Gastrointestinal foreign bodies are commonly encountered in clinical practice. However, although perforation of the gastrointestinal tract by a foreign body is not unusual, the formation of a hepatic abscess as a result of the migration of a foreign body is extremely rare. Patients usually present with atypical symptoms, and the treatment of such pyogenic liver abscesses presents a challenge. Here we report a case of hepatic abscess secondary to stomach perforation by a fish bone.
Gastrointestinal foreign bodies are commonly encountered during clinical practice. Although most foreign bodies do not cause any clinical symptoms, some may cause gastrointestinal tract bleeding and perforation as a result of blockage of the gastrointestinal tract and physiological stenosis. Pyogenic hepatic abscess is a common clinical emergency involving suppurative liver infection caused by bacterial invasion of the liver parenchyma, usually as a result of biliary tract diseases. The classic indicators of hepatic abscess include epigastric pain, and fever with chills and jaundice. However, hepatic abscesses arising as a result of foreign body perforation of the gastrointestinal tract are extremely rare, and clinical experience in their diagnosis and treatment is therefore lacking.
Case ReportA 34-year-old Chinese woman presented with an 8-day history of progressively increasing epigastric pain. She had a history of hypertension and was being treated with felodipine (2.5 mg/day), but had no history of diabetes, surgery, or trauma. She had initially complained of epigastric pain