Jaundice is one of the most common medical condition affecting infants, children, and adults. Jaundice is not a disease but it is a visible sign and symptom of liver disease which occurs when there is an increase in the amount of bilirubin circulating in the blood due to the abnormal metabolism and excretion in the urine. Medicinal plants are being used long ago by our ancestors for the treatment of jaundice. At the present era, consumption of these herbal medicines is increasing at a high speed, due to its less or no side effect and cost-effectiveness as compared to synthetic medicines.
This review describes approximately 55 medicinal plants which are used by rural and tribal people of different area of Chhattisgarh for curing jaundice.
The data was collected from different kinds of literature survey from the year 1993 to 2018. This review has been conferred in a systematic way which includes plant's vernacular name, botanical name along with its family, part used and ethnomedicinal uses in a tabulated form and also the description of scientific evidence behind the folklore uses of some medicinal plants along with their mechanism of action which have been reported in different kinds of literature.
The current study may be useful for the development of new medicines for the treatment of jaundice.
The liver is one of the most important organs of our body. The main function of the liver is to metabolize and detoxify food, drug, and chemicals in the liver [1]. Liver damage or dysfunction is mainly caused by toxic substances such as carbon tetrachloride, chemotherapeutics drugs, antibiotics, microorganism, and chronic alcohol consumption. These leads to the development of different types of liver diseases/disorder such as hepatitis A, hepatitis B, hepatitis C, jaundice, cirrhosis, liver cancer, hemolytic anaemia, etc.[1,2]. The most common cause of the liver disorder is inflammation which is mainly due to the excessive consumption of alcohol, poor diet, malnutrition or drug induced. Jaundice is one of the most common amongst the different types of liver disorders [3]. It is not a disease but it is a symptom of the liver disease which indicates liver malfunctioning. Jaundice is derived from the French word ‘Jaune’ means ‘yellow’ and it is characterized by yellow pigmentation. It is also known as icterus which means yellowish pigmentation of the skin, mucous membrane, and sclera due to an increase in the level of bilirubin in the blood and this condition is called – hyperbilirubinemia. This may be caused by a number of conditions, including an inflamed liver and obstruction in bile duct [4].
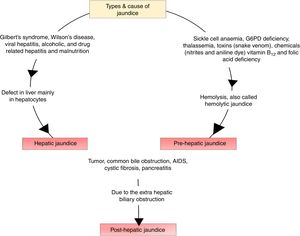
According to the pathophysiology of jaundice and metabolism of bilirubin, there are three types of jaundice which includes
- 1.
Pre-hepatic jaundice which is caused due to the hemolysis of red blood cell.
- 2.
Hepatic jaundice which is caused due to the abnormal metabolism and excretion of bilirubin by the liver.
- 3.
Hepatic jaundice due to the obstruction in the bile duct.
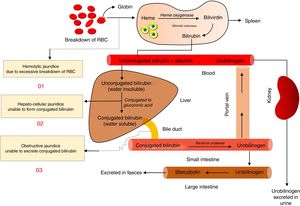
Jaundice is either acquired or congenital [4]. Bilirubin is synthesized within the body by the breakdown of aged red blood cell which causes the release of haemoglobin in the reticuloendothelial cell of liver, spleen and bone-marrow where iron is liberated from haemoglobin along with carbon monoxide and biliverdin which later gets converted by biliverdin reductase to bilirubin which remains in the body as a waste product. The liver usually filters out this bilirubin from the blood and then excreted out of the body through urine and faeces after being metabolized. Jaundice is either caused due to overproduction of bilirubin or inability of the liver to abandon it due to acute liver inflammation, bile duct inflammation, hemolytic anaemia, obstruction of the bile duct, cholestasis, and Gilbert's syndrome. Symptoms of jaundice include a yellow tinge in the skin and in the whites of the eyes, normally starting from the head and spreading down the body, pruritus, fatigue, abdominal pain, weight loss, vomiting, fever, stool paler than usual, and dark urine. The types and causes of jaundice are shown in Fig. 1.
It can also cause psychosis, lethargy, seizures, coma or even death [4,5]. Jaundice is most common in neonates than an adult but when occur in adult, it causes serious plight [6]. Liver disease is one of the major causes of morbidity and mortality all over the world. According to W.H.O. data published in 2017, the total deaths caused due to the liver disease in India reached 2.95%. Liver disease may affect one in every five Indians [7]. The pathophysiology of jaundice is given in Fig. 2.
Chhattisgarh is enriched with natural flora and fauna. Most of the human folk in this region restricts themselves with traditional therapy without any side effects. It became eye-catching to see such exploration of flora, which provides significant therapeutic efficacy against dreadful diseases with lesser costs [8]. In the present day scenario, the region of Chhattisgarh is reported to be of high morbidity and mortality rate of human population due to hepatic disorder within all age groups, wherein the allopathic system became incompatible, and failed to come to the rescue of the patients. The survey found that 2% of the population in Chhattisgarh suffers from Asthma, 11% from malaria, 1% from Jaundice. The prevalence of tuberculosis, jaundice, and malaria is much higher in rural areas than urban areas [9]. Polluted and dirty water is the prime reason for the spread of jaundice, which was confirmed by the recent test done on the water being supplied to the households. The allopathic systems of medicines which are so far formulated and underuse are not completely safe on the ground and free from toxicity. General management of jaundice includes high water intake, proper nutrition, and low-fat diet [10]. Steroids and immunosuppressant are used for the treatment of prehepatic jaundice which can cause an adverse effect on a long-term basis. Further, they are very much costly for routine use. Herbal medicines are often retained popularity due to historical and cultural reasons [11]. In this context, we are focusing on the gathering of information by the literature survey regarding plants which has been traditionally used along with its scientific proof done by the researchers on plants from the folklore of Chhattisgarh. No systematic review on ethnopharmacological studies has been conducted to explore the traditional remedies of Chhattisgarh for treatment of jaundice. There is also no scientific evidence-based review on the traditional medicinal plants used for the treatment of Jaundice in Chhattisgarh. So in this concern, we reviewed different medicinal plant from the different kinds of literature which has been used traditionally by the people of Chhattisgarh for the treatment of jaundice along with its biochemical mechanism of action with its active phytochemicals that are or may be responsible for treatment for the jaundice. This review article may be important for the development of new pharmaceuticals and also to emphasize on the role of ethnomedicine to cure jaundice.
In Chhattisgarh region various medicinal plants has been used traditionally for the management and treatment of jaundice. List of these medicinal plants, traditionally used orally for the treatment of icterus was gathered from the different literature and electronic database such as PubMed, Scopus, and Google Scholar. The data for the traditionally used medicinal plant for the treatment of jaundice was retrieved from different articles along with its scientific evidence for its efficacy and molecular mechanism of action. Data related to the traditionally used medicinal plant was collected from the year 1993 to 2018. Table 1 demonstrates the selected traditional medicinal plants used for the treatment of jaundice by the tribal people of Chhattisgarh which consists of botanical names of plants along with its vernacular name, parts used of the plant, ethnomedicinal use other than jaundice. Table 2 shows the scientific evidence for the traditional claim of these medicinal plants, which includes biological names of the plants, parts, and type of extract of that plant part used for the study, animal model used for the in vivo studies, and method and route of administration of extract. Results of these studies were also summarized by comparing the difference between test and control group on the basis of a different biochemical parameter such as SGOT, SGPT, ALP, SOD, CAT, GSH, TG level, and serum bilirubin level.
