Introduction and aim. The detection of hepatitis B virus (HBV) depends on primary care center activity. The present study aims to investigate the impact of peer-to-peer sessions with hepatologists on hepatitis B screening efficacy in primary care centers.
Material and methods. Peer-to-peer one-hour sessions were scheduled to improve the screening program for HBV in Seville, Spain. The sessions were focused on who should be tested for HBV and how positive cases should be referred. Fourteen out of 26 health care centers were selected to participate in peer-to-peer sessions. The centers were classified according to how many sessions they held (no sessions, one session or more than one session).
Results. Over a five-year period, HBV screening was performed in 32 203 people. In Seville, the prevalence of HBsAg was 0.87% (283/32 203). The detection rates for new HBsAg-positive cases were 7.1, 16.9 and 21.3 cases/105 population/year in non-session, one-time session and more than one session centers, respectively (p < 0.05). The rate of patients who effectively visited centers as outpatients was significantly higher after peer-to-peer sessions-86/94 (91%) for one session and 81/89 (91%) for two session centers vs. 16/27 (67%) for non-session centers (p = 0.002). The only independent predictor of patient referral was peer-to-peer sessions (OR, 1.925 [95% CI, 1.002-3.699]; p < 0.05).
Conclusions. Peer-to-peer sessions in primary care centers increased HBV detection and visitation rates.
Chronic hepatitis B virus (HBV) is responsible for most cases of chronic hepatitis, cirrhosis, and hepatocellular carcinoma (HCC) around the world. An estimated 2,000 million people worldwide have contracted the virus, and more than 350 million people are carriers of the surface antigen of hepatitis B (HBsAg), representing 5% of the world population.1 Many primary care physicians have a limited understanding of HBV prevention, testing and treatment since screening for HBV in high-risk populations is not routine.2 Correct serological diagnosis of HBV is based on the detection of HBsAg. Although achieving a cure remains elusive, the current treatment controls viremia3 and slows the progression of liver fibrosis, avoiding the development of cirrhosis and decreasing the risk of developing HCC.4 In the peer-to-peer training method, hepatologists and primary care physicians involved in the current medical scenario help each other learn.5 Peer-to-peer training sessions have been investigated in previous primary care studies; however, the results have been controversial.6,7
