The role of hepatologists in the management of hepatocellular carcinoma (HCC) is not well defined. We conducted a cross-sectional study to assess the feasibility of hepatology-directed HCC treatment.
PatientsWe evaluated 107 patients with newly diagnosed HCC, undergoing locoregional therapy as the first therapy between January 2017 and February 2019.
ResultsThe hepatologist directly participated in most of the microwave ablations. This descriptive cross-sectional study reveals the feasibility of the hepatologist-directed thermal ablation therapy, with decent outcome including response rate.
ConclusionsHepatologists can play a key role in the management of HCC in the current era of multidisciplinary team approach. Training fellows in performing ultrasound guided thermal ablation techniques would be one step forward in this direction.
There have been global efforts to manage hepatocellular carcinoma (HCC) cases in a multidisciplinary team setting [1]. More recently, this has been broadened to the concept of ‘Transplant Oncology’: multiple disciplines of transplantation medicine and oncology for the comprehensive management and research of hepatobiliary tumors are encompassed [1–7]. Involvement of hepatologists in the management of HCC would lead to reduction in mortality [7]. However, the role of hepatologists in the setting HCC continues to remain uncertain.
We published preliminary data on hepatology-directed HCC treatment using ultrasound-guided thermal ablation technique which one the authors (Tomohiro Tanaka), a hepatologist, directly administered [6]. We now present our data of the cross-sectional study on hepatology-directed management of HCC.
2MethodsWe conducted a descriptive cross-sectional study of 107 patients with newly diagnosed HCC, undergoing locoregional therapy (LRT) as a first therapy and one follow up imaging. Those who underwent other treatment modalities for HCC (such as surgical resection or systemic chemotherapy) or those who did not have the first follow up imaging within 3 months after LRT were not included. LRT included microwave ablation, Trans arterial chemoembolization, Trans arterial radioembolization or Stereotactic body radiation therapy done in an academic tertiary institution with a multi-organ transplant program in the U.S. Midwest between January 2017 to February 2019. There were three referral pathways: an internal referral from hepatologists to oncologists (H/O-group, n=62), outside referral directly to oncologists (O-group, n=24), and hepatologist-directed management (H-group, n=21). We have multiple channel of referrals, and generally the service which received the referrals manage the initial management of HCC.
The hepatologist (Tomohiro Tanaka) performed all microwave ablations in H-group. Those ablative procedures were provided as a corroborative work with the Division of Interventional Radiology: Professional charges were divided equally amongst the two services according to the primary practitioner; the rest of the LRTs were performed either by interventional radiology or radiation oncology [6]. Response was evaluated by modified response evaluation criteria in solid tumor (mRECIST) [8].
As documented elsewhere [6], the hepatologist performing thermal ablation (TT), completed a Gastroenterology/Hepatology fellowship at a high-volume tertiary care center in Japan [9], which included hands-on teaching of ablative techniques for liver tumors under the direct supervision of experienced hepatologists. TT had completed over 120 ablations upon completion of this 3-year fellowship, and got certified for independent practice in performing the procedures. This certification was accepted by the University of Iowa Credentialing Committee in December 2016.
A multidisciplinary team conference (MDTC) to conduct evidence-based discussion for the management of hepato-pancreato-biliary tumors was established in our institution in 2012. The committee consists of hepatobiliary surgeons (who also perform liver transplantations), hepatologists, medical oncologists, body imaging radiologists, interventional radiologists, and radiation oncologists. Most HCC patients included in our study were presented at this weekly MDTC, but some patients were discussed with the sub-specialists outside the setting of MDTC. This current study was approved by the University of Iowa institutional review board (#201708797).