List of traditional medicinal plant used for treatment of jaundice.
| S. no. | Botanical name | Family | Vernacular name | Part use | Ethnomedical use | Ref. |
|---|---|---|---|---|---|---|
| 01 | Abrus precatorius L. | Fabaceae | Gunja | Leaves, root, seed | Jaundice, gonorrhoea, fever, cough, cold paralysis, abdominal pain, tumour | [12] |
| 02 | Acacia nicotica (L.) Wild | Fabaceae | Babool | Whole plant/flower | Jaundice, scurvy, pneumonia, diarrhoea, toothache, cough, facial paralysis, ease delivery, asthma, fever | [13] |
| 03 | Achras sapota L. | Apocynaceae | Pilaghanti | Leaf, flower | Jaundice, liver tumour, malaria, anticancer | [14] |
| 04 | Aegle marmelos (L.) Correa | Rutaceae | Bael, Khotta | Leaf, stem, bark, fruit, flower | Jaundice, stomach tonic, piles, cardiotonic, urinary problem, toothache, diabetes, diarrhoea, dysentery, piles | [15,16] |
| 05 | Aloe barbadensis Linn. | Liliaceae | Ghikwire | Leaf | Jaundice, headache | [15] |
| 06 | Andrographis paniculata Ness (Burm. f.) Wall. | Acanthaceae | Kalmegh, Bhuineem | Whole plant, seed | Jaundice, blood purifier, skin disease, malaria, diabetes, joint pain, fever, anti-snake venom, stomachic, cough, liver tonic, antifungal, leaves in diabetes and blood purifier | [13,16,17] |
| 07 | Argemone maxicana L. | Papaveraceae | Pili kateri | Latex, oil, root, bark, leaf seed | Latex in Jaundice, skin disease, wound healing seed oil anthelmintic, purgative used in skin disease | [13,18] |
| 08 | Baliospermum montanum (Wild) Muell. Arg. | Euphorbiaceae | Wild castor, Dandi Dantimool | Root | Jaundice, piles, anaemia, conjunctivitis, skin disease, snake bite, blood purifier | [12] |
| 09 | Bryophyllum pinnatum (Lam.) Oken | Crassulaceae | Patharchata | Leaf | Jaundice, diabetes, diarrhoea, headache, asthma, in a wound, kidney stone, skin disease | [13,14] |
| 10 | Boerhaavia diffusa Linn. | Nyctaginaceae | Punarnava | Whole plant | Viral jaundice, fever, constipation, leucorrhoea, lumbar pain, myalgia, skin diseases, cardiac disorders, urinary infection, vesical stone, anaemia, dyspepsia, constipation, and general debility | [19] |
| 11 | Cajanus cajan Linn. | Fabaceae | Arhar | Leaf, seed | Jaundice, stomach disorder | [20] |
| 12 | Carica papaya Linn. | Caricaceae | Papita | Fruit, root, bark | Jaundice, abortion, inflammation, sickle cell anaemia, inflammation | [21] |
| 13 | Cassia angustifolia (Vahl) | Fabaceae | Charota bhaji, Markandik | Whole plant | Jaundice, rheumatoid arthritis, blood disease, diarrhoea, scabies, eczema, ringworm, leucoderma, skin disease | [12] |
| 14 | Chrozophora plicata (Vahl) | Euphorbiaceae | Sahadevi | Aerial part | Jaundice, tantircuse | [22] |
| 15 | Chrozophora tintoria L. | Euphorbiaceae | Kukronda | Aerial part | Jaundice | [22] |
| 16 | Clitoria ternateu | Fabaceae | Aparajita | Seed | Jaundice and liver swelling, juice applied in nose for a migraine, excessive bleeding, child abdomen pain | [23] |
| 17 | Coccinia grandis (L.)J. otto Voigt | Cucurbitaceae | Kunuru | Leaf | Jaundice leaves paste in high fever, diabetes, tuberculosis and skin disease | [18] |
| 18 | Coleus aromatic | Lamiaceae | Pashan bhed, patar Bhed | Root | Jaundice | [22] |
| 19 | Curculigo orchioides | Liliaceae | Kali musli | Root | Jaundice, asthma, aphrodisiac, alternative, appetizer, piles, blood-related disorders, etc. carminative, tonic, antipyretic and ophthalmic, indigestion, vomiting, diarrhoea, joint pains, etc. | [19] |
| 20 | Curcuma angustifolia L. | Zingiberaceae | Tikhur | Rhizome | Jaundice, asthma, fever, leprosy, leucoderma, anaemia, burning sensation, kidney stone | [21] |
| 21 | Eclipta alba (L.) Hassk | Asteraceae | Bhringaraj | Whole plant | Jaundice, juice used in hair problem, typhoid, dysentery | [23] |
| 22 | Eclipta prostrata Roxb. | Euphorbiaceae/Asteraceae | Ghamira, Bhringraj | Whole plant, leaf | Jaundice, liver disorder, enlargement of liver and spleen, headache, night blindness, asthma, cold, cough, malaria, fever, hair tonic | [12,17] |
| 23 | Emblica officinalis Gaertn. Linn. | Euphorbiaceae | Amla | Fruit, leaf, bark | Jaundice, constipation, stomatitis, disorders of vision, fever, cough, wheezing, cardiac disorders, arthritis, skin problem, hair fall, tuberculosis, wound healing and rheumatism | [16,18,19] |
| 24 | Eriocaulon sp. Linn. | Eriocaulaceae | Choota, Chootatrina | Whole plant | Jaundice, inflammation, fever, pretties, and urinary system diseases, laxative, diuretic, carminative, digestive, stomachic | [19] |
| 25 | Ficus hispida Linn. | Moraceae | Gobla | Leaves, fruits, bark | Jaundice, leucoderma, psoriasis, haemorrhoids, ulcers, inflammations, fever | [19] |
| 26 | Ficus religiosa Linn. | Moraceae | Peepal | Whole plant, latex | Jaundice, eczema, toothache, leucorrhea, cut and wounds, earache, stomach pain cough and cold | [13] |
| 27 | Hedyotiscorymbosa (Linn.) | Rubiaceae | DavanaPatta | Whole plant | Jaundice, fever, depression, giddiness, flatulence, colic, constipation, skin diseases, cough, bronchitis, and hepatitis | [19] |
| 28 | Hemidesmus indicus (L.) R.Br. | Asclepiadaceae | Anantmool | Root, bark, leaves | Root in jaundice and abdominal pain, leaves in eye infection, teeth ache | [23] |
| 29 | Hygrophilla auriculata (K. Schum.) | Acanthaceae | TalmakhanaKamtakalya | Roots, leaves, seeds | Jaundice, liver disorder, ascites, hyperpiesia, rheumatoid arthritis, vesicle calculi, sexual weakness, impotency, dropsy, cough, and anaemia | [17,19] |
| 30 | Lawsonia inernis Linn | Lythraceae | Mehnadi | Seed, leaves, root | Jaundice, nervine disorder, headache, anti-inflammatory, skin disease, emmenagogue, antifungal, hair fall, burn | [12,13] |
| 31 | Leucas cephalotus L. | Lamiaceae | Gubha | Juice | Jaundice, headache, snake bite, wound, carminative, laxative and anti-parasitic | [12] |
| 32 | Luffa acutangula (L.) W. Roxburg | Cucurbitaceae | Torae | Fruit, tendrils, seed | Jaundice, tendrils used as an antidote, juice used in snake bite and seed constipation | [18] |
| 33 | Madhuca longifolia Mach | Sapotaceae | Mahua | Jaundice, piles, relieve the pain of a hernia, snake bite | [21] | |
| 34 | Mallotus phillippensis Muell Arg. | Euphorbiaceae | Rohini | Fruit | Jaundice, destroy threadworm, hookworm, roundworm, colic pain, bronchitis, purgative, carminative | [12] |
| 35 | Mentha arvensis L. | Lamiaceae | Pudina | Whole plant | Jaundice, abdominal pain, antiemetic | [14] |
| 36 | Mimosa pudica Linn. | Fabaceae | Lajwanti | Leaves, root | Jaundice, oedema, allergy, bronchial asthma, haemorrhoids, menorrhagia, ulcer, arthritis and fever, diabetes, piles, diarrhoea, excessive urination, indigestion | [13,19] |
| 37 | Momordica charantia L. | Cucurbitaceae | Karela | Fresh fruit, leaves | Jaundice, diabetes, piles, vermifuge, carminative, laxative, cough, paralysis, eye problem | [12] |
| 38 | Peristrophic bicalyculata (Retz) Nees | Acanthaceae | Kak jangha | Whole plant | Jaundice | [22] |
| 39 | Phyllanthus amarus Linn. | Euphorbiaceae | Bhui korma | Leaf, root | Jaundice, diabetes, root in fever and decoction of the whole plant in malarial fever and skin disease | [18,19] |
