Introduction and aim. We sought to identify independent risk factors for cirrhosis in HFE p.C282Y homozygotes in a cross-sectional study.
Material and methods. We evaluated 368 p.C282Y homozygotes who underwent liver biopsy and compared characteristics of those with and without cirrhosis. We performed multivariable logistic regression on cirrhosis with: age; sex; race/ ethnicity; diabetes; blood pints/units donated voluntarily; erythrocyte pints/units received; iron supplement use; alcohol intake, g/d; body mass index, kg/m2; swollen/tender 2nd/3rd metacarpophalangeal joints; elevated alanine aminotransferase; elevated aspartate aminotransferase; steatosis/fatty liver; iron removed by phlebotomy, g; and GNPATp.D519G positivity.
Results. Mean age of 368 participants (73.6% men) was 47 ± 13 (standard deviation) y. Cirrhosis was diagnosed in 86 participants (23.4%). Participants with cirrhosis had significantly greater mean age, proportion of men, diabetes prevalence, mean daily alcohol intake, prevalence of swollen/tender 2nd/3rd metacarpophalangeal joints, mean serum ferritin, elevated alanine aminotransferase, elevated aspartate aminotransferase, and mean iron removed; and significantly fewer mean blood pints/units donated. GNPATp.D519G positivity was detected in 82 of 188 participants (43.6%). In a multivariable model for cirrhosis, there were four significant positive associations: age (10-y intervals) (odds ratio 2.2 [95% confidence interval 1.5, 3.3]); diabetes (3.3; [1.1, 9.7]); alcohol intake (14 g alcohol drinks/ d) (1.5 [1.2, 1.8]); and iron removed, g (1.3 [1.2, 1.4]). There was no statistical evidence of two-way interactions between these variables.
Conclusion. In conclusion, cirrhosis in HFE p.C282Y homozygotes is significantly associated with age, diabetes, daily alcohol intake, and iron removed by phlebotomy, taking into account the effect of other variables.
Hemochromatosis is an autosomal recessive condition that is usually caused by homozygosity for the p.C282Y mutation (c.845G>A; rs1800562) of the HFE (high iron) gene (chromosome 6p21.3).1HFE p.C282Y homozygosity occurs in 0.3%-0.6% of persons of European descent and accounts for ~90% of hemochromatosis-related iron loading in Caucasians.1 Decreased hepcidin expression in p.C282Y homozygotes increases iron absorption.2 Although clinical penetrance of iron overload is mild in some p.C282Y homozygotes, severe iron overload occurs in other p.C282Y homozygotes and is complicated by arthropathy, diabetes, other endocrinopathy, cirrhosis, primary liver cancer, and cardiomyopathy.1
Cirrhosis is the major complication of iron overload in persons with hemochromatosis.1 Cirrhosis risk in persons with hemochromatosis and HFE p.C282Y homozygosity is greater with age,3,4 male sex,4,5 diabetes,6 alcohol consumption,7 and severe iron overload.4,8 Iron loading in p.C282Y homozygotes may also be modified by blood donation9,10 or oral iron supplements.11 No study of p.C282Y homozygotes has reported joint evaluation of these and other factors in a multivariable statistical model of cirrhosis risk.
We sought to evaluate a large cohort of HFE p.C282Y homozygotes who underwent liver biopsy (n = 368), to compare characteristics of those with (n = 86) and without (n = 282) cirrhosis, and to identify independent factors that influence cirrhosis risk. This sample size provides statistical power to estimate independent joint effects in a multivariable model. Available observations included: age at diagnosis; sex; race/ ethnicity; diabetes; lifetime whole blood pints/units donated; lifetime erythrocyte pints/units received as transfusion; use of iron supplements; daily alcohol intake; body mass index, kg/m2; swollen/tender 2nd/3rd metacarpophalangeal joints; serum ferritin; elevated alanine aminotransferase (ALT) activity; elevated aspartate aminotransferase (AST) activity; steatosis/ fatty liver; cirrhosis; and iron removed by phlebotomy to achieve iron depletion (QFe, g). We also determined the association of cirrhosis with positivity for glyceronephosphate O-acyltransferase (GNPAT) p.D519G (c.1556A>G; rs11558492; chromosome 1q42.2), a polymorphism associated with increased iron loading in p.C282Y homozygotes.12,13 We discuss the present results in the context of other reports of cirrhosis risk, iron phenotypes, and non-iron conditions in persons with hemochromatosis and p.C282Y homozygosity.
