Chronic hepatitis C can be associated with extrahepatic manifestations; thus, we explored the association of this viral infection with dilated cardiomyopathy in a group of sixty-three patients with a cardiac ejection fraction of less than 40% determined by an echocardiogram in a prospective study. Two of the forty-one patients with non-ischemic cardiomyopathy (4.8%) had serum antibodies to the hepatitis C virus and one of those had hepatitis C virus RNA (2.4%) in serum, consistent with chronic hepatitis C. One of the 22 patients with ischemic cardiomyopathy (4.5%) had serum antibodies to the hepatitis C virus but the hepatitis C virus RNA was not detected in their serum, consistent with prior infection but not chronic hepatitis C. In this study, chronic hepatitis C was not prevalent in the group of patients, although the only patient with chronic hepatitis C had non-is-chemic cardiomyopathy. As a genetic predisposition to develop cardiomyopathy secondary to chronic hepatitis C has been suggested to be relevant in this type of complication, studies that include different racial and ethnic groups are warranted, as treatment of the hepatitis may lead to resolution of the cardiomyopathy.
No conflict of interests exist
Investigator initiated study supported by