| 40 | Phyllanthus fraternus Webstar. | Euphorbiaceae | Bhuiamla | Fresh leaves | Jaundice, fever, inflammation, asthma, cough, diabetes, ulcer | [12] |
| 41 | Phyllanthus niruri L. | Euphorbiaceae | Bhuiamla | Whole plant | Jaundice, fever, urinary disease, dysentery, genitourinary affection, sores, menstrual problem | [12,14,16] |
| 42 | Phyllanthus urinaria L. | Euphorbiaceae | Bhuiamla | Whole plant | Jaundice, liver disorder, demulcent, eczema | [12] |
| 43 | Portulaca oleracea | Portulacaceae | Badinoni | Whole plant | Jaundice, tumour, inflammations, diabetes, burns, headache, burning sensation, vomiting, dysentery, skin diseases, and stomatitis | [19] |
| 44 | Punica gratum L. | Punicaceae | Aanar | Fruit, leaf, whole plant | Jaundice, heart problem, eye and ear disorder, tonic, migraine, vomiting, piles | [13] |
| 45 | Raphanus sativus L. | Brassicaceae | Muli, Mura | Leaf and root juice | In jaundice and gall bladder stone, diarrhoea, pemphigus | [14,18,21] |
| 46 | Saccharum officinarum L. | Gramineae | Ikha/Ganaa | Leaves | Jaundice, cooling, laxative, diuretic, urinary disease | [12] |
| 47 | Solanum nigrum Linn. | Solanaceae | Makoi | Jaundice, constipation, piles | [21] | |
| 48 | Sphaeranthus indicus Linn. | Asteraceae | Molal Phaji, Mundi | Fruit, whole plant | Jaundice epilepsy, migraine, fever, cough, haemorrhoids, helminthiasis, skin diseases and as a nervine tonic, earache with black pepper, toothache, piles, vomiting, and uterus pain | [18,19,21] |
| 49 | Tacca aspera | Dioscoreaceae | Barahi kand | Embarked stem | Jaundice, tonic, fever, blood purifier | [22] |
| 50 | Tamarindus indica Linn. | Fabaceae | Imali | Leaf, flower, root, bark, fruit, seed | Jaundice, asthma, amenorrhea, scabies, ulcer, wound | [24] |
| 51 | Tephrosia purpurea (Linn.) Pers | Fabaceae | SarphonkMeghapati | Seed, whole plant | Jaundice, poison, seed oil externally in skin diseases, purities, splenomegaly, ulcer, dysentery, wound, fracture, filariasis, dysmenorrheal, anaemia, fever, boils, pimple, and haemorrhoids | [19,21] |
| 52 | Thespesia lampus Lav | Malvaceae | Amagong | Leaf, fruit juice, root, bark, seed | Jaundice, gonorrhoea, syphilis, hyperacidity, cough, dysentery, fever, sunstroke, worms, health tonic | [12] |
| 53 | Tinospora cardifolia (Wild.) Miers | Menispermiaceaea | Giloy | Whole plant, stem root, leaf, leaf | Jaundice, diabetes, rheumatoid arthritis, piles, eye problem, dengue, leprosy, fever, cardiac debility, skin disease, cough, urinary system disease | [13,19,21] |
| 54 | Triticum aestivum L. | Poaceae | Ganha | Leaves, seed | Jaundice, constipation, ulcerative colitis | [20] |
| 55 | Woodfordia fruticosa (Linn.) Kurz | Lythraceae | Dhavi | Flower | Jaundice, haemorrhage, anaemia, leucorrhea, menorrhagia, diarrhoea, dysentery, ulcer, diabetes, oligospermia, urinary tract infection | [19] |
In vivo studies on medicinal plant traditionally used for the treatment of jaundice.
| S. no. | Plant | Part used/extract | Method/route of administration of extract | Animal model | Results | Active constituent that may be/are responsible | Ref |
|---|---|---|---|---|---|---|---|
| 1 | Abrus precatorius Linn. | Seed/hydro-ethanolic | Paracetamol-induced liver damage/orally | Wistar rate male | Significant reduction in paracetamol induced increased serum enzyme level (ALT, AST, ALP, bilirubin) | Gallic acid, glycyrrhizi, trigonelline | [25] |
| 2 | Acacia nilotica | Aerial part/methanolic | Acetaminophen-induced hepatic damage/orally | Male Wistar rate | AST, ALT, ALP, liver weight, and total bilirubin level reduced to the normal elevated the total protein and GSH level and decreased the level of LPO | Umbelliferone, gallic acid, niloticane, and kaempferol derivatives | [28] |
| Bark/ethanol extract | N-nitrosodiethylamine and CCl4 induced hepatocellular carcinoma | Swiss albino rats | Reduction in liver injury and restored liver cancer markers level (ALT, AST, ALP, GT, TBL, AFP, and CEA) and prevent hepatic MDA formation and GSH, increase in activities of CAT, SOD, GPx and GST | Gallic, protocatechuic, caffeic, ellagic acids, quercetin | [29] | ||
| 3 | Aegle marmelos | Pulp/seed aqueous extract | CCl4 induced hepatotoxicity/orally | Albino Wistar rat | Reduction in plasma enzyme (ALT, AP, AST) and bilirubin level to normal level by pre- and post-treatment with extract | [67] | |
| Leaves/powder | Ethanol-induced liver toxicity/orally | Male albino Wistar rat | Reduction in the increased level of TBARS and GPx to normal in liver tissue and significant improvement of GSH, SOD, CAT in plasma and liver tissue. Increased catalase activity | [68] | |||
| Powdered fruit pulp | Gentamicin-induced liver injury/oral | Wistar albino rats | Reverse the increase in SGOT, SGPT, ALP, ACP, and bilirubin level) and histological (damage to hepatocytes) induced by gentamicin and also reverse the significant changes in the level of LPO, SOD, glutathione, and catalase in liver homogenate injury | [69] | |||
| 4 | Andrographis paniculata Nees. | Aerial part/ethanol | Paracetamol-induced acute hepatotoxicity/orally | Female Swiss albino mice | SGPT, SGOT, ALP, bilirubin reduced to the normal and improve the level of SOD, catalase, GSH, GPx decrease level of LPO | [70] | |
| Leaves/alcoholic extract/ | Plasmodium berghei K173 induced hepatic damage/orally | Male mastomyl natalensis GRA Gissen strain | Decrease level of lipid peroxidation product, ALP, SGOT, SGPT, recovery of SOD, glycogen, LPO, protein, total cholesterol | Diterpenes (andrographolide and neoandrographolide) | [30] | ||
| Leaves/aqueous extract orally | BHC induced liver damage/orally | Male albino mice | The protective effect due to the increase in the activity of GSH, CAT, SOD, GSH, GPx, GRx, Decrease in the activity of LPO | [31] | |||
| Leaves/isolation with chloroform and methanol | CCl4/tBHP induced hepatic intoxication/intra-peritoneal | Albino mice | Decrease MDA formation, reduced GSH depletion and enzymatic leakage of glutamine, SGPT, and ALP | Diterpenes (Andrographolide I, Andrographolide II, Andrographolide III) | [71] | ||
| Leaves/methanol and chloroform isolation of andrograph-olide and arabinogalactan proteins | Ethanol-induced hepatic renal toxicity/intra-peritoneal | Albino mice | Decreases the level of GOT, GPT, ACP, ALP, and LP to normal | Andrographolide and arabinogalactan proteins | [32] | ||
| 5 | Argemone maxicana L. | Stem/aqueous extract | CCl4 induced hepatotoxicity/oral | Albino Wistar rate | Decrease serum aspartate transaminase, Alanine aminotransferase, alkaline phosphate to normal | [34] | |
| Crude leaf powder | CCl4 induced hepatotoxicity/oral | Albino Wistar rate | Anti-icterus activity by the decrease in AST, ALT, ALP, total and direct bilirubin level to normal | [36] | |||
| 6 | Baliospermum montanum (Willd.) Muell.-Arg | Root/methanolic extract | Paracetamol-induced liver toxicity/orally | Wistar albino rat | Decrease in the elevated serum levels of SGOT, GPT, ALP, TBL, and CHL and increase in the levels of TPTN and ALB | Flavonoids | [72] |