Materials and MethodsStudy performanceThis study was performed in accordance with the Declaration of Helsinki. Approval was obtained from institutional review boards at: University of California, Irvine; University of Western Ontario; QIMR Berghofer Medical Research Institute; Rochester General Health System; Cancer Council Victoria, Australia; University of Utah; and Department of Veterans Affairs Long Beach Healthcare System. All participants provided written informed consent. Consortium study sites identified HFE p.C282Y homozygotes in clinical practice settings associated with the authors or from population studies in which one or more of the authors are/were chief or principal investigators: 1) the Hemochromatosis and Iron Overload Screening (HEIRS) Study that recruited from five centers in North America; 2) the HealthIron study of genetic and environmental modifiers of hemochromatosis phenotypes in Melbourne, Victoria, Australia; 3) a screening study of American Red Cross blood donors conducted at the University of Utah; and 4) a study of the Prevalence of Iron Overload and Frequency of the Hemochromatosis Gene conducted at the Department of Veterans Affairs Long Beach Healthcare System.
Clinical and laboratory data collectionInformation was obtained from medical records of participants identified through clinical practices, from the National Institutes of Health BioLincc biorepository for HEIRS Study participants,12 the Melbourne Collaborative Cohort Study data and sample repository at the Cancer Council Victoria and University of Melbourne in Australia for the HealthIron study, and the University of Utah. A 72-question case report form was created and approved by study investigators before data collection commenced. Observations recorded at diagnosis of hemochromatosis included: age; sex; race/ethnicity; diabetes; lifetime pints/ units of whole blood voluntarily donated before diagnosis of hemochromatosis; lifetime pints/units of erythrocytes received as transfusion; use of iron supplements; daily alcohol intake, g; body mass index, kg/m2; swollen/tender 2nd/3rd metacarpophalangeal joints; serum ferritin; serum ALT; serum AST; steatosis/fatty liver; and cirrhosis. After participants achieved iron depletion by phlebotomy, QFe as defined previously12,14 was also recorded.
Most investigators submitted participant data to the Study Center via on-line case report forms and secure Research Electronic Data Capture Software (REDCap, Vanderbilt University, Nashville, TN, USA). University of Utah investigators submitted participant data via a REDCap importing file that permitted direct upload into the REDCap database. Responses to the REDCap cirrhosis item (yes or no) could be expanded in a text comments box. All investigators contributed to data review via conference calls and e-mails and re-consulted data sources for verification or amendments, as appropriate.
HFE p.C282Y and GNPAT p.D519G genotypingHFE p.C282Y homozygosity was diagnosed at referring institutions or in screening programs. Positivity for GNPAT p.D519G (heterozygosity or homozygosity) was detected with exome sequencing12 or single-nucleotide polymorphism analysis.15
Participant selectionInclusion criteria included: 1) HFE p.C282Y homozygosity; 2) liver biopsy data; and 3) consent to perform DNA analysis.
Diagnosis of hemochromatosis in p.C282Y homozygotes does not depend on the availability of liver biopsy specimens. Thus, recommendations that participants undergo liver biopsy to investigate possible cirrhosis or non-iron liver conditions were made on an individual basis. A total of 1,014 participants with p.C282Y homozygosity were enrolled in the present study, among whom were 418 participants whose cirrhosis status (Yes/No) was available. Of the 418 participants, a liver biopsy report was not available in 50 participants. After excluding these 50 participants, the analysis cohort consisted of 368 participants. Of these, 99 participants were diagnosed or treated by the present physician co-authors in five consortium centers and 269 other participants were diagnosed in screening programs. The 368 participants resided in the USA, Canada, and Australia.
Diagnosis of liver conditionsSteatosis/fatty liver was defined as a combination of three variables: steatosis or steatohepatitis reported by pathologists; history of fatty liver (yes, no); estimated daily alcohol consumption. We defined alcoholic steatosis/fatty liver as the combination of steatosis/fatty liver and consumption of > 60 g alcohol daily. To identify other liver conditions, we reviewed text comments for REDCap liver biopsy entries (available for 63 participants) and clinical practice documentation (all 368 participants). Liver biopsy specimens were interpreted by clinical pathologists at the respective participating institutions. Cirrhosis was defined as the histological occurrence of regenerating nodules of hepatocytes surrounded by bands of fibrous connective tissue.16
StatisticsWe used available observations for 368 participants. For participants who reported making voluntary blood donations of unknown number, we imputed a value of one pint/unit. For participants who reported that they received erythrocyte transfusions of unknown number, we imputed a value of one pint/unit. For participants without transfusion data, we imputed a value of zero pints/units. For some computations, we defined age as 10-y intervals and 14 g of pure ethanol as one alcohol drink-equivalent.17 We performed log10 transformation of serum ferritin values to determine geometric means.