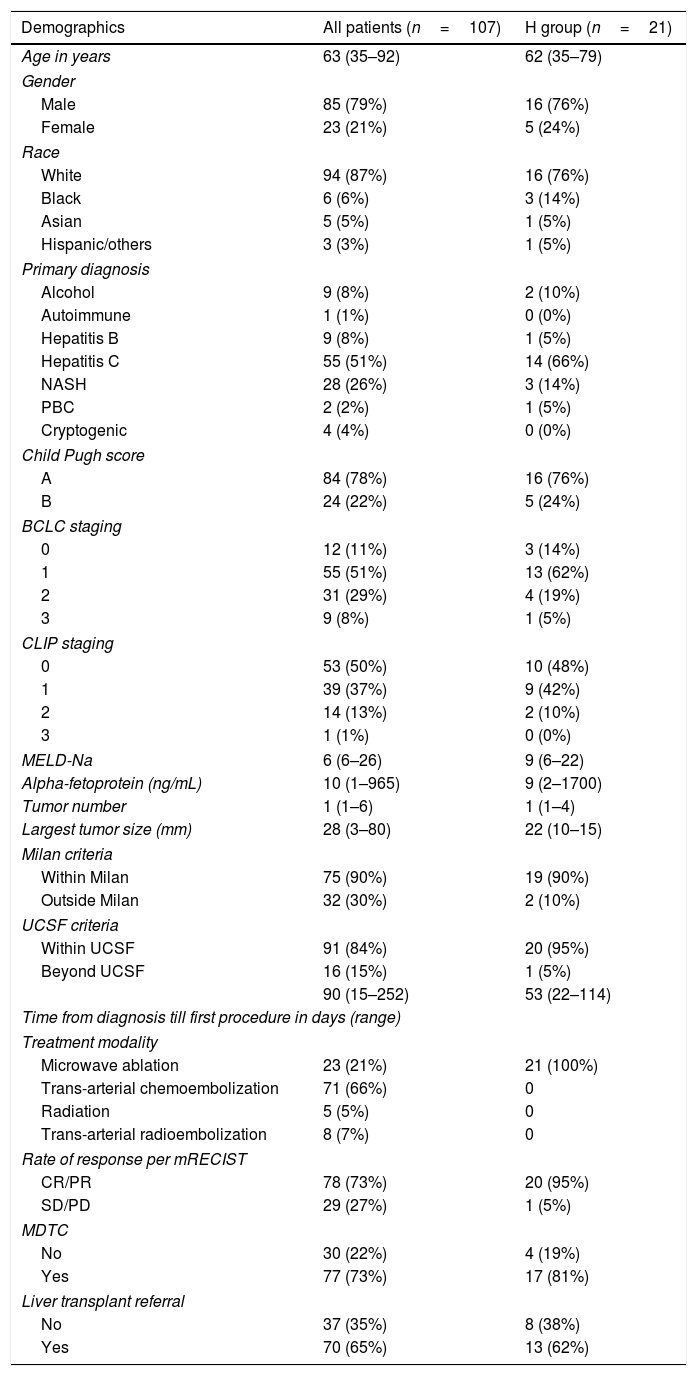
3ResultsThe characteristics of the patients are summarized in Table 1. The hepatologist performed 21 cases of MWA for HCC, out of all the 107 cases who underwent LRT. In H-group, 76% were in Barcelona clinic liver cancer (BCLC) stage 0–1, 90% were within Milan criteria, 95% were within University of California San Francisco (UCSF) criteria, 81% cases were discussed in MDTC, and 62% were refeed for liver transplantation. None of the patients in this group experienced adverse events associated with the ablation. Follow up imaging showed 95% (20/21) achieved a complete or partial response, most of which (92%) was complete response.
Patient characteristics.
| Demographics | All patients (n=107) | H group (n=21) |
|---|---|---|
| Age in years | 63 (35–92) | 62 (35–79) |
| Gender | ||
| Male | 85 (79%) | 16 (76%) |
| Female | 23 (21%) | 5 (24%) |
| Race | ||
| White | 94 (87%) | 16 (76%) |
| Black | 6 (6%) | 3 (14%) |
| Asian | 5 (5%) | 1 (5%) |
| Hispanic/others | 3 (3%) | 1 (5%) |
| Primary diagnosis | ||
| Alcohol | 9 (8%) | 2 (10%) |
| Autoimmune | 1 (1%) | 0 (0%) |
| Hepatitis B | 9 (8%) | 1 (5%) |
| Hepatitis C | 55 (51%) | 14 (66%) |
| NASH | 28 (26%) | 3 (14%) |
| PBC | 2 (2%) | 1 (5%) |
| Cryptogenic | 4 (4%) | 0 (0%) |
| Child Pugh score | ||
| A | 84 (78%) | 16 (76%) |
| B | 24 (22%) | 5 (24%) |
| BCLC staging | ||
| 0 | 12 (11%) | 3 (14%) |
| 1 | 55 (51%) | 13 (62%) |
| 2 | 31 (29%) | 4 (19%) |
| 3 | 9 (8%) | 1 (5%) |
| CLIP staging | ||
| 0 | 53 (50%) | 10 (48%) |
| 1 | 39 (37%) | 9 (42%) |
| 2 | 14 (13%) | 2 (10%) |
| 3 | 1 (1%) | 0 (0%) |
| MELD-Na | 6 (6–26) | 9 (6–22) |
| Alpha-fetoprotein (ng/mL) | 10 (1–965) | 9 (2–1700) |
| Tumor number | 1 (1–6) | 1 (1–4) |
| Largest tumor size (mm) | 28 (3–80) | 22 (10–15) |
| Milan criteria | ||
| Within Milan | 75 (90%) | 19 (90%) |
| Outside Milan | 32 (30%) | 2 (10%) |
| UCSF criteria | ||
| Within UCSF | 91 (84%) | 20 (95%) |
| Beyond UCSF | 16 (15%) | 1 (5%) |
| 90 (15–252) | 53 (22–114) | |
| Time from diagnosis till first procedure in days (range) | ||
| Treatment modality | ||
| Microwave ablation | 23 (21%) | 21 (100%) |
| Trans-arterial chemoembolization | 71 (66%) | 0 |
| Radiation | 5 (5%) | 0 |
| Trans-arterial radioembolization | 8 (7%) | 0 |
| Rate of response per mRECIST | ||
| CR/PR | 78 (73%) | 20 (95%) |
| SD/PD | 29 (27%) | 1 (5%) |
| MDTC | ||
| No | 30 (22%) | 4 (19%) |
| Yes | 77 (73%) | 17 (81%) |
| Liver transplant referral | ||
| No | 37 (35%) | 8 (38%) |
| Yes | 70 (65%) | 13 (62%) |
Abbreviations: hepatologist-directed management (H-group), Nonalcoholic steatohepatitis (NASH), Primary Biliary Cholangitis (PBC), Barcelona clinic liver cancer (BCLC), University of California San Francisco (UCSF), modified response evaluation criteria in solid tumor (mRECIST), Complete Response (CR), Partial Response (PR), Stable Disease (SD), Progressive Disease (PD).
The establishment of a multidisciplinary team approach for management of HCC is crucial [1]. One of the goals would be to set-up a multidisciplinary HCC clinic [5], or at least have a regular discussion as a multidisciplinary team regarding the management of HCC patients [3,4]. Given the emerging idea of transplant oncology, hepatologists are expected to play a major role in the management of HCC [2]. Our cross-sectional study described favorable profile of the patients that were dealt with the direct involvement of hepatologists, thus suggesting that the involvement of hepatologists can lead to better access to appropriate HCC management down the road.