| Roots/alcohol, chloroform, and aqueous extract | Paracetamol-induced liver toxicity/orally | Male albino rats (Wistar strain) | SGPT, SGOT, and ALP restored to the normal level more by alcohol, aqueous extracts than chloroform extract | [37] | |||
| 7 | Cajanus cajan L. | Leaves/methanolic extract | Acetaminophen and d-galactosamine induced hepatic toxicity/oral | Wistar albino rat | Significant reduction in elevated serum enzyme level (SGOT, SGPT, TBL) | Alkaloid and flavonoids | [38] |
| Aerial part/hydroalcoholic extract | CCl4 induced liver damage/oral | Wistar albino rat/orally | Significant reduction in serum enzyme AST and ALT and an increase in total protein | [40] | |||
| Leaves/ethanolic extract | Paracetamol-induced hepatotoxicity/oral | Wistar albino rat | Decreased activity of SGOT, SGPT, ALP, bilirubin (direct and total), total cholesterol, a significant increase in the level of GSH, SOD, CAT, HDL cholesterol | Flavonoids | [39] | ||
| 8 | Cassia angustifolia Vahl | Leaves/90% alcohol | CCL4 induced liver damage/oral | Male Wistar rate | Decrease in bilirubin, AST, ALT, ACP, LDH and increase the total protein level | Flavonoid, terpenoids, tannin, and steroids | [73] |
| 9 | Clitoria ternatea L. | Leaves/ethanolic extract | CCl4 induced liver damage/oral | Male Wistar rate | Decrease AST, ALT, ALP, ACP, LDH and increase in total protein, total conjugate, and unconjugated bilirubin | Alkaloid, anthraquinone, catechin, flavonoid, phenol, saponin, steroid, tannin, terpenoids | [42] |
| Methanol extract/flower | Acetaminophen-induced liver toxicity/oral | Wistar albino mice | Liver marker enzyme, lower the level of AST, ALT and bilirubin levels and level of glutathione restored | Phenolic and flavonoids compound (kaempferol, quercetin, myricetin) | [43] | ||
| Leaf/methanol extract | Paracetamol-induced hepatotoxicity/oral | Wistar albino mice | A significant decrease in AST, ALT and bilirubin level | [41] | |||
| 10 | Chrozophora plicata Vahl | Leaves/methanolic extract | CCL4, paracetamol, thioacetamide | Wistar albino rat | Decrease SGOT, SGPT, ALP, increase total protein, decrease total bilirubin and TG and liver weight | Flavonoid, glycoside, alkaloid, and lignan | [44] |
| 11 | Coccinea grandias Linn. | Leaves/ethanolic and aqueous extract | CCL4 induced hepatotoxicity/oral administration | Wistar albino rate | Significant lowering of serum level of SGOT, SGPT, ALP, total bilirubin, total cholesterol, increase in the level of total protein and albumin | Flavonoid compound | [45] |
| Fruits/methanolic | CCL4 induced hepatotoxicity/oral administration | Wistar albino rate | Decrease in the leakage of marker enzyme into the circulation, AST, ALT, ALP, SB, serum cholesterol, total protein | [46] | |||
| Leaves/ethanolic extract | Paracetamol and CCL4 induced hepatotoxicity/oral | Wistar albino rate | Reduced serum activities, the level of SGOT, SGPT, ALP, and bilirubin level | Alkaloids, triterpenoid or reducing sugar or their combination | [74] | ||
| Leaves/pet ether, chloroform, ethyl acetate fraction of hydro methanol extract | Paracetamol-induced hepatotoxicity/orally | Swiss albino mice | SGOT, SGPT, ALP and Acid phosphate, alkaline phosphate, uric acid and bilirubin reduction in serum Increase total protein and inhibition of lipid peroxidation | [75] | |||
| Root extract/ethanolic extract | Paracetamol, induced liver toxicity/orally | Rat | The decrease in SGOT, SGPT, ALP, total bilirubin, direct bilirubin, the significant increase in total protein, SOD, CAT, GSH activity | [47] | |||
| Fruit/ethanolic extract | CCL4 induced hepatotoxicity/orally | Male Wistar strain albino rat | SGOT, SGPT, ALP, total and direct bilirubin become reduced to normal | [48] | |||
| 12 | Coleus aromaticus Benth | Leaf/ethanolic extract | Naphthalene-induced hepatotoxicity/orally | Male rat | An activity of AST, ALT, AP, ALP, LDH reduced significantly activity of CHL, FFA, LCAT, HDL, LDL, BL reduced significantly | Phenolic compound | [76] |
| 13 | Eclipta alba Hask | Leaves/aqueous extract | CCl4 induced hepatotoxicity/orally | Male albino rat | Preventing the increase of ALT, AST, ALP, total serum bilirubin and a decrease in protein level | Flavonoids and Wedelo lactone | [49] |
| Aerial part/ethyl alcohol extract | CCl4 induced hepatotoxicity/orally | Charles foster rat, Swiss albino mice | Significant reduction in CCl4 induced increase in hexobarbitone sleep time, zoxazolamine induced paralysis time, brormosulphalein retention significant reduced, reduction in AST, ALT, bilirubin elevated level | [77] | |||
| Aerial part/ethanol extract | Paracetamol-induced hepatotoxicity | Albino mice | ALT level reduced significantly after treatment with extract in the group which received paracetamol and ethyl acetate | [50] | |||
| Fresh leaves/ethanolic extract | CCl4 induced hepatotoxicity/orally | Rat and mice | Shortening of hexobarbitone sleep time, zoxazolamine induced paralysis time, brormosulphalein retention, decrease in AST, ALT, bilirubin elevated level | Coumarin, wedel lactone, desmethyl wedel lactone, apigenin, luteolin, and 4 hydroxyls benzoic acid and protocatechuic acid | [78] | ||
| 14 | Emblica officinalis Gaertn. | Aqueous fruit extract/silver nanoparticle | CCl4 induced hepatotoxicity/orally | Wistar male albino rat | Elevated enzymatic level AST, ALT, LDH, Bilirubin ALP restored to normal, TPL increase to the normal level | [51] | |
| Fruits/aqueous extract | CCl4 induced hepatotoxicity/orally | Male Wistar rats | The decrease in the level of serum and liver lipid peroxide (LPO), GPT, ALP, reduce the elevated level to normal | Anti-oxidant, Vitamin E, ellagic acid, new hydrolyzable tannin, emblicanin A and B | [52] | ||
| 15 | Ficus carica Linn. | Leaf/methanolic extract | CCl4 induced hepatotoxicity/orally | Male Wistar rats | The decrease in level of AST, ALP, bilirubin to the normal | Steroids/triterpenoids, coumarin | [79] |
| 16 | Hemidesmus indicus R.Br. | Root/methanolic extract | Paracetamol-induced hepatotoxicity/orally | Wistar rat | Altered AST, ALT, ALP total bilirubin, gamma glutamate transpeptidase came to normal level | Flavonoid, coumarin-lignan, and tannin | [80] |
| Root/methanolic extract | CCl4 and paracetamol-induced hepatotoxicity/orally | Wistar rat | SGOT, SGPT, ALP, total and direct bilirubin restored to normal level | [81] | |||
| Hemidesmus var. pubescens R.Br. | Root, methanolic extract | CCl4 and Paracetamol-induced hepatotoxicity/orally | Wistar rat | SGOT, SGPT, ALP, total and direct bilirubin level reduces, total protein, albumin, total cholesterol, HL, TG restored to normal | Glycosides, tannin, coumarin, phenolic compound | [82] | |
| 17 | Lawsonia inermis Linn. | Root/ethanolic and water extract | Paracetamol and antitubercular drug hepatotoxicity/orally | Wistar rat | Level of cytosolic enzyme reversed to normal, increased the level of endogenous antioxidant enzymes (superoxide dismutase, catalase, and glutathione, GOT, GPT, LDH level, ALT, AST, bilirubin, total protein significant reduction) | Lactone, flavonoids, sterol, tannin, terpenes, gallic acid, and polyphenol | [83] |