Descriptive data are displayed as enumeration (n), percent (%), mean ± 1 standard deviation (SD), or odds ratio (OR) with 95% confidence interval [95% CI] obtained by inverting the Wald χ2 Test of the null hypothesis of no association. We compared characteristics of participants with and without cirrhosis using Fisher’s exact test or the Wilcoxon Rank-Sum test, and applied univariate logistic regression models. We used multivariable backward stepwise logistic regression to estimate the magnitude of the association between the diagnosis of cirrhosis (dichotomous dependent variable) and variables that possibly contribute to cirrhosis risk. For each predictor variable, observations with non-valid or missing responses were excluded from analyses. Quantitative variables included age at diagnosis; lifetime whole blood pints/units donated voluntarily; lifetime erythrocyte pints/units received as transfusion; mean daily alcohol intake, g; body mass index, kg/ m2; and QFe, g. Qualitative variables included sex; race/ ethnicity; diagnosis of diabetes; use of iron supplements (dichotomous); swollen/tender 2nd/3rd metacarpophalangeal joints; steatosis/fatty liver; elevated ALT activity; elevated AST activity; and GNPAT p.D519G positivity (homozygosity or heterozygosity). Serum ferritin and hepatic iron concentration, surrogates for storage iron, were not included in multivariable analyses because their positive correlations with QFe are significant. Elevated ALT activity and elevated AST activity were additional confounding variables and were also excluded from final multivariable logistic regression analyses.
Models were examined for the presence of interactions between age at presentation, diabetes, daily alcohol intake, and QFe. For continuously-valued exposure variables, we assumed that there is a linear relationship between the magnitude of the exposure and the log-odds of cirrhosis. Although this assumption indicates the correct direction of the association (increased or decreased cirrhosis risk), it does not exclude the possibility that the true relationship between exposure and cirrhosis risk is non-linear, investigation of which would require additional data. Other sources of potential bias include lack of available data for some variables in some participants and lack of participant recall of some data. We used SAS® v.9.4 (Statistical Analysis System, Cary, NC).
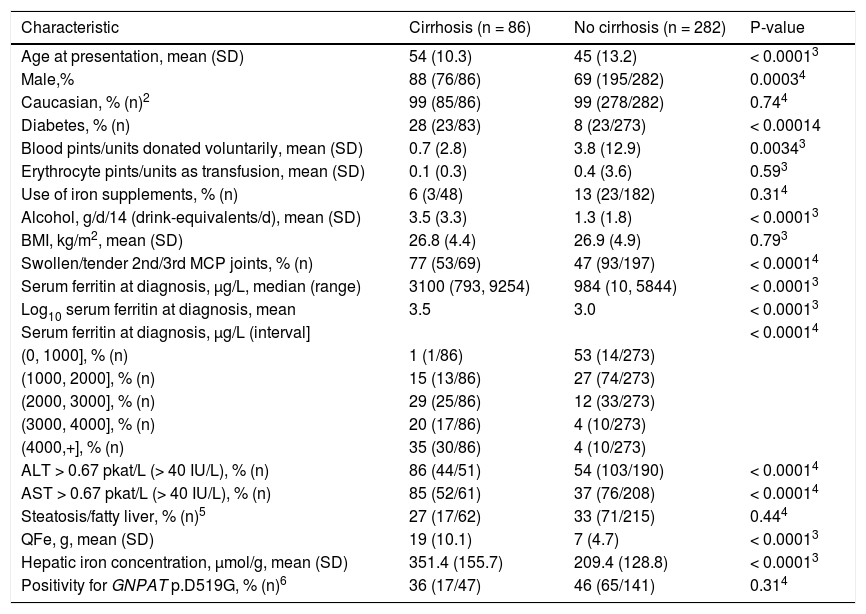
ResultsCharacteristics of participants at diagnosisOf 368 participants (73.6% men), 98.6% reported Caucasian race/ethnicity (Table 1). Mean age at hemochromatosis diagnosis was 47 ± 13 (SD) y. Forty-six of 356 participants (12.9%) were diagnosed to have diabetes. Mean pints/units of blood donated voluntarily was 3.1 ± 11.4 (range 0-118; 345 participants). Mean pints/units of erythrocytes received as transfusion was 0.3 ± 3.2 (range 0 - 54; 345 participants). Twenty-six of 230 participants (11.3%) reported using iron supplements. Mean daily alcohol intake was 1.9 ± 2.5 drink-equivalents (range 0-14.3; 333 participants).