located in the upper left abdominal quadrant and xiphoid process 8 days before admission. The pain was associated with asthenia, anorexia, nausea, vomiting, and mild fever. The patient reported no history of chills, thoracic pain, jaundice, lumbago, or respiratory or urinary complaints.
On physical examination, her general state of health was normal, acyanotic, anicteric, febrile (39.1°C), and eupneic. Her blood pressure was 125/94 mmHg and her pulse rate was 110 beats/min. Her abdomen was soft and the xiphoid process and left upper quadrant were tender, with muscle guarding and no rebound tenderness. No masses or collateral circulation were palpable. Her liver and spleen were not palpable.
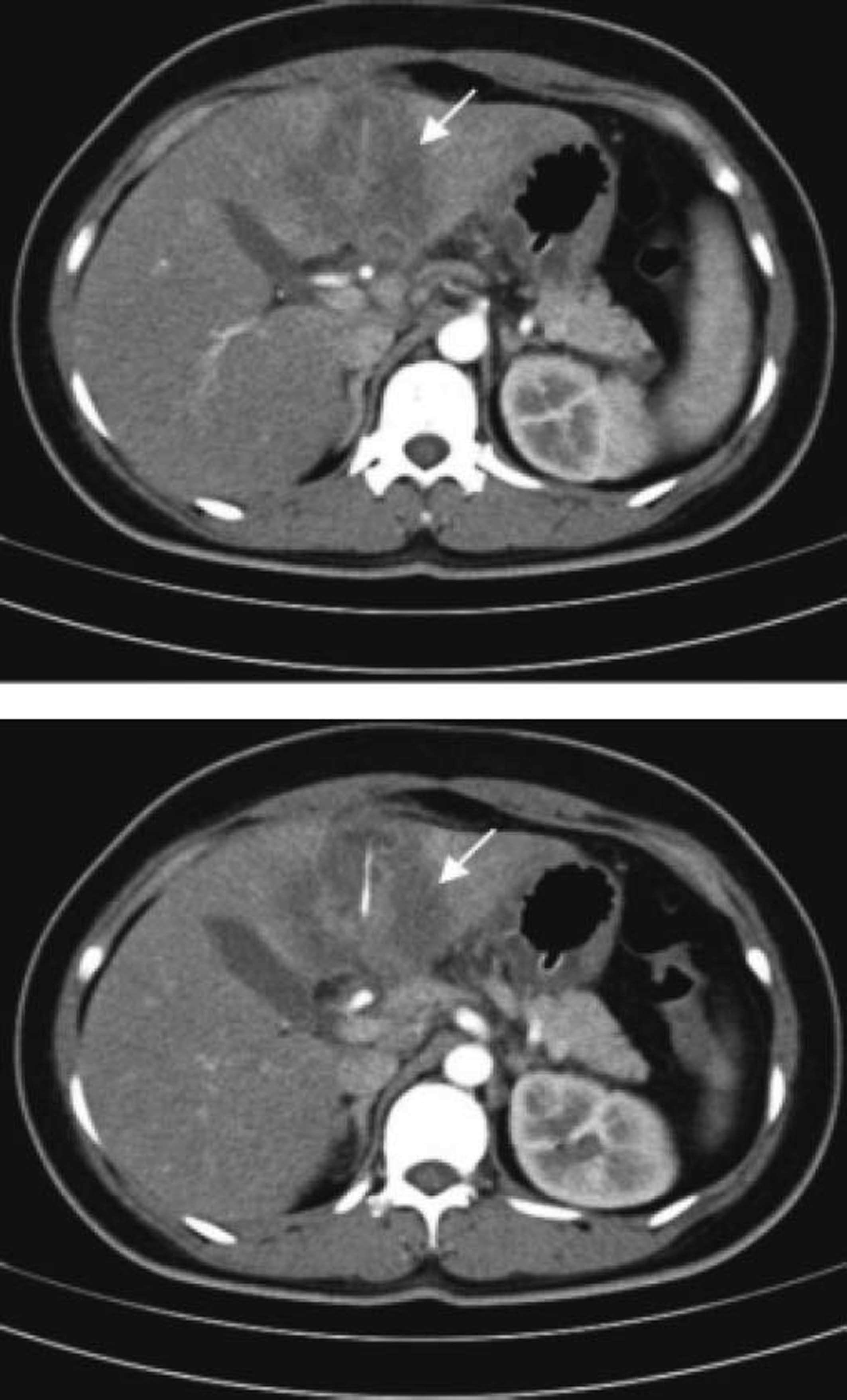
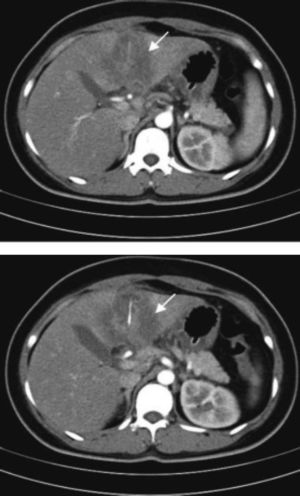
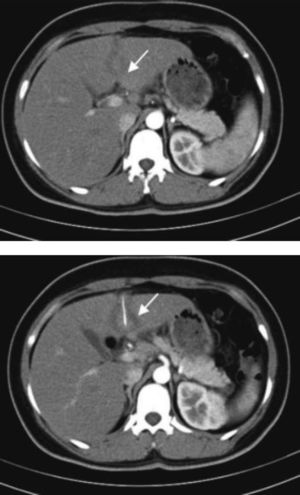
The results of laboratory tests were as follows: white cell count 18.59 × 109/L; neutrophils% 86.9%; C-reactive protein 226.2 mg/L; and erythrocyte sedimentation rate115 mm/h. Hepatic laboratory tests revealed normal levels of liver enzymes and bilirubin. Standard abdominal X-ray results were normal. Contrast-enhanced computed tomography (CT) of the upper abdomen revealed a left-sided solid liver abscess, with a straight, hyperdense feature ~3.0 cm long at the centre, and gastric wall thickening at the antrum (Figure 1). Upper gastrointestinal endoscopy showed no perforation or foreign body. The diagnosis at that point was a hepatic abscess of unclear aetiology and the patient was started on antibiotic therapy (rocephin combined with tinidazole).