| Leaves/methanolic | CCl4 induced hepatotoxicity/orally | Albino rat | ALT, AST, bilirubin level significantely reduces, total protein level increased, | [84] | |||
| Leaves/aqueous extract | CCl4 induced hepatotoxicity/orally | Albino rat | Decrease SGOT, SGPT, SALP, SB level to normal | [85] | |||
| Leaf/butanolic extract | 2-Acetylamino fluorene induced hepatic damage/orally | Male albino rat | Decrease SGOT, SGPT, SALP, SB, lipid peroxidation to normal | [86] | |||
| Seed extract/ethanol | Paracetamol-induced liver toxicity/orally | Male albino rat | Decrease SGOT, SGPT, SALP, SB, bilirubin to normal level, increase level of protein | [87] | |||
| 18 | Leucas cephalotus Linn. | Whole plant/methanolic extract | CCL4 induced liver toxicity/orally | Male mice | Decrease SGOT, SGPT, SALP, SB, total bilirubin level to normal | Flavonoid | [88] |
| 19 | Luffa acutangula Roxb. | Fruit/alcoholic and aqueous extract | Paracetamol-induced hepatotoxicity/orally | Wistar albino rat | Significant reduction in ALT, AST, ALP, direct and total bilirubin, cholesterol, TG, level to normal total protein, albumin | Saponin | [89] |
| Fruit extract/hydroalcoholic extract | CCL4 and rifampin induced liver toxicity/orally | Wistar albino rat | Decrease AST, ALT, ALP, and LDH, increase the level of total protein, decrease malondialdehyde, Increase activity glutathione and enzymatic oxidation, CAT and SOD | Saponin, flavonoid | [90] | ||
| Fruit/alcoholic and aqueous extract | CCl4 induced hepatic injury/orally | Wistar albino rat | Significant reduction SGPT, SGOT, ALP direct and total bilirubin, cholesterol, TG level, increase in total protein and albumin, HDL level | [91] | |||
| 20 | Mallotus phillippensis Muell Arg. | Leaves/methanolic extract | Ethanol-induced liver damage/oral | Albino rat | Significant prevention of an increase in SALT, SALP, direct bilirubin, total bilirubin, cholesterol, level | [92] | |
| LEAVES/METHANOLIC EXTRACT | CCl4 induced hepatotoxicity/orally | Rat | Decrease in level of SGOT, SGPT, SALP, direct bilirubin, total bilirubin and MDA to normal level on pretreatment with extract | [93] | |||
| 21 | Mentha arvensis Linn. | Leaves/ethanol, chloroform, aqueous extract | CCl4 induced hepatotoxicity/orally | Albino Wistar rat | Reduction in the elevated level of SGOT, SGPT, SALP, and SB to normal | Flavonoids | [94] |
| Leaves/ethanol extract | CCl4 induced hepatotoxicity/orally | Albino Wistar rat | Reduction in the elevated levels of AST, ALT, ALP, total and direct bilirubinCAT, SOD, GSH significantly increased and MDA level significantly decreased | Flavonoid and phenolic compound | [95] | ||
| 22 | Mimosa pudica | Leaves powder | CCl4 induced hepatotoxicity/orally | Male albino rats | The decrease in total bilirubin, ALP, ACP, LPO, γ-GT, AST and ALT to normal | Flavonoid, glycoside, alkaloid | [96] |
| Root/methanolic extract | CCl4 induced hepatotoxicity/oral | Rat | Prevent the increase in the level of SGPT, SGOT, CHL, Bilirubin, increase Catalase, GSH, MDA content significantly decreases | [55] | |||
| Whole plant/ethanol | CCl4 induced hepatotoxicity/oral | Albino rat | Reduce the parameter to normal value ALP, ACP, LPO in Tissue, TB, glutamyl transferase δ-GT, AST, ALT treat and protect the hepatic cell | Alkaloid, tannin, glycoside, terpenoids, flavonoids, and saponin | [53] | ||
| Leaves/ethanolic | CCl4 induced hepatotoxicity/oral | Albino rat | Prevented elevation of serum SGOT, SGPT, ALP, total bilirubin and direct bilirubin | Flavonal aglycone and glycoside, coumarin, terpenoids, phenol, tannin, alkaloid | [54] | ||
| Leaves extract/methanolic extract | CCl4 induced hepatotoxicity/oral | Male albino rats | Prevent the increase in SGOT, SALP, SGPT, total bilirubin, direct bilirubin, increases antioxidants SOD, CAT, TP | Glycosides, Alkaloid phenolic compound, alkaloid, triterpenoid, flavonoids | [97] | ||
| 23 | Momordica charanta | Fruit/alcoholic extract | Hyperammonemia induced by ammonium chloride/oral | Male albino Wistar rat | Decrease activity of TBARS, HP, ALT, AST, and ALP, GPx, SOD, CAT, reduce the level of ammonia and urea | Phenolic phytochemicals | [98] |
| Leaves/ethanolic extract | Acetaminophen-induced liver damage/oral | Wistar albino rats | Significant reduction ALT, AST, ALP increase in TLP, GSH level decrease in MDA | Alkaloid, tannin, flavonoid, phenol, saponin, Vitamin C | [99] | ||
| Fruit/aqueous extract | Acetaminophen intoxicated rabbit/orally | Rabbit | Hepatocurative effect and hepatoprotective effect due to the decrease in elevated ALT, AST, ALP, and LDH | [100] | |||
| Fruit/aqueous extract | Restraint stress-induced liver injury/intragastrically | Male mice | Reduces the level of AST, ALT, NO, TBARS and increases GSH, GSHPX catalase level | Phenolic and flavonoid compound | [101] | ||
| 24 | Madhuca indica | Leaves/hydroalcoholic and ethanolic extract | Paracetamol-induced hepatoprotective/orally | Wistar rat | Significant reduction in liver toxicity by lowering ALT, SGOT, SGPT, Bilirubin level to normal | Flavonoid | [102,103] |
| Leaves/ethanolic and hydroalcoholic extract | CCl4 induced liver toxicity/orally | Wistar rat | Significant lowering of the increased level of SGOT, SGPT, ALT, bilirubin to normal | [104] | |||
| 25 | Phyllanthus amarus | Aerial part/aqueous extract | Ethanol-induced liver damage/oral | Male Wistar rats | Decrease release of serum AST, ALT, STG, HTG(hepatic TG) α (TNF-α), IL-1β level back to normal | [57] | |
| Seed/methanolic extract | Simvastatin-induced hepatotoxicity/orally | Albino rat | SGPT, SGOT, ALP, total and direct bilirubin, serum cholesterol and serum TG back to near to normal level, Protein level restored, reduce total bilirubin | [56] | |||
| 26 | Phyllanthus niruri | Leaves and fruit/methanolic extract and aqueous extract | CCL4 induced liver toxicity/orally | Rat | Pretreatment prevent the rise in SGOT, SGPT level, and lipid peroxidation | Phyllanthin and hypophyllanthin | [58] |
| Leaves/ethanolic extract | CCL4 induced liver toxicity/orally | Albino | Significant decrease level of serum bilirubin, SGOT, SGPT, SALP to normal level | [59] | |||
| Leaves and stem/aqueous extract | Nimesulide induced oxidative stress/oral and intraperitoneal | Swiss male albino mice | Increase in SOD, CAT, GSH activity and restored level near to the normal, in pretreated group i.p. than orally | [60] | |||
| 27 | Raphanus sativus | Root/methanolic extract | Paracetamol-induced hepatotoxicity/oral | Albino rat | Level of TBARS, SGOT, SGPT were low, glutathione level was significantly higher in treated group | [105] | |
| Leaves/ethanolic extract | Ethanol-induced hepatotoxicity | Albino rat | Significant reduction of AST, ALT, ALP, total bilirubin | [106] | |||
| Enzyme extract | Tacrine and CCl4 induced cytotoxicity | Male SD rats | Significantly reduced the elevated level of AST, ALP, ALT, bilirubin level to normal | [107] | |||
| 28 | Sphaeranthus indicus | Flower head/methanol extract | CCL4 induced liver toxicity/orally | Wistar albino rat | Lower SGPT and SGOT, ALP hexobarbitone induced shortening of sleeping time and extra stimulated bile flow (chlorogenic activity) | [61] | |