Characteristics of 368 HFE C282Y homozygotes.1
| Characteristic | Cirrhosis (n = 86) | No cirrhosis (n = 282) | P-value |
|---|---|---|---|
| Age at presentation, mean (SD) | 54 (10.3) | 45 (13.2) | < 0.00013 |
| Male,% | 88 (76/86) | 69 (195/282) | 0.00034 |
| Caucasian, % (n)2 | 99 (85/86) | 99 (278/282) | 0.744 |
| Diabetes, % (n) | 28 (23/83) | 8 (23/273) | < 0.00014 |
| Blood pints/units donated voluntarily, mean (SD) | 0.7 (2.8) | 3.8 (12.9) | 0.00343 |
| Erythrocyte pints/units as transfusion, mean (SD) | 0.1 (0.3) | 0.4 (3.6) | 0.593 |
| Use of iron supplements, % (n) | 6 (3/48) | 13 (23/182) | 0.314 |
| Alcohol, g/d/14 (drink-equivalents/d), mean (SD) | 3.5 (3.3) | 1.3 (1.8) | < 0.00013 |
| BMI, kg/m2, mean (SD) | 26.8 (4.4) | 26.9 (4.9) | 0.793 |
| Swollen/tender 2nd/3rd MCP joints, % (n) | 77 (53/69) | 47 (93/197) | < 0.00014 |
| Serum ferritin at diagnosis, µg/L, median (range) | 3100 (793, 9254) | 984 (10, 5844) | < 0.00013 |
| Log10 serum ferritin at diagnosis, mean | 3.5 | 3.0 | < 0.00013 |
| Serum ferritin at diagnosis, µg/L (interval] | < 0.00014 | ||
| (0, 1000], % (n) | 1 (1/86) | 53 (14/273) | |
| (1000, 2000], % (n) | 15 (13/86) | 27 (74/273) | |
| (2000, 3000], % (n) | 29 (25/86) | 12 (33/273) | |
| (3000, 4000], % (n) | 20 (17/86) | 4 (10/273) | |
| (4000,+], % (n) | 35 (30/86) | 4 (10/273) | |
| ALT > 0.67 pkat/L (> 40 IU/L), % (n) | 86 (44/51) | 54 (103/190) | < 0.00014 |
| AST > 0.67 pkat/L (> 40 IU/L), % (n) | 85 (52/61) | 37 (76/208) | < 0.00014 |
| Steatosis/fatty liver, % (n)5 | 27 (17/62) | 33 (71/215) | 0.444 |
| QFe, g, mean (SD) | 19 (10.1) | 7 (4.7) | < 0.00013 |
| Hepatic iron concentration, µmol/g, mean (SD) | 351.4 (155.7) | 209.4 (128.8) | < 0.00013 |
| Positivity for GNPAT p.D519G, % (n)6 | 36 (17/47) | 46 (65/141) | 0.314 |
For each variable, observations with non-valid responses were excluded. SD: standard deviation. BMI: body mass index. MCP: metacarpophalangeal. ALT: alanine aminotransferase. AST: aspartate aminotransferase. QFe: quantity of iron removed by phlebotomy to achieve iron depletion.
One participant with biopsy-proven cirrhosis reported African-American race/ethnicity. One participant each without cirrhosis reported Native American, Asian, Pacific Islander, African-American, and multiple race/ethnicity.
Mean body mass index was 26.8 ± 4.8 kg/m2 (range 17.3-48.5; 235 participants). Swelling and/or tenderness of the 2nd/3rd metacarpophalangeal joints was reported in 146 of 266 participants (54.9%). ALT was elevated in 147 of 241 participants (61.0%). AST was elevated in 128 of 269 participants (47.6%). Mean serum ferritin was 4,047 ± 3,319 pmol/L (22-20,794; 359 participants).
Steatosis/fatty liver occurred in 88 of 287 participants (30.7%). One or more of the three variables we used to diagnose steatosis/fatty liver was missing in 91 participants. The prevalence of missing steatosis/fatty liver data did not differ significantly between participants with cirrhosis and participants without cirrhosis (27.9% (24/86) vs. 23.8% (67/282); p = 0.4757).