Our aims were to assess the impact of peer-to-peer sessions between hepatologists and primary care physicians on HBV screening efficacy, to assess the influence of these sessions on the rate of patient detection and referral at primary care centers, and to evaluate the rate of patient attendance and treatment by hepatologists at the hospital.
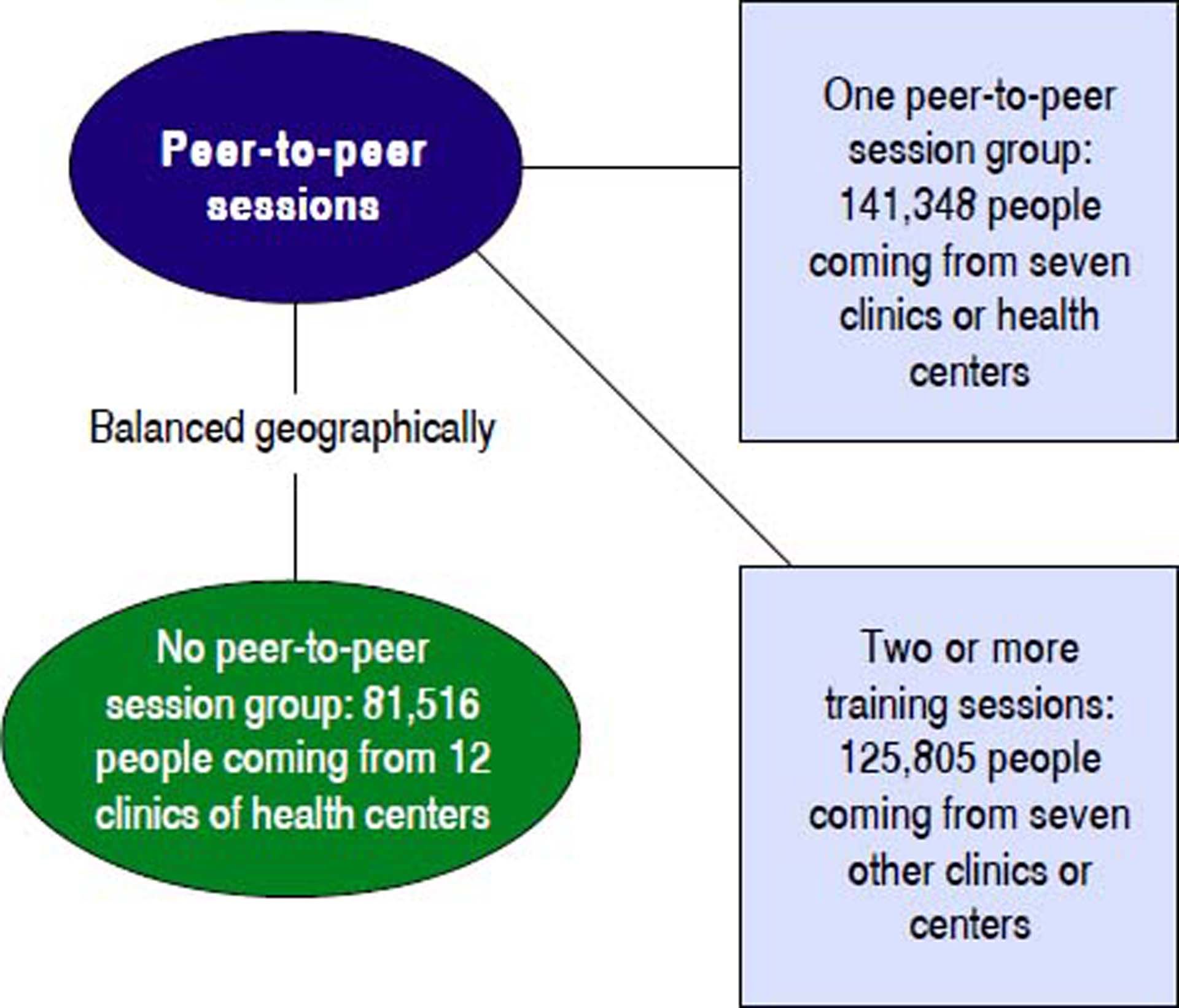
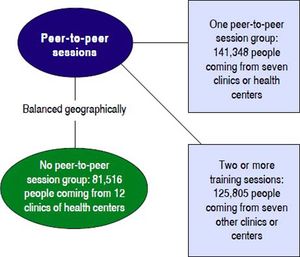
Material and MethodsParticipantsPrimary care physicians from southern Seville Sanitary District, coming from 26 primary care centers and Valme University Hospital, participated in the project. The fourteen primary centers that held sessions were selected based on their geographic dispersion, clinician availability to attend the sessions and the possibility of reaching an agreement with the director of each unit (Figure 1). Primary centers were classified into 3 groups: 12 centers without peer-to-peer session, 7 centers that held one session and 7 centers that held two or more peer-to-peer sessions. This study was approved by the local institutional review board.
Peer-to-peer sessions in primary care centersThe peer-to-peer sessions were scheduled in 14 primary care centers from 2:00 pm to 3:00 pm at the end of the morning shift. The session content included the following:
- •
The principal routes of transmission of HBV.
- •
Risk situations for hepatitis B and when to suspect an HBV infection.
- •
How to diagnose hepatitis B and the role of HBsAg detection.
HBsAg-positive patients were offered direct appointments in the hepatology outpatient office by primary care centers so that they could be referred directly to the hospital. Twenty-one sessions were developed by six hepatologists belonging to the Clinical Management Unit of Digestive Diseases at Valme University Hospital. The attendees of peer-to-peer sessions, which were primary care physicians, were coordinated by their medical director in conjunction with the principal investigator of this study. We recorded 243 attendances by primary care professionals with an average of 12.7 professionals per session.
Patient histories and serological assaysPatient medical charts were reviewed to obtain relevant information, such as HBV infection status, immigrant status, active drug or alcohol consumption and suspected liver disease. Qualitative HBsAg was measured by a commercially available enzyme-linked immunosorbent assay (Quick Titer™ Hepatitis B Surface Antigen [HBsAg] ELISA Kit. Cell Biolabs, INC. San Diego. CA USA). A recent meta-analysis suggested that the laboratory-based enzyme immunoassay had a sensitivity and specificity of 88.9% (95% CI: 87.0, 90.6) and 98.4% (95% CI: 97.8, 98.8), respectively.8 The confirmatory test was not performed.