| Stem and leaves/methanolic extract | CCL4 induced liver toxicity/orally | Male albino rat | A decrease in the level of AST, ALT, ALP, TSP, SOD, CAT, GST | Flavonoid, phenolic | [63] | ||
| Flower head/aqueous and methanolic extract | Acetaminophen on induced liver toxicity/orally | Male albino rat | SGOT, SGPT, ACP, ALP, bilirubin and total protein, increase the level of SOD, catalase, GPX by reducing malondialdehyde | Flavonal, flavonoids | [62] | ||
| 29 | Tephrosia pupurea | Root/ethyl acetate fraction of ethanol extract | CCl4 induced liver toxicity/orally | Rat | Prevent the increase in ALT, AST, ALP, bilirubin, TG level | Phenol | [108] |
| Root/ethanolic extract | CCl4 induced liver toxicity/orally | Wistar albino rat | Significant reduction in the AST, ALT, ACP, ALP, LDH, 5′ nucleotides | Flavonoid and polyphenol | [109] | ||
| Whole plant aqueous extract | Paracetamol intoxicated rat/orally | Rat | Elevated serum level of ALT, AST, bilirubin (direct and total) level restore significantly to normal | Flavonoid and polyphenol | [110] | ||
| 30 | Thespesia lampus (Cav.) Dalz | Root/methanolic and aqueous extract | CCl4 induced liver toxicity/orally | Male Wistar rat | Significant reduction of the elevated enzymes levels SGOT, SGPT, ALP, serum bilirubin | [111] | |
| Stem/methanolic extract | CCl4 induced liver toxicity/orally | Male Wistar rat | Lower serum SGOT, SGPT, ALP, serum bilirubin, cholesterol, TG level, Increase SOD, CAT, reduced GSH and decrease LPOX | [112] | |||
| 31 | Tinospora cardifolia (Willd.) Miers | Aerial part/aqueous extract | CCl4 induced liver toxicity/oral | Albino Wistar rat | Significant reduction in ALT, ALP and total bilirubin level to normal | [65] | |
| Stem and leaves/aqueous extract | Lead nitrate-induced hepatotoxicity/oral | Swiss albino male mice | Increase the activity of SOD and CAT reduce the oxidative stress and decreases the level of AST, ALT, ALP ACP | [66] | |||
| Root, stem leaf/petroleum ether, ethanol, and aqueous extract | CCl4 induced hepatotoxicity/oral | Wistar albino rat | Significant reduction in ALT, AST, ALT, and TBL level with ethanolic extract than aqueous extract and petroleum ether extract | Flavonoid, alkaloidPhenolic | [64] |
Abbreviation: ALT, alanine transaminase; AST, aspartate transaminase; ALP, alkaline phosphatase; AP, acid phosphatase; LDH, lactate dehydrogenase; CHL, cholesterol; FFA, free fatty acid; CAT, catalase; HDL, high density lipoprotein; LDL, low density lipoprotein; BL, bilirubin; TBAR, thiobarbituric acid reactive tissue; GT, glutamyl transferase; TBL, total bilirubin; GPx, glutathione peroxidase; SOD, superoxide dismutase; AFP, alpha fetoprotein; CEA, carcino embryonic antigen; GSH, reduced glutathione; GST, glutathione-S-transferase; LPO, lipid peroxidase; ALKP, alkaline phosphate; TPTN, total protein; ALB, albumin; HP, hydroperoxides; STG, serum triglyceride; HTG, hepatic triglyceride; TNF, tumour necrosis factor; IL, interleukin; NO, nitric oxide; GSHPx, glutathion peroxidase.
A. precatorius is a native plant of India commonly known as Gunja in Raipur and Ratti in Raigarh and Korea district of Chhattisgarh. The leaves, roots, and seeds of A. precatorius are used traditionally for the treatment of tetanus, scratches, leucoderma, snake bite and fever along with cough, cold, fever, jaundice. It's paste is used in abdominal pains, in tumour and for abortion also [12,13,17]. Treatment of paracetamol-induced hepatotoxicity in rat by the oral administration of hydroalcoholic extract of seeds of A. precatorius causes significant reduction in the enhanced level of serum enzymes alanine aminotransferase (ALT), aspartate aminotransferase (AST), alkaline phosphatase (ALP) and bilirubin. These results were comparable with the results of reference standard silymarin. Probable mechanism that may be responsible for hepato-protection by the hydroalcoholic extract is that the active constituent such as gallic acid, glycyrrhizin and trigonelline present in the extract act as free radical scavenger which obstruct the production of free radicals involved in the metabolism of paracetamol by microsomal enzymes and interrupt their interaction with polyester fatty acids and diminishes the membrane lipid peroxidative processes [25,26].
2.2Acacia nilotica Linn.A. nilotica is commonly known as Babul/Desi-kikar. Traditionally the bark, leaves, aerial part and flower of this plant is used in Raigarh district of Chhattisgarh for the treatment of congestion, diarrhoea, haemorrhoids, dysentery, cancers and/or tumours, fever, tuberculosis, ophthalmia, leprosy and menstrual problems [13,27]. Administration of the methanolic extract of A. nilotica in rat results in the restoration of the increased serum enzyme level of ALT, AST, and ALP due to the acetaminophen-induced liver damage to normal range level. A. nilotica extract also increases GSH (reduced glutathione) level and decrease MDA (malonyl aldehyde) level indicating its hepatoprotective action against acetaminophen-induced liver damage. A.nilotica contains a high amount of flavonoids, alkaloids, phenolics, steroids, terpenoids, saponins, and tannins. Thus this natural constituent may possess a beneficial effect in the treatment of jaundice through free radical scavenging activity [28]. It has also been reported that gallic acid and catechin present in bark and leaves of A.nilotica showed a protective effect against N-nitrosodiethylamine-induced hepatocarcinogenesis [29].
2.3Andrographis paniculata NeesA. paniculata Nees (Acanthaceae) commonly known as Kal-Megh, which is used traditionally for the treatment of liver disease, jaundice, skin disease, malaria, diabetes, fever, anti-snake venom, stomachic, cough, liver tonic, antifungal, leaves in diabetes and as blood purifier dysentery, bowel complications in children, colic pain and general debility [24,13,16,17]. It has been reported that alcoholic extract of A. paniculata and two of its active constituent, andrographolide, and neoandrographolide, when given orally for two weeks to Plasmodium berghei, infected Mastomys natalensis, causes significant reduction in levels of serum lipoprotein-X, ALP, Glutamate oxaloacetate (GOT), Glutamate pyruvate transaminase (GPT) and bilirubin level to the normal level, which were increased due to the infection [30]. A. paniculata treatment showed hepatoprotective action against BHC (hexachlorocyclohexane) by preventing the BHC induced increase in the activities of glutamyl transpeptidase dismutase, catalase, and glutathione S transferase, and lipid peroxidation [31]. It was also reported that A. paniculate possibly causes induction of hepatic drug metabolizing systems for detoxification of hepatotoxins. Ethanolic extract of the whole plant of A. paniculata significantly reduces elevated serum marker enzymes such as GPT, GOT, ALP, and bilirubin, restored the tissue antioxidant levels and decreased the lipid peroxidation levels in the liver. The results indicate the potential of these two plant extracts to offer protection against the acute hepatotoxicity induced by paracetamol [32].