Cirrhosis was diagnosed in 86 of 368 participants (23.4%). Cirrhosis prevalence was greater in men than women (28.0% vs. 10.3%, respectively; p = 0.0004). Mean liver iron concentration was 238 ± 146 µmol/g dry weight (range 9-847; n = 262). Mean liver iron concentration was significantly greater in participants with cirrhosis than in those without cirrhosis (Table 1). The prevalence of alcoholic steatosis/fatty liver was greater in participants with cirrhosis than participants without cirrhosis (21.0% (13/62) vs. 7.0% (15/215); p = 0.0031). Mean QFe was 10.1 ± 8.2 g (range 0.5-50; n = 307). One participant without cirrhosis was diagnosed to have hepatitis C. Another participant without cirrhosis was diagnosed to have “acute hepatitis.” A participant with cirrhosis was diagnosed to have extensive hepatic sarcoidosis.
GNPAT p.D519GGNPAT p.D519G was detected in 82 of 188 participants (43.6%; 13 homozygotes, 69 heterozygotes; allele frequency 0.25).
Participants with cirrhosisMean age at diagnosis, proportion of men, prevalence of diabetes, mean daily alcohol intake, prevalence of swollen/tender 2nd/3rd metacarpophalangeal joints, mean serum ferritin, elevated ALT, elevated AST, and mean QFe were significantly greater in participants with cirrhosis. Mean blood pints/units donated voluntarily was significantly lower in participants with cirrhosis (Table 1).
Multivariable logistic regression on cirrhosisRegression on cirrhosis revealed four significant positive associations: age; diabetes; alcohol drink-equivalents/d; and QFe (Table 2). There was no significant association of cirrhosis with other variables, including sex and GNPAT p.D519G positivity, after inclusion of these significant four variables. There was no statistical evidence of two-way interactions between age, diabetes, alcohol drink-equivalents/d, and QFe.
Independent variables in a multivariable logistic regression on cirrhosis in 274 HFE p.C282Y homozygotes.*
| Variable | p-value of Wald χ2 test | Odd ratio | 95% Wald confidence limits | |
|---|---|---|---|---|
| Age at diagnosis/10 (10-y increments) | 0.0001 | 2.2 | 1.5 | 3.3 |
| Diabetes | 0.034 | 3.3 | 1.1 | 9.7 |