Statistical analysisThe χ2 test was utilized to compare qualitative variables (detection rate, patient referral rate, effective referral rate, and hospital visit success rate). Quantitative variables (age) were compared with the student’s t-test or Mann-Whitney U-test. Multivariate logistic regression analyses were used to predict dichotomous variables (independent predictor influences application serology, patients’ derivation, and hospital visit success rate). Logistic regression analysis was conducted to confirm independent variables associated with screening rate and referral rate. A p < 0.05 was considered to be statistically significant. Data were analyzed using SPSS version 21 software (SPSS, Chicago, IL, USA).
Sample size calculationThe minimum number of participants in each group needed to find a statistically significant difference in the detection of HBV infection between the two study groups (peer-to-peer session versus non-session primary care centers) was 2 168 people based on an expected HBV prevalence of 0.7% to 1.68%,9 the bilateral character of the test, an α error of 5% and a power (1-β) of 80%. Given the nature of our analyzed population, the number of patients included far exceeded the required sample size.
ResultsThe target population of this study was 348,669 people who received primary care from 234 family doctors in 26 different centers in the southern area of Sevilla in Andalusia, Spain.
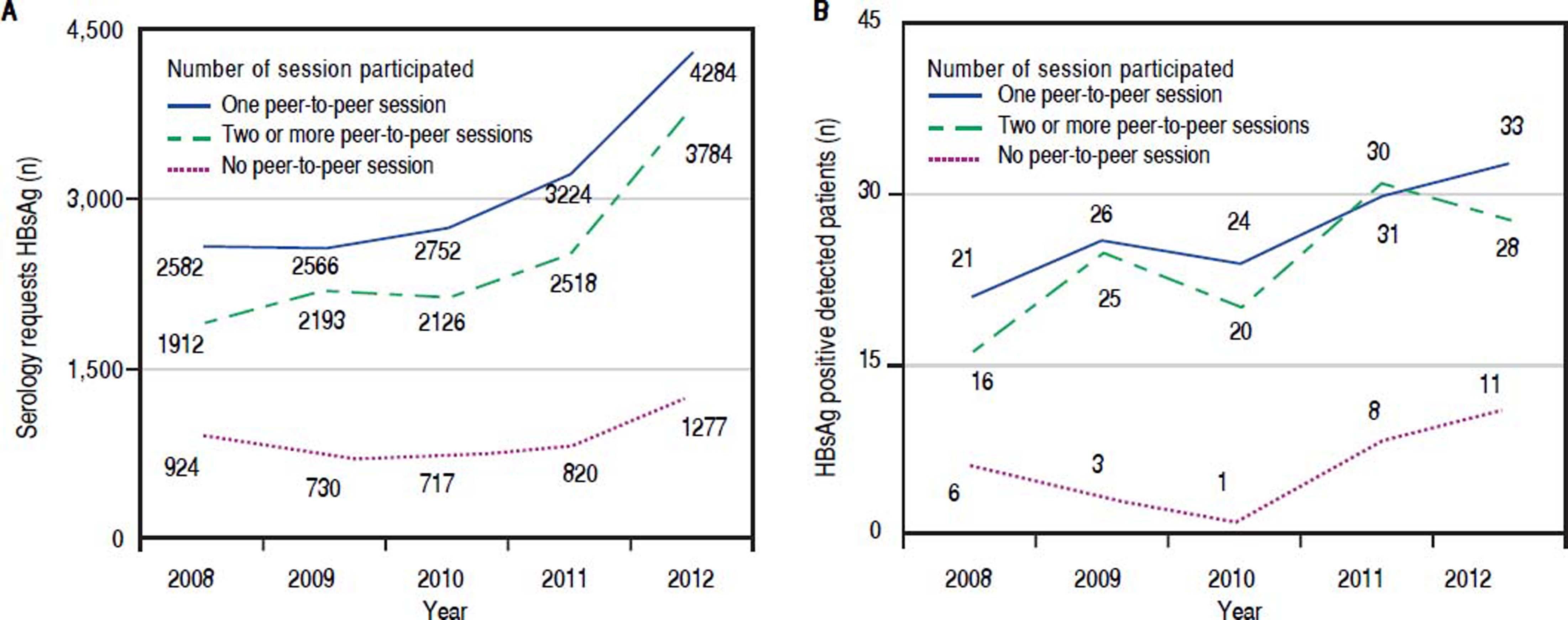
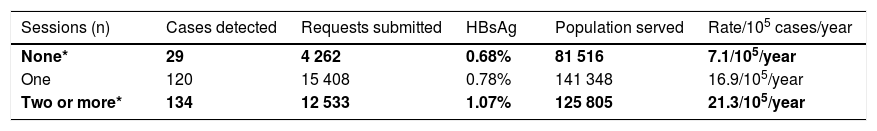
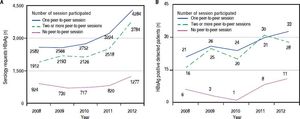
Impact of peer-to-peer sessions on detection of HBsAgDuring the five years of study, 39,591 requests for HB-sAg were analyzed, but 7,388 of these requests were repeated requests from previous years; therefore, 32,203 requests were ultimately included. There were 283 positive cases out of 32,203 requests, representing an HBsAg positivity rate of 0.873%. The detection rate of HBsAg was significantly lower in non-session centers (29 detected cases from 262 applications, 0.68%) than in centers that participated in one session (120 detected cases from 15 408 applications, 0.78%) or centers with two or more sessions (134 detected cases from 12,533 applications, 1.07%) (p < 0.01) (Table 1). The detection of new cases, number of serology requests, and detection rate increased after the sessions in 2010, with differences found between non-session and peer-to-peer session centers (Figure 2). In the final year, we detected two times as many serology applications as in the first year (Figure 2A).
Impact of the peer-to-peer sessions on the detection rate of HBsAg (*p < 0.05).
| Sessions (n) | Cases detected | Requests submitted | HBsAg | Population served | Rate/105 cases/year |
|---|---|---|---|---|---|