2.4Argemone mexicana Linn.A. mexicana L. regarded as one of the most significant plant species in a traditional system of medicine. This plant is used traditionally for the treatment of several ailments including tumours, warts, skin diseases, inflammations, rheumatism, jaundice, leprosy, microbial infections, and malaria. The yellow juice which exudes from this plant has long been used for dropsy, jaundice, ophthalmia, scabies and cutaneous affections [13,18,33]. When the aqueous extract of A. mexicana stems administered orally to male albino Wistar rats it showed propitious antihepatotoxic activity against carbon tetrachloride-induced hepatotoxicity in rat. A. mexicana stem extract, decreased serum aspartate transaminase, alanine aminotransferase, and alkaline phosphatase level [34]. Methanolic extract of this plant also showed hepatoprotective action against Carbon tetra chloride (CCl4) induced hepatotoxicity in rat [35]. Crude leaves powder of A. mexicana was also evaluated for its folklore claim of anti-icterus activity against CCl4 induced liver injury in rat. This result showed significant anti-icterus activity in intoxicated rat [36].
2.5Baliospermum montanum (Willd.) Muell.B. montanum is commonly known as Danti belonging to the family Euphorbiaceae. This plant is traditionally used as a remedy for managing various conditions such as jaundice, piles, anaemia, conjunctivitis, skin disease, snake bite, as blood purifier [12,24]. The administration of alcohol, chloroform and aqueous extract of root of B. montanum orally to rat showed a significant reduction in the elevated level of a biochemical parameter such as SGPT, SGOT, and ALP which were elevated by paracetamol. This result reveals that alcohol and aqueous extract of this plant possess significant hepatoprotective activity against paracetamol-induced liver necrosis than the chloroform extract when compared with that of silymarin. In the literature, it has been reported that this plant contains a high content of phenols which posse's high antioxidant activity, which may be responsible for its hepatoprotective activity [37].
2.6Cajanus cajan Linn.This plant is locally called as Arhar, belong to the family Papilionaceae. It has been traditionally used for the treatment of many ailments like jaundice mouth disease, sores, toothache, dysentery, heart disease, bronchitis and as an anthelmintic [20]. It has been confirmed by the experimental data that methanolic extracts of leaves of C. cajans exhibit remarkable hepatoprotective activity in the acetaminophen and d-galactosamine induced hepatic injury. This natural remedy accomplishes hepatoprotective activity by significantly lowering the elevated biochemical marker enzymes such as serum glutamate oxaloacetate (SGOT), serum glutamate pyruvate transaminase (SGPT) and serum total bilirubin to normal level in experimental rats [38]. The ethanolic extract of C. cajan is reported to contain large amounts of flavonoids. It may be assumed that the hepatoprotective activity may be due to the presence of flavonoids in this extract [39]. The hepatoprotective activity of hydroalcoholic extract of the aerial part of C. cajan was also studied against carbon tetrachloride (CCl4) induced liver damage in Wistar rats. The hydroalcoholic extract of C. cajan showed the presence of alkaloid and flavonoid which may be responsible for the hepatoprotective efficiency of the plant against CCl4 induced liver damage [40].
2.7Clitoria ternatea L.C. ternatea, a medicinal herb is commonly known as Aparajita belonging to the family Fabaceae. Seeds of this plant are traditionally used by the people of Bilaspur district of Chhattisgarh as a remedy for jaundice and liver swelling. The juice is applied in the nose for a migraine, excessive bleeding, and child abdomen pain. The leaves and roots are used in the treatment body aches, infections, urogenital disorders, anthelmintic and antidote to animal stings [23]. Methanolic extract of C. ternatea leaves possess a significant therapeutic potential to protect the liver against paracetamol-induced toxicity in mice. The active constituent present in the methanolic extract significantly decreases the elevated level of ALT, AST, and bilirubin in the paracetamol-induced hepatic model. The hepatoprotective activity of C. ternatea leaf may be due to its free radical-scavenging and antioxidant activity of some phenolic compounds which are present in the extracts [41]. Ethanolic extract of leaves of C. ternatea showed significant hepatoprotective potential against CCl4 induced hepatotoxicity by a significant decrease in AST, ALT, ALP, bilirubin, thiopentone induced sleeping time and increase in glutathione, catalase and superoxides dismutase level [42]. One of the studies also confirmed the hepatoprotective action of methanolic extract of C. ternatea flower against hepatotoxicant acetoaminophenon [43].
2.8Chrozophora plicata VahlC. plicata has traditionally used by the people of Bailadila reserve forest area of Dantewada [22]. Experimental investigation of hepatoprotective action of methanolic extract of C. plicata leaves against CCl4, paracetamol and thioacetamide intoxicated rats attenuated significantly the serum level of SGOT, SGPT, ALP, total bilirubin, triglyceride levels and increases the total protein levels. The presence of flavonoids, alkaloids, glycosides, and lignans in the methanolic extract of leaves of C. plicata which was confirmed by phytochemical screening, may be responsible for hepato-protection [44].
2.9Coccinia grandis Linn.The hepatoprotective activity of ethanolic and aqueous of Coccinia grandis leaves was revealed by the significant decrease in the activity of enzymes i.e. SGOT, SGPT, ALP, decreases in the level of total bilirubin, cholesterol and increases the level of total protein in CCl4 induced hepatotoxic model in rat. Flavonoid present in the extract may be responsible for its protective effect [45]. The methanolic extract of the fruits of C. grandis Linn. (Curcubitaceae) also showed hepato-protective action when administered orally to the Wistar rat by observing the same biochemical parameters as above in carbon tetrachloride (CCl4) induced hepatotoxic model [46]. Methanolic extract of root and fruit of C. grandis also showed hepatoprotective action against paracetamol-induced hepatic damage in rat [47,4].
2.10Eclipta alba (L.) HasskE. alba (Asteraceae) commonly known as Bhringaraj. Folklore use of this plant is for the treatment of jaundice, hair problem, typhoid, and dysentery. The aqueous extracts of E. alba when administered orally in CCl4 induced liver injured rats. The plant extract significantly prevent the increase of ALT, AST, ALP, and serum bilirubin in the liver intoxicated rat [49]. Hepatoprotective study of aerial part of this plant was also conducted on the paracetamol induced hepatocellular damage in mice and the result showed a significant protective effect on the liver of mice. This data gives scientific evidence to its traditional use for the liver-related disease [50].
2.11Emblica officinalis (Gaertn.) Linn.E. officinalis belongs to the family Euphorbiaceae. Fruit, leaf, and bark of this plant were traditionally used for jaundice, constipation, stomatitis, vision disorders, fever, cough, wheezing, cardiac disorders, arthritis, skin problem, hair fall, tuberculosis, wound healing and rheumatism [16,18–20]. The hepatoprotective activity of aqueous extract of the fruit of E. officinalis and silver nanoparticles synthesized by using E. officinalis fruit extract was studied in CCl4 induced hepatic damage in Wistar male albino rats. CCl4 causes an elevation in the enzymatic levels of AST, ALT, ALP, LDH, and bilirubin which restore to normal level after the treatment with the aqueous fruit extract of E. officinalis and also the total protein level restored to the normal value [51,52].
2.12Mimosa pudica L.Pretreatment of the 50% ethanolic extract of the M. pudica (Fabaceae) leaves to the liver intoxicated rats by carbon tetrachloride and hepatoprotective action was studied by evaluating the biochemical parameters such as SGPT, SGOT, ALP, total bilirubin, albumin, and total protein. The results were compared with the standard drug silymarin. Pretreatment with this plant extract significantly prevented the increase in the levels of serum SGOT, SGPT, ALP and bilirubin (total and direct) level and also prevented decreases in the total plasma protein level in the CCl4 intoxicated rat. By the phytochemical investigation, it was found that the leaves of this plant contain phytoconstituents like alkaloid, flavonoid, tannin, saponin, coumarin, terpenoids and phenols. These phytoconstituents have antioxidant property due to which it provides protection against hepatic degeneration [53,54]. Methanolic extract of root of M. pudica plant also showed significant hepatoprotective action against CCl4 intoxicated rat [55].