| Daily alcohol consumption, g/14 (drinks/d) | 1.5 × 10-5 | 1.5 | 1.2 | 1.8 |
| QFe, g | 4.3 × 10-11 | 1.3 | 1.2 | 1.4 |
Area under the curve = 0.92. We used the independent variables which differed significantly between participants with and without biopsy-proven cirrhosis in univariate logistic models (p < 0.05): age at diagnosis; sex; diabetes; blood pints/units donated; alcohol consumption; tender/swollen 2nd/3nd metacarpophalangeal joints; and quantity of iron removed by phlebotomy to achieve iron depletion (QFe).
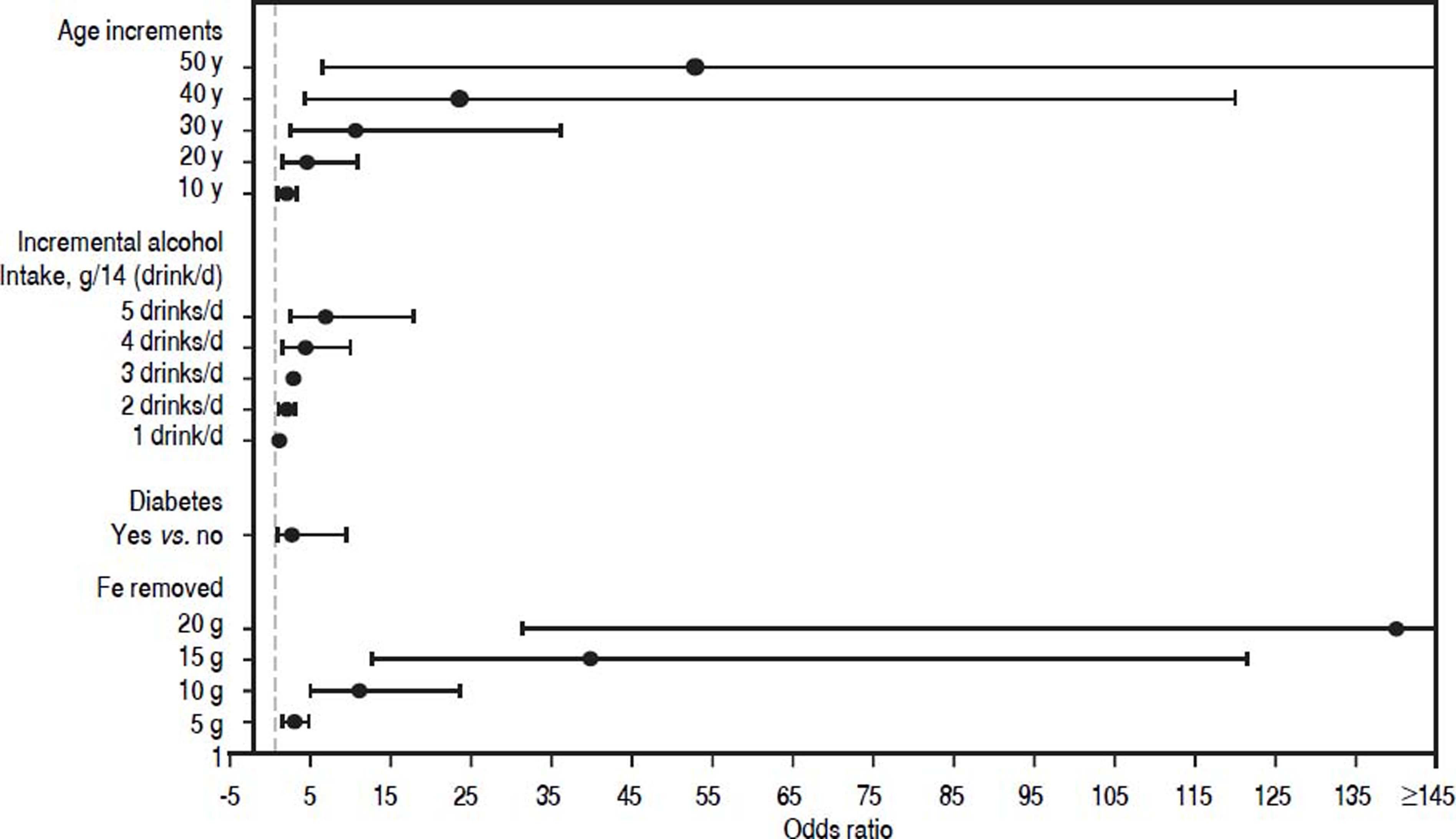
The OR for continuous predictor variables age at diagnosis (10-y intervals), daily alcohol intake (g), and QFe (g) represents the increased odds of cirrhosis for each one unit increase in each individual predictor variable, adjusted for the presence of the remaining predictors (Table 2). As shown in Figure 1, the odds of cirrhosis is 4.9-fold higher [95% CI 2.4, 10.0] with daily alcohol intake of 4 drinks/d than that of no alcohol intake, adjusted for age at diagnosis, diabetes, and QFe. For an estimated daily alcohol intake of 5 drinks/d, the odds of cirrhosis increases 7.3-fold [95% CI 3.0, 17.8], adjusted for the additional predictors. In participants whose QFe was 10 g, the odds of cirrhosis increases 11.8-fold [95% CI 5.7, 24.5]. In participants whose QFe was 15 g, the odds of cirrhosis increases by 40.5-fold [95% CI 13.5, 121.6], adjusted for age at diagnosis, daily alcohol intake, and diabetes. The occurrence of diabetes increases the odds of cirrhosis 3.3-fold [95% CI 1.1, 9.7], adjusted for the presence of the remaining predictors (Table 2).
Odds ratios (black dots) and 95% confidence intervals for prediction of cirrhosis. The odds ratios for the continuous predictor variables including age increments since diagnosis (10 y intervals), incremental alcohol intake (g/14 (drink/d)), and additional iron removed to achieve iron depletion (g) represent the increased risks of biopsy-proven cirrhosis for the indicated increase in each individual predictor variable, adjusted for the presence of the remaining predictors. The diagnosis of diabetes aso increases cirrhosis risk, adjusted for the presence of the remaining predictors.