| None* | 29 | 4 262 | 0.68% | 81 516 | 7.1/105/year |
| One | 120 | 15 408 | 0.78% | 141 348 | 16.9/105/year |
| Two or more* | 134 | 12 533 | 1.07% | 125 805 | 21.3/105/year |
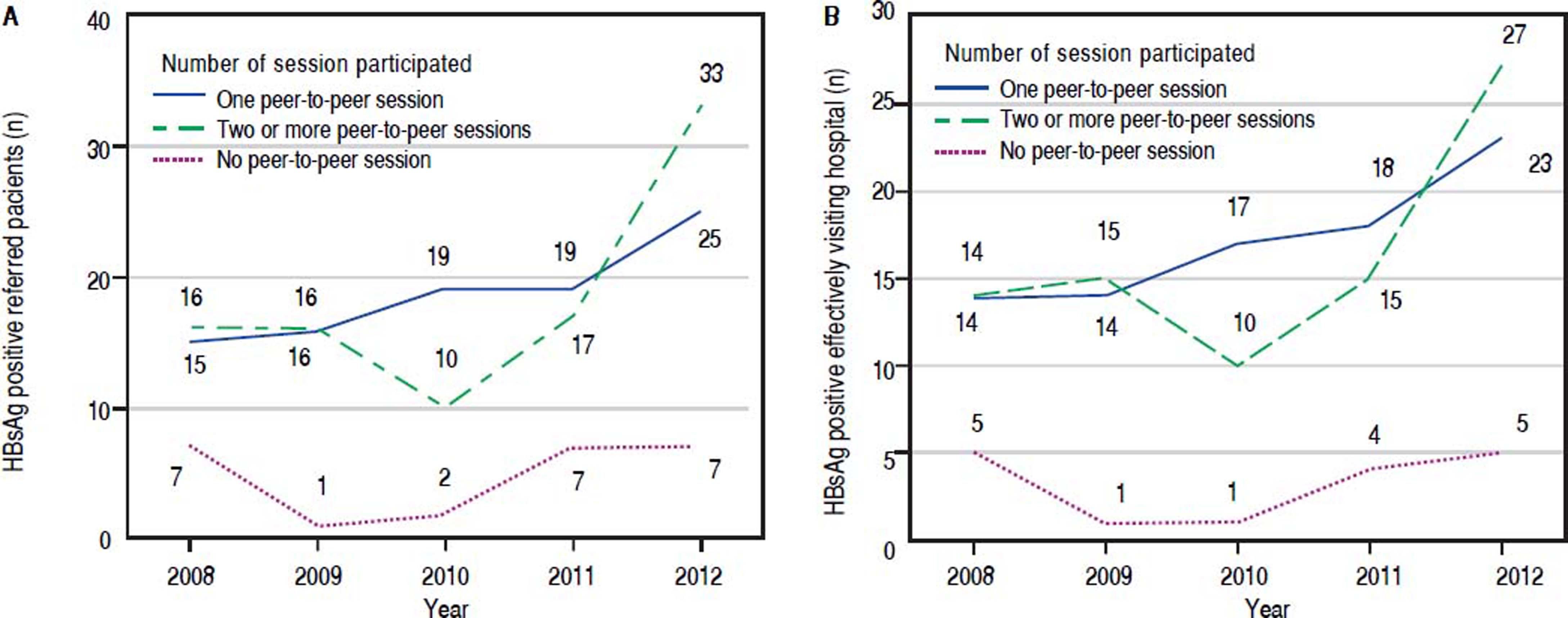
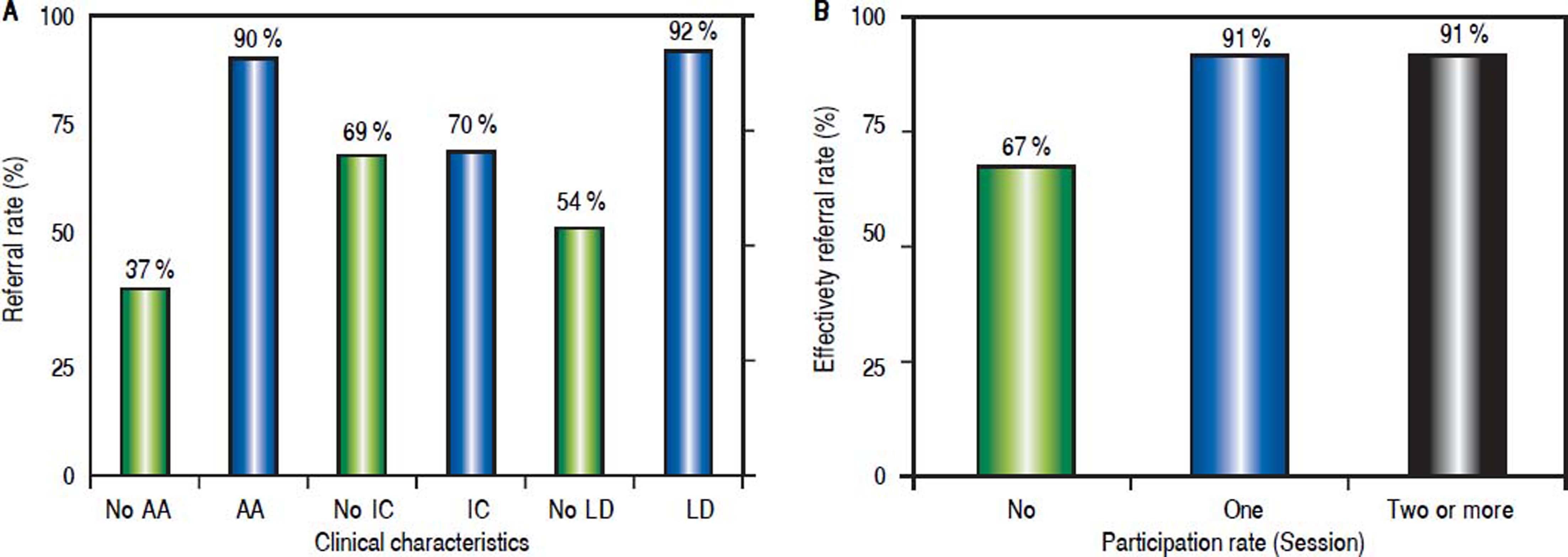
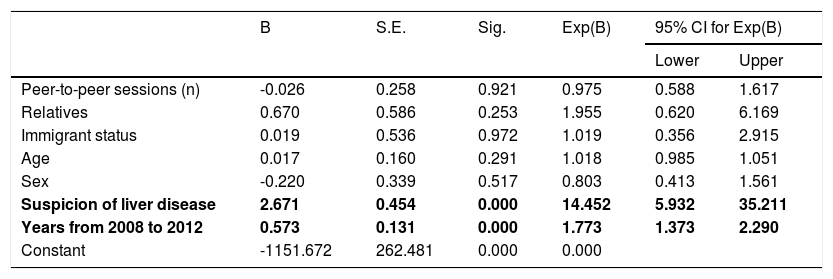
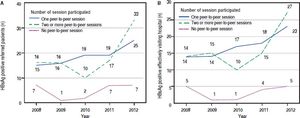
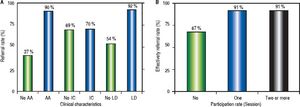
We detected HBsAg positivity in 283 cases, with 207 cases being referred for a hospital consultation (a referral rate of 73%). The rate increased steadily each year from 2008 (38/55 cases, 69%), 2009 (35/57 cases, 61%), 2010 (31/ 41, 76%), 2011 (43/59 cases, 73%) to 2012 (60/71, 85%) (p < 0.05). However, participation in specific HBV internal peer-to-peer sessions did not have an influence on the referral rate; centers without sessions were related to 24 of 34 cases (71%), centers with an internal session were related to 94 of 128 cases (73%), and centers with two sessions or more were related to 89 of 121 cases (74%) (p = 0.9). No significant difference was found between male (95/ 135, 70%) and female (112/148, 76%) (p = 0.7) patients for referral rate or in patients coming from the same family (17/24, 71%) versus unrelated patients (190/259, 73%), (p = ns). The number of referral patients increased after the sessions were completed in 2010, and the group of centers that participated