), but 20% of them are seronegative for all markers.16
Unique characteristics of HBV infection and one that seems to be fundamental in OHB is the persistence of the circular shape of its episomal genomic DNA (cccDNA) in the hepatocyte nucleus, which maintains viral replication.17,18 It has been observed that the HBV variant most frequently found in OHB is the wild type strain, with no genetic mutations and with replication stages similar to those occurring in the classical infection,19,20 but strong suppression of viral replication and gene expression by antiviral cytotoxic T cells is responsible for the very low or undetectable levels of serum HBV DNA.20 Another event that can suppress replication of HBV is co-infection with other viruses, particularly the hepatitis C virus (HCV).21 It has been reported that the antigen core of HCV strongly inhibits the replication of HBV.17
The exact clinical relevance of OHB is not clear, but the possible role exerted by this infection on the cryptogenic cirrhosis and HCC development has been demonstrated by several studies and recently revised.17 It has also been noted that the presence of OHB can negatively affect the response to treatment of chronic hepatitis C.22 Another important feature of this entity is the possibility of reactivating hepatitis B under immunosuppressive conditions, such as chemotherapy and organ transplantation.15,23,24
DiagnosisStandardized tests for the diagnosis of OHB are still not available. The gold standard test currently used is the identification of HBV DNA in liver tissue by very sensitive amplification tests (nested PCR and real-time PCR).8,9,16 As tests on liver tissue are not easily available because of the necessity of performing a liver biopsy, in practice, these tests are performed on serum. The Taormina consensus recommended using primers for different highly conserved segments of the viral genome. Usually the S, pre-C/C and X regions are used.25
PrevalenceThe prevalence of OHB predominantly depends on a region’s level of endemicity19 and the susceptibility of the population studied, which is higher in those populations with higher risk of parenteral infection and immunosuppressed patients,16,26,27 HCV carriers28 and those with cirrhosis and HCC of unknown causes.3,4
In addition to these traditional populations’ OHB has also been reported in low-risk populations such as blood donors in various parts of the world, including Brazil.29,30
Hepatitis B in HemodialysisChronic kidney disease in its most advanced stage (stage V) is a significant problem that is present in almost all countries. The incidence has continued to increase, mainly as a result of the consequences of diabetes mellitus and hypertension.31 Renal replacement therapies (RRT) such as hemodialysis are the final treatment for these individuals.
HBV infection can cause increased morbidity in patients in the terminal stage of chronic kidney disease. As one of the main modes of transmission of this virus is the parenteral route, these patients have a high risk of acquiring an infection by this mechanism because hemodialysis requires prolonged vascular access. It has been observed that HBV is the most common virus transmitted by this route in this population.7,32,33
Despite this susceptibility, the prevalence of HBV has decreased in dialysis centers around the world, including those in Brazil.33–34 According to data from the Brazilian Society of Nephrology the prevalence of HBsAg in Brazilian dialysis units was approximately 1.1% in 2010.34 These numbers were as high as 41% for the same serological marker in the 1980s.35 This decrease can be attributed to mandatory vaccination, segregation of infected individuals into different rooms and dedicated hemodialysis machines, and the implementation of standard precautions to prevent pathogen transmission in dialysis centers.33,36
Once the individual on dialysis is contaminated with HBV, the possibility of becoming a chronic carrier is very high, which is not the case with immunocompetent individuals. Although this population is immunocompromised, the natural history of this infection in this population appears no different from that observed in normal individuals.37 Its major clinical importance seems to be after renal transplantation, as it can cause reactivation episodes that may be so severe that they cause the patient’s death.38
Occult Hepatitis B in Patients on HemodialysisHBV infection with HBsAg-negative serum in hemodialysis patients was initially reported by Cabrerizo, et al.39 This team investigated 33 patients who were HBsAg negative looking for HBV-DNA in the serum and detected the marker in 19 patients (58%). Among these patients, 12 (63%) had a serological marker for HBV. Since that report, many studies have been published on the subject, revealing the presence of a significant problem in almost all countries, as recently reviewed by Hollinger, et al.40
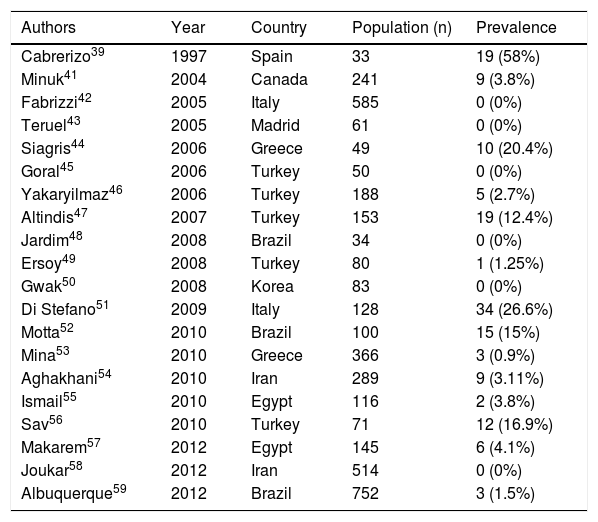
The prevalence of OHB in hemodialysis is quite variable, ranging from 0-58% (Table 1). This variability, as observed in subjects with normal renal function, must be related to the degree of endemicity of HBV in a region, the sensitivity of the tests used and selection biases.39,41–59
Prevalence rates of occult hepatitis B in patients undergoing renal replacement therapy (hemodialysis).