Cirrhosis in this cohort of 368 HFE p.C282Y homozygotes was associated with four significant independent variables: age; diabetes; alcohol drink-equivalents/d; and QFe. There was no statistical evidence of two-way interactions between these four variables. Progressive increments of each of the three continuous variables were associated with progressive increments in cirrhosis risk, taking into account the effect of diabetes. The diagnosis of diabetes also increases cirrhosis risk, taking into account the effect of the three continuous variables. Altogether, the large sample size of the present study permitted the ascertainment of significant independent variables that contribute to cirrhosis risk and pathogenesis that were previously suggested by analyses of smaller cohorts.3,8
Greater age at diagnosis of hemochromatosis was significantly associated with greater cirrhosis risk in the present multivariable logistic regressions. In other studies of HFE p.C282Y homozygotes, cirrhosis was diagnosed only those aged > 40 y.3,8 In a retrospective study of 60 patients with hemochromatosis, risk of high-grade hepatic fibrosis increased with greater age at diagnosis.18 In 182 patients with hemochromatosis phenotypes, advanced hepatic fibrosis was significantly associated with age, after adjustment for HFE genotype and other variables.5 In a study of patients with hemochromatosis phenotypes reported before the discovery of HFE, those with cirrhosis were significantly older than those without cirrhosis.19
The prevalence of cirrhosis in the present men with HFE p.C282Y homozygosity was more than two-fold greater than that of the women in univariate analyses. In 182 patients with hemochromatosis phenotypes, advanced hepatic fibrosis was significantly associated with male sex, after adjustment for HFE genotype and other variables.5 In two studies of persons with hemochromatosis phenotypes reported before the discovery of HFE, the prevalence of cirrhosis in men was also significantly greater than that in women.19,20 Heavy alcohol consumption did not account for the difference between men and women.19,20 The unexpected finding that male sex was not independently associated with cirrhosis in the present multivariable analyses could be explained in part by either a greater prevalence of presenting manifestations in women, suggesting that liver biopsy was indicated, or a greater prevalence of previously unsuspected cirrhosis in women than men.
The prevalence of diabetes was more than three-fold higher in the present participants with cirrhosis than in those without cirrhosis. In a report of 291 other HFE p.C282Y homozygotes selected because they underwent liver biopsy, diabetes was associated with increasing hepatic fibrosis stage independent of male sex, alcohol consumption, and iron loading.6 In a study of 159 consecutive referred hemochromatosis probands with p.C282Y homozygosity, cirrhosis was not significantly associated with diabetes in multivariable regressions.14
The mean number of donated blood pints/units was significantly lower in the present participants with cirrhosis than without cirrhosis, although the mean number was relatively low in both participant subgroups. The numbers of blood pints/units voluntarily donated before diagnosis of hemochromatosis were not significantly associated with cirrhosis in multivariable logistic regressions. In a previous study of HFE p.C282Y homozygotes, numbers of blood units donated before diagnosis of hemochromatosis were not significantly related to numbers of therapeutic phlebotomy units required to achieve iron depletion.9 In another study, there was no significant difference in mean self-reported serum ferritin at diagnosis of hemochromatosis in non-screening probands with p.C282Y homozygosity who were or were not volunteer blood donors before diagnosis.21 In the present and previous studies,9,21 the proportions of persons who voluntarily donated blood before hemochromatosis diagnosis were small.
Use of iron supplements was reported by 11% of the present participants, consistent with a survey of a large number of hemochromatosis patients.22 The present analyses did not detect a significant association of cirrhosis with reports of supplemental iron use. In a previous study of 213 screening study participants with HFE p.C282Y homozygosity, there was no significant relationship between serum ferritin levels and reports of supplemental iron use.23
Greater daily alcohol intake was significantly associated with greater cirrhosis risk in the present univariate and multivariable analyses. In 224 HFE p.C282Y homozygotes without viral hepatitis or non-alcoholic steatohepatitis reported previously, the prevalence of cirrhosis was nine-fold greater in those who consumed ≥ 60 g of alcohol daily than in those who consumed less than this amount.7 In a study of 291 p.C282Y homozygotes, there was a significant positive association of heavy alcohol intake with hepatic fibrosis stage.24 In two reports published before the discovery of HFE, heavy alcohol intake by persons with hemochromatosis was associated with greater cirrhosis risk.19,25