Our data shows a potential extension of the role of hepatologists in HCC treatment. The direct participation of hepatologists in HCC treatment would be innovational if they are trained feasibly in performing thermal ablation for hepatomas, alike in Asia. GI/Hepatology fellows in North America are trained to perform ultrasound-guided liver biopsies. The technical skills are similar between liver biopsy and thermal ablation in terms of localization by ultrasound and handling of the needle. The most important part of training for ablation is the precise localization of the needle tip under image guidance [10]. We would like to propose training of GI/hepatology fellows in collaboration with interventional radiology, after certain numbers of liver biopsies are performed under ultrasound guidance. Further discussions would be warranted to determine the actual numbers of ablative procedures required by a trainee to be an independent practitioner. After establishing this training pathway, our observation should support that it benefits patient with HCC in a variety of ways.
We would also like to emphasize the role of transplant oncology in HCC prevention. Outreach in the community including primary and secondary care institutions to improve hepatoma screening strategy in certain risk population is an urgent task [11], and we believe this approach should be mainly driven by hepatologists practicing in the community.
We note one of the most important drawbacks of this study arises from its cross-sectional nature including lack of longitudinal data which limits the establishment of causal relationship and antecedent-consequent bias. Thus, the result did not support directly the technical/administrative superiority of the hepatologist-directed thermal ablation over that by interventional radiologists.
Overall, hepatologist-directed thermal ablative therapy for HCC could be an innovative strategy potentially to improve patient access to loco-regional therapy and treatment rates, as well as to improve liver transplant referral pathway and maintenance on waitlist. Hepatologists can play a key role in the management of HCC in the current era of multidisciplinary team approach. Training GI/hepatology fellow in performing ultrasound guided thermal ablation techniques would be one step forward in this direction.AbbreviationsHCC hepatocellular carcinoma locoregional therapy modified response evaluation criteria in solid tumor multidisciplinary team conference The Model for End-Stage Liver Disease Barcelona clinic liver cancer University of California San Francisco
TT: Study concept and design; interpretation of data; statistical analysis; drafting of the manuscript. DA: Acquisition of data; drafting of the manuscript. SS, SL and MK: Critical revision of the manuscript for important intellectual content.
Conflict of interestNone of the authors have any potential conflicts (financial, professional, or personal) relevant to the manuscript.