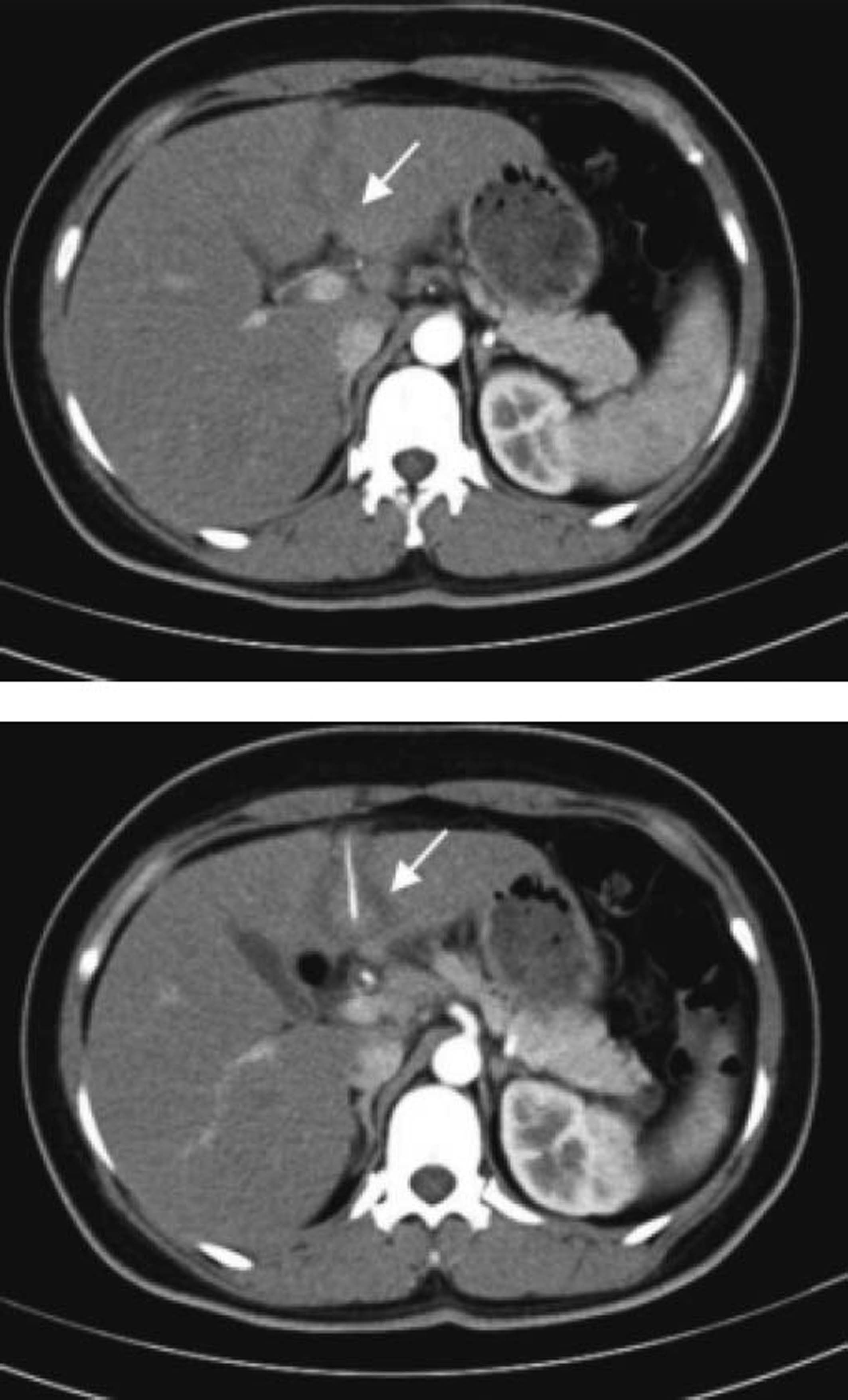
The patient’s epigastric pain had improved and her blood culture showed no abnormalities after 5 days of treatment, and routine blood tests, C-reactive protein, and erythrocyte sedimentation rate were normal after 3 weeks of treatment. Repeat contrast-enhanced CT scan of the upper abdomen revealed that the left-sided liver abscess had narrowed after treatment, but the straight, hyperdense feature at the centre of the liver abscess remained (Figure 2). The patient agreed to undergo exploratory laparoscopy to determine the nature and origin of the foreign body. The sagittal part of the left lateral lobe of the liver was found to adhere closely to the stomach wall and the retina, and was difficult to separate under endoscopy, and the foreign body could not be located. Exploratory laparotomy was then carried out and ultrasound revealed a slightly hyperechoic foreign body in the proximal sagittal part of the left hepatic lobe, partially exposed to the left lateral fissure of the liver. The foreign body was removed from the liver and subsequently identified as a fish bone (Figure 3). Upon careful retrospective anamnesis, the patient denied knowingly ingesting any foreign bodies, but remembered experiencing severe epigastric pain 2 weeks prior to admission, though this pain had rapidly resolved without any specific treatment. The patient’s recovery was uneventful and she was discharged on postoperative day 7.