The prevalence of either elevated ALT or elevated AST was significantly greater in participants with cirrhosis than without, although neither elevated ALT nor elevated AST was significantly associated with cirrhosis in multivariable logistic regressions. Elevated AST in patients with hemochromatosis and iron overload is typically associated with hepatic injury, especially cirrhosis.26 In a study of 197 patients with HFE p.C282Y homozygosity, the absence of severe hepatic fibrosis was associated with the combination of serum ferritin ≤ 2,247 pmol/L, lack of hepatomegaly, and normal serum AST.8
Steatosis/fatty liver was not significantly associated with cirrhosis in this study, although the prevalence of cirrhosis was three-fold greater in participants with steatosis/ fatty liver who also consumed > 60 g alcohol daily than in participants with steatosis/fatty liver whose daily alcohol consumption was ≤ 60 g. It is possible that morphologic evidence of hepatic steatosis disappeared in some participants before their respective liver biopsy specimens revealed cirrhosis. In another study, 41% of 214 patients with hemochromatosis and HFE p.C282Y homozygosity had biopsy-proven steatosis that was independently associated with male sex, excess alcohol intake, hepatic iron content, and fibrosis.27 In a study of 291 p.C282Y homozygotes, increasing fibrosis stage revealed a significant positive association with “any steatosis.”24
Cirrhosis was significantly associated with QFe in the present multivariable regressions. Previous studies concluded that persons with cirrhosis and hemochromatosis phenotypes with or without demonstration of HFE p.C282Y homozygosity typically have severe hepatic siderosis.3,5,8,19,28
The proportion of the present participants with GNPAT p.D519G positivity did not differ significantly between those with and without cirrhosis. Similarly, allele frequencies of p.D519G in Italian hemochromatosis patients with absent/mild fibrosis and severe fibrosis/ cirrhosis did not differ significantly.29 In contrast, cirrhosis was significantly associated with the patatin-like phospholipase domain-containing-3 (PNPLA3) I148M polymorphism (rs738409) in Italian patients with hemochromatosis and p.C282Y homozygosity whose body mass index was < 25 kg/m2.30PCSK7 (proprotein convertase subtilisin/kexin type 7) rs236918 C allele was a risk factor for cirrhosis in 244 German and Austrian/ Swiss31and 187 Italian32 patients with hemochromatosis and p.C282Y homozygosity, but not 112 Swedish patients with hemochromatosis and p.C282Y homozygosity.31
A strength of the present study is that this is the largest cohort for cirrhosis in hemochromatosis in which all participants were demonstrated to be HFE p.C282Y homozygotes and underwent liver biopsy. Limitations of the present data include missing responses, non-valid data, and lack of observations. Our review of REDCap liver biopsy text entries and clinical practice documentation indicates that the proportion of p.C282Y homozygotes who had hepatitis C and other non-iron liver conditions unrelated to alcohol consumption and non-alcoholic steatosis/fatty liver that may increase cirrhosis risk is small. The present results cannot confirm or exclude the possibility that the independent variables we identified also influence lesser degrees of hepatic injury than cirrhosis interpreted as fibrosis stages 1, 2, or 3. The present study was not designed to evaluate the association of cirrhosis with alleles other than GNPAT p.D519G. Longitudinal evaluation of survival and risk of primary liver cancer in the present cohort was beyond the scope of this study.
ConclusionsCirrhosis in HFE p.C282Y homozygotes is significantly associated with age, diabetes, daily alcohol intake, and iron removed by phlebotomy, taking into account the effect of other variables.
Abbreviations- •
ALT: alanine aminotransferase.
- •
AST: aspartate aminotransferase.
- •
CI: confidence interval.
- •
GNPAT: glyceronephosphate O-acyltransferase gene.
- •
HFE: high iron gene.
- •
OR: odds ratio.
- •
QFe: quantity of iron (g) removed by phlebotomy to achieve iron depletion.
- •
SD: standard deviation.
The authors recognize and appreciate financial support in part by grant 1R24DK093433-01 from the National Institute of Diabetes and Digestive and Kidney Diseases, grant P30 CA-62203 from the National Cancer Institute, and funds from the Department of Veterans Affairs. V.N.S. and G.A.R. are supported by Senior Research Fellowships from the NHMRC of Australia. J.C.B. is supported in part by Southern Iron Disorders Center.
Author ContributionsAll authors contributed equally to this work. J.C.B. conceived the study and drafted the manuscript. J.C.B., P.D.P., P.C.A., L.W.P., V.N.S., J.D.P., C.J.P., and G.D.M. contributed samples and data. C.E.M. and M.J.E. provided design and analysis oversight. C.E.M., W.P.C., G.D.M., J.C.B., and M.J.E. reviewed and approved the final dataset for analysis. W.P.C., C.E.M., and M.J.E. tabulated outcomes and performed statistical analyses. C.E.M., M.J.E., G.A.R., G.J.A., L.W.P., V.N.S., P.C.A, P.D.P., L.C.G., J.D.P., C.J.P., and G.D.M. contributed to the manuscript.
DisclosuresNone of the authors has a conflict of interest to report.