| Authors | Year | Country | Population (n) | Prevalence |
|---|---|---|---|---|
| Cabrerizo39 | 1997 | Spain | 33 | 19 (58%) |
| Minuk41 | 2004 | Canada | 241 | 9 (3.8%) |
| Fabrizzi42 | 2005 | Italy | 585 | 0 (0%) |
| Teruel43 | 2005 | Madrid | 61 | 0 (0%) |
| Siagris44 | 2006 | Greece | 49 | 10 (20.4%) |
| Goral45 | 2006 | Turkey | 50 | 0 (0%) |
| Yakaryilmaz46 | 2006 | Turkey | 188 | 5 (2.7%) |
| Altindis47 | 2007 | Turkey | 153 | 19 (12.4%) |
| Jardim48 | 2008 | Brazil | 34 | 0 (0%) |
| Ersoy49 | 2008 | Turkey | 80 | 1 (1.25%) |
| Gwak50 | 2008 | Korea | 83 | 0 (0%) |
| Di Stefano51 | 2009 | Italy | 128 | 34 (26.6%) |
| Motta52 | 2010 | Brazil | 100 | 15 (15%) |
| Mina53 | 2010 | Greece | 366 | 3 (0.9%) |
| Aghakhani54 | 2010 | Iran | 289 | 9 (3.11%) |
| Ismail55 | 2010 | Egypt | 116 | 2 (3.8%) |
| Sav56 | 2010 | Turkey | 71 | 12 (16.9%) |
| Makarem57 | 2012 | Egypt | 145 | 6 (4.1%) |
| Joukar58 | 2012 | Iran | 514 | 0 (0%) |
| Albuquerque59 | 2012 | Brazil | 752 | 3 (1.5%) |
Higher prevalence rates of OHB have been reported in the presence of anti-HBc as an isolated marker, with HBsAg and anti-HBs negative in patients without kidney failure. An Iranian study found the presence of HBV DNA in 50% of patients on hemodialysis with isolated anti-HBc.54 In contrast, a study by Fabrizzi, et al.42 involving more than 500 patients on hemodialysis in Italy found no positivity for HBV-DNA among isolated anti-HBc carriers. Similarly, in a recently published Brazilian study, HBV-DNA was positive in only 3 patients out of 135 carriers of the isolated anti-HBc profile.59 Thus, the isolated presence of anti-HBc in patients undergoing hemodialysis may have very different meanings depending on the region where it is being studied. Moreover, among hemodialysis patients infected with HCV, OHB has been found in varying degrees from 0–36%.44–46,51 In Brazil, where the prevalence of OHB patients on hemodialysis has ranged from 0 to 15%,48,52,59 a greater frequency has not been observed among patients with HCV.48,52
The need to identify individuals with OHB in dialysis units is predicated on the fact that these patients may be potential sources of HBV transmission, as the nosocomial transmission of the virus is well documented in this area.32,33 Whether all individuals undergoing dialysis should be submitted to HBV-DNA screening or whether this test should be restricted to high-risk populations still has not been ascertained.60
ConclusionAlthough the vast majority of studies on the prevalence of occult hepatitis B in hemodialysis point toward a low prevalence, it seems advisable to search for OHB under certain conditions. Screening for HBV infection should be permanent in dialysis services, and it seems sensible to test for OHB whenever there are co-infections, especially HCV and HIV, in patients with isolated antiHBc, those with liver disease of an indeterminate cause and in renal transplant candidates. This diagnosis can minimize the transmission of the virus under these conditions, as preventive measures can be taken, carriers can be screened for HCC, and serious complications due to reactivation after renal transplantation can be prevented.