2.13Phyllanthus amarus Schum. & Thom.P. amarus is a medicinal plant of the family Euphorbiaceae. Treatment with the methanolic extract of seeds of this plant to the simvastatin-induced hepatotoxic rat showed significant hepatoprotective by bringing back the elevated level of SGPT, SGOT, ALP, total and direct bilirubin, serum cholesterol, and serum triglycerides to near normal levels [56]. Treatment with aqueous extract of aerial part of P. amarus to ethanol-induced liver injured rat brings the elevated serum level AST, ALT, HTG (hepatic triglycerides), tumour necrosis factor (TNF) to the normal. The probable mechanism behind the hepatoprotective action of this plant is due to the antioxidant effect of the phytoconstituent present in it [57].
2.14Phyllanthus niruri Linn.P. niruri commonly known as Bhuiamla is an annual herb with various medical indications. Traditionally it is used for various ailments like jaundice, diabetes, kidney stones, and liver disorders and also for treatment of hepatitis B viral infection. When methanolic and aqueous extract of leaves & fruits of P. niruri administered to the rat, both the extracts showed significant hepatoprotective action against CCl4 induced hepatotoxicity in rats. It shows hepatoprotective activity by inhibition of membrane lipid peroxidation (LPO), scavenging of 1,1-diphenyl-2picrylhydrazyl (DPPH) radical, by lowering the increased level of SGOT and SGPT. Flavonoids and tannins were reported in the chemical study of this plant that may be responsible for its hepatoprotective action due to its antioxidant property [58]. Ethanolic extract of leaves of this herbal plant also causes a significant reduction in the elevated levels of serum bilirubin, SGOT, SGPT and SALP to normal level in the CCl4 liver intoxicated rat [59]. Aqueous extract of this plant also prevents the hepatotoxicity induced in the rat by nimesulide by investigating the same biochemical parameters [60].
2.15Sphaeranthus indicus Linn.The methanolic extract and aqueous of S. indicus flower head showed a significant hepatoprotective effect against CCl4 induced liver damage by decreasing the serum AST, ALT and ALP level to normal. This hepatoprotective activity further confirmed by decreasing the hexobarbitone induced sleeping time which was increased by CCl4[61]. Similar study was done on the aqueous and methanolic extract of the flower head of S. indicus on acetaminophen-induced hepatotoxicity in the rat. The results confirmed the hepatoprotective action by lowering the SGOT, SGPT, Acid Phosphate (ACP), ALP, bilirubin and increasing the level of total protein [62]. The protective effect of stem and leaves of S. indicus on CCl4 hepatotoxic rat due to the increase in the level of antioxidant enzymes this may be due to the presence of flavonoids which contribute for its hepatoprotective action [63].
2.16Tinospora cardifolia (Thunb.) MiersPetroleum ether, ethanol and aqueous extract of T. cardifolia leaf, stem and root showed significant hepatoprotective action against CCl4 induced liver damage in the rat when administered orally by lowering the serum enzyme level of ALT, AST, ALP, and total bilirubin. Phytoconstituents such as flavonoids and alkaloid present in the ethanolic extract that may be responsible for its hepatoprotective action [64,65]. T. cardifolia stem and leaves extract also showed hepatoprotective action against lead-induced hepatotoxicity in mice due to the scavenging of free radicals generated by the lead toxicity [66]. Table 2 gives detail about the in vivo evidence and its possible mechanism for the efficacy of the medicinal plant used by the people of Chhattisgarh for the treatment of jaundice.
3Discussion and conclusionThe innumerable medicinal plant has been used by the tribal people of Chhattisgarh to get relief from jaundice and other liver related disorder. Various investigation and experimental studies have been done on these medicinal plant have been congregated and its effectiveness with it its possible mechanism are presented in this review. Botanical name and vernacular names of the medicinal plant used traditionally by the people of Chhattisgarh for the treatment of icterus are shown in Table 1. The complete detail about the animal studies of these plants to prove its traditional claim summarized in Table 2. In Table 2 medicinal plants with its possible biochemical mechanism of action along with its active phytoconstituents that may be responsible for the management of jaundice is also described. Various hepato-toxins used in the experiments to prepare the animal model. Most commonly used hepatotoxin to prepare the animal model for hepatoprotective studies are carbon tetrachloride and paracetamol. These chemicals are toxic to the liver by the formation of free radicals after metabolism by cytochrome P450. These free radical cause's lipid peroxidation which causes hepatocyte injury. The hepatoprotective property of medicinal plant is mainly due to the inhibitory effect of phytocontituents present in them on the microsomal enzymes to limit the generation of free radicals and also prevent lipid peroxidation by its antioxidant property. These phytoconstituent acts as a free radical scavenger and a stimulatory effect on hepatic regeneration. Pretreatment of the animal model with the medicinal plant extract exert beneficial effect through several cellular and biochemical mechanism including down-regulation of serum marker enzymes such as SGOT, SGPT, and SALP, direct bilirubin, total bilirubin, and MDA. Medicinal plant extract also reversed the changes in functional parameters, antioxidant parameters and its effectiveness is also confirmed by histological observations. In these studies, we have recorded the various plant species which has been used traditionally for the treatment of jaundices along with its reported pharmacological literature. The present study concludes that varieties of medicinal plants have been traditionally used by the people of Chhattisgarh to cure jaundice and other health condition. This review also confers the scientific evidence and molecular mechanism of these traditional medicinal plant used by the tribal people of Chhattisgarh for the treatment of jaundice. This review also gives an idea about the various active phytoconstituents that may be responsible for the therapeutic effect so that these phytochemical agents can be further investigated to validate the traditional claim and also to isolate and identify new bioactive phytochemicals for the potential therapeutic benefit. Based on this review various active phytochemicals present in the mentioned medicinal plants that are efficacious or may be responsible for the therapeutic effect on jaundice are from different chemical categories including flavonoids like flavonols (quercetin, kaempferol), lignin, a phenolic compound, alkaloid, gallic acid, glycyrrhizin, trigonelline, umbelliferone, protocatechuic acid, diterpenes, andrographolide and neoadrographolide, terpenoids, tannin, steroids, catechin, saponin, lignan, myricetin. Triterpenoids, vitamin C, hypophyllanthin, phyllanthin, wedelactone, coumarin, apigenin, luteolin, protocatechuic acid, luteolin, antioxidants (Vitamin E, ellagic acid), emblicanin A and B, lactone. Various in vitro and in vivo animal studies on the traditionally used medicinal plant of Chhattisgarh confirmed the bioefficacy of that plant on the jaundice management. Further research is needed for finding the efficacy and safety of these phytochemicals for the development of novel drugs.AbbreviationsACP acid phosphatase alpha fetoprotein albumin alkaline phosphatase alanine transaminase acid phosphatase aspartate transaminase hexachlorocyclohexane bilirubin catalase carbon tetra chloride carcinoembryonic antigen cholesterol 1,1-diphenyl-2picrylhydrazyl free fatty acid glutathione peroxidase glutathione reductase reduced glutathione reduced glutathione peroxidase glutathione-S-transferase glutamyl transferase high density lipoprotein hydroperoxides hepatic triglyceride interleukin lecithin cholesterol acyl transferase lactate dehydrogenase low density lipoprotein lipid peroxidase malonyl aldehyde nitric oxide lipoprotein reactive oxygen species serum glutamate oxaloacetate transaminase serum glutamate pyruvate transaminase superoxide dismutase serum triglyceride thiobarbituric acid reactive tissue total bilirubin triglyceride tumour necrosis factor total protein total serum protein World Health Organization
No funding or financial support for this review.
Conflict of interestNo conflict of Interest.
Authors are thankful to the Principal, Dr S.S. Nayak, Siddhi Vinayaka Institute of Technology & Sciences, Bilaspur, Chhattisgarh for his encouragement and support.