in the sessions displayed an increasing trend; however, no difference was found between the group with one session or the group with two or more sessions (Figure 3A). There was no significant difference in sex, origin of citizenship, or family membership (if patients came from the same family) that influenced the referral rate. The referral rate was significantly higher in patients with suspected liver disease (94 of 102, 92%) than in other patients (75 of 138, 54%) (p < 0.0001). Additionally, in patients with active drug or alcohol consumption, the referral rate was 90% (9/10) vs. 37% (13/35) in patients with previous consumption but without active consumption (p < 0.003). In contrast, there was no significant difference in suspected inactive carriers (39 of 56, 70%) vs. the rest of the patient population (115 of 167, 69%) (p = 0.9) nor in normal ALT (110 of 156, 71%) vs. elevated ALT (46 of 65, 71%) (p = 0.9) (Figure 4A). After adjusting number of peer-to-peer sessions, relatives, immigrant status, age and sex, multivariate analysis confirmed that suspicion of liver disease (OR, 14.45 [95% CI, 5.93-35.21]; p < 0.0001) and that the referral rate by every growing year (from 2008 to 2012) (OR, 1.77 [95% CI, 1.37-2.29]; p < 0.0001) were independently associated with the referral rate (Table 2).
Multivariate analysis of the factors influencing the referral rate.