Gastrointestinal foreign bodies are common in the clinic. However, > 80% of gastrointestinal foreign bodies pass through the gastrointestinal tract within 1 week, and their discharge can also be aided by endoscopic technologies.1 Only 1% of gastrointestinal foreign bodies cause gastrointestinal perforation, with 71% of such perforations occurring in the peritoneal cavity.2 Perforation by a foreign body leading to a hepatic abscess is thus extremely rare.
Lambert reported the first case of a hepatic abscess caused by gastrointestinal tract perforation by a foreign body in 18983 and 40 cases have been reported during the last 10 years. The formation of hepatic abscesses due to foreign body gut perforation is becoming increasingly recognized,4 and some investigators have thus suggested that this “rare condition should be kept in mind when dealing with cases of hepatic abscess or even septic shock of unknown origin”.5 However, many hepatic abscesses secondary to perforation are still being misdiagnosed as cryptogenic.
Most patients’ symptoms are subtle, and few present with the classic indicators of hepatic abscess. Fever with chills, abdominal pain, and jaundice are the most common presenting symptoms,6 and none of the patients have reported ingesting foreign objects.
Pointed or sharp objects such as sewing needles, toothpicks, chicken or fish bones, and pens often cause gastrointestinal perforation,7 with the stomach being the most common site of perforation. Peristaltic waves in the stomach gradually cause the foreign body to penetrate the mucosa of the thicker gastric wall, while the omentum and neighbouring organs progressively surround and seal the perforation.8 Although most liver abscesses due to foreign bodies are caused by direct penetration of a foreign body through the gastrointestinal tract,6 Martin and Rete reported a case of hepatic abscess following haematogenous transmission following rectal foreign body perforation.9 Because of its anatomical location, the left hemi-liver is the most commonly affected.6
Routine laboratory examinations cannot provide any specific diagnostic information,10 and ultrasound is usually the first choice, due to its ease of access.9 However, compared with ultrasound, CT demonstrates a sensitivity as high as 90%.10 Imaging examinations may locate the foreign body, such as a fish bone, which is often expressed as a linear structure of calcification.11
Gastroscopy or ultrasonic gastroscopy may be used to locate digestive tract foreign bodies during the early stage of perforation, when the foreign body has not fully penetrated the gastric wal.12 The treatment of hepatic abscesses includes antibiotic therapy, percutaneous drainage, and surgery. In the case of hepatic abscesses caused by foreign bodies, it is necessary to remove the foreign body surgically; the foreign body is taken out and the abscess drained, and the gastrointestinal tract perforation can be repaired.
In the current case, there was no history of foreign body ingestion or surgical trauma, and the patient presented at the hospital because of abdominal pain. The CT results were valuable for making a diagnosis in this patient by revealing a hepatic abscess in the left lobe of the liver, including a linear calcified structure. The CT scan also suggested thickening of the gastric wall at the antrum. Although upper gastrointestinal endoscopy showed no perforation or foreign body, based on CT and surgical results, which revealed the sagittal part of the left lateral lobe of the liver adhering closely to the stomach wall and the retina, we concluded that the fish bone was likely to have perforated the gastric antrum completely and then moved to the left lobe of the liver, resulting in the formation of a hepatic abscess. Because the fish bone had perforated the gastric wall completely and migrated into the liver, it was hard to locate the bone during surgery, and we therefore used ultrasound to locate the foreign body during the operation.
ConclusionClinicians encountering patients with a hepatic abscess of unknown origin must take a thorough history and examine the clinical evidence carefully to avoid potential misdiagnosis or missed diagnosis. Although antibiotic treatment may temporarily relieve the symptoms of hepatic abscess caused by a foreign body, surgical removal of the foreign body represents the best treatment plan.