| B | S.E. | Sig. | Exp(B) | 95% CI for Exp(B) | ||
|---|---|---|---|---|---|---|
| Lower | Upper | |||||
| Peer-to-peer sessions (n) | -0.026 | 0.258 | 0.921 | 0.975 | 0.588 | 1.617 |
| Relatives | 0.670 | 0.586 | 0.253 | 1.955 | 0.620 | 6.169 |
| Immigrant status | 0.019 | 0.536 | 0.972 | 1.019 | 0.356 | 2.915 |
| Age | 0.017 | 0.160 | 0.291 | 1.018 | 0.985 | 1.051 |
| Sex | -0.220 | 0.339 | 0.517 | 0.803 | 0.413 | 1.561 |
| Suspicion of liver disease | 2.671 | 0.454 | 0.000 | 14.452 | 5.932 | 35.211 |
| Years from 2008 to 2012 | 0.573 | 0.131 | 0.000 | 1.773 | 1.373 | 2.290 |
| Constant | -1151.672 | 262.481 | 0.000 | 0.000 | ||
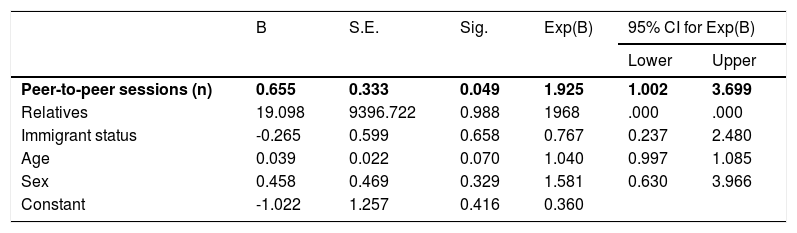
The rate of patients visiting a hospital after a positive HBsAg diagnosis was 88% (183 visiting patients out of 207 derived patients). Participation in the peer-to-peer sessions was associated with greater success in patients effectively visiting the hospital (Figure 3B). The success rate was 67% (16 of 24) in centers without participation sessions vs. 91% (86/94) in centers with one session and 91% (81/89) in centers with two or more sessions (p = 0.002) (Figure 4B). The possibility of attending a hospital was higher in autochthonous patients (160 of 177, 90%) than in immigrants (23 of 30, 77%) (p = 0.03). On the other hand, no differences were found by sex (male 85/95, 90% and female 98/112, 88%) (p = 0.65) nor referral rate: in 2008, 33 of 38 patients (87%) visited; in 2009, 30 of 35 (86%) visited; in 2010, 28 of 31 (90%) visited; in 2011, 37 out of 43 (89%) visited; and in 2012, 55 of 60 (92%) visited (p = 0.8). After adjusting relatives, immigrant status, age and sex, multivariate analysis showed the number of sessions was the only independent predictor of successful visits to a hospital for referred patients (OR, 1.925 [95% CI, 1.002-3.699]; p < 0.05). (Table 3).
Multivariate analysis of the factors influencing the effective outpatient visitation rate.
| B | S.E. | Sig. | Exp(B) | 95% CI for Exp(B) | ||
|---|---|---|---|---|---|---|
| Lower | Upper | |||||
| Peer-to-peer sessions (n) | 0.655 | 0.333 | 0.049 | 1.925 | 1.002 | 3.699 |
| Relatives | 19.098 | 9396.722 | 0.988 | 1968 | .000 | .000 |
| Immigrant status | -0.265 | 0.599 | 0.658 | 0.767 | 0.237 | 2.480 |
| Age | 0.039 | 0.022 | 0.070 | 1.040 | 0.997 | 1.085 |
| Sex | 0.458 | 0.469 | 0.329 | 1.581 | 0.630 | 3.966 |
| Constant | -1.022 | 1.257 | 0.416 | 0.360 | ||
An essential objective of public health systems is to provide continuity of care for hepatitis B to reduce perinatal transmission and mortality caused by complications, such as liver cirrhosis and liver cancer. This continuity of care requires an increase in the awareness, training, and knowledge of physicians, who act as goalkeepers of the system.2 The present study demonstrates that the implementation of peer-to-peer sessions to discuss diagnostic and therapeutic management for hepatitis B, together with direct appointments from primary care centers to outpatient offices, resulted in a higher detection rate of HBsAg positivity. The detection rate was superior in centers that participated in peer-to-peer sessions, whereas minimal differences were found between centers that participated in a single session versus those that participated in more than one session. The possible explanations for these expected findings are multiple:
- •
The peer-to-peer session enabled discussion and presented direct appointment management and serology request tools.10
- •
The session itself aroused the interest of primary care physicians in a pathology that was losing visibility due to the emergence of other forms of hepatitis.10
- •
Face-to-face communication achieves better results than the use of prerecorded videos, information brochures, attendance at medical conferences or telephone consultations.11
- •
Sessions with continuing education groups have been demonstrated as a select way to follow up with most participants.12
Factors influencing the referral rate include the following:
- •
A request for analysis and the reception of a results system can influence the rate of referral. In the electronic health history, the results are highlighted by a system of visible alerts in a mailbox.
- •
Patients lacking a sense of disease (like inactive carriers of HBsAg) declined to be referred.
- •
A loss of derived cases, which decreases the observed referral rate, could be attributed to the group of pregnant women who are usually referred to an obstetrician.
In the present study, there may be several reasons why 76 cases (27%) were not referred to a hospital. The suspicion of liver disease and active drug or alcohol consumption, which determine the referral rate (> 90%), are significantly more frequent than cases of suspected inactive carriers (70%); this situation may partly be due to the persistence of the idea of a “healthy carrier” who does not require investigation. In fact, this denomination was collected as such in the health history of numerous cases. In the absence of previous liver disease or active addiction, the referral rates fall to 54% and 37%, respectively, which may reflect the idea of the absence of risk of disease in all patients who were considered to be “healthy carriers”.
Post-graduate education was considered to be the second leading useful source of information for improving physician awareness.6 Our study echoes a previous study that showed that in US disease centers, 4,727 patients from endemic areas in Africa and Asia underwent HBsAg analysis, and a lack of awareness of the disease and language barriers were the main factors influencing the effective derivation of HBsAg-positive patients.13 Moreover, the rate of patients effectively visiting outpatient offices in our study (one or more sessions was 91% versus without any sessions was 67%) significantly improved with peer-to-peer sessions in comparison to the previous study (66%). However, one study suggested that female physicians and single-handed practices, not physician training practices, were independent factors in the analyses of patient hepatitis C virus testing rates and positivity rates.7 Nevertheless, in order to increase the detection of HBsAg in primary care centers, it is fundamental to schedule peer-to-peer sessions that eliminate doubts about this pathology and clarify management options. Sometimes, interpretation of the serology test can be complex, and the detection of HBsAg enables the classification of patients into two types: positive “with suspected HBV” vs. negative “HBV is ruled out”. The inclusion of these recommendations, together with those of diagnostic and therapeutic management, is one of the fundamental pillars of the positive impact of these types of sessions. Previous experience in the detection of human immunodeficiency virus with tools of communication supports this approach.14
Peer-to-peer sessions for improving physicians’ understanding of HBV have a major impact compared to conventional education programs, campaigns, broadcasts, radio and community-based education. Improved understanding and knowledge initiated by physicians as a starting point not only increases serology requests but also provides a more vivid and comprehensive transmission of knowledge from physicians to HBsAg-positive patients, further enhancing the possibility of patients visiting outpatient offices for treatment and follow up. We anticipate that the effectiveness of peer-to-peer sessions can be amplified in African (8.83%)15 and East Asian (3.01%)15 populations relative to European (2.06%)15 and Spanish populations (0.7-1.68%)9 due to higher HBV prevalence in African and East Asian populations. Moreover, HBV infection is attributed to 60% of HCC cases in Africa and East Asia, whereas it is attributed to only 20% of cases in the developed Western world; therefore, the implementation of peer-to-peer sessions can achieve improved costeffectiveness.16 However, a critical concern for achieving the ultimate goal of HBV eradication and improved cost-effectiveness still remains as treatment and follow-up care may not be feasible in developed counties or low economic regions. Peer-to-peer sessions and education are the first programs to be cut when difficult economic times arise. Good funding allocation and the stretching of limited resources are required to maintain the sustainability of HBsAg care.
Several limitations are present. First, the HBsAg positivity rate of 0.873% in our study aligns with the rate in the study of Muñoz-Gámez JA, et al. (HBV prevalence in Spain);9 however, a relativity low prevalence might restrict the precision of the detection rate, referral rate and effective referral rate. Second, the present study was unable to calculate proportions instead of rates to illustrate the effective rate due to low prevalence. Finally, follow-up testing during medical evaluation to confirm HBV infection is recommended,17 even though the HBsAg test has high specificity.18
In summary, the present study revealed that peer-to-peer sessions increased the HBsAg detection rate and effective outpatient visitation rate, improving the continuity of care for hepatitis B.
Abbreviations- •
HBsAg: surface antigen of hepatitis B.
- •
HBV: hepatitis B virus.
- •
HCC: hepatocellular carcinoma.
None.
GrantsNone.
AcknowledgmentsThe authors wish to thank the clinical managers of the primary care, digestive disease and microbiology units for their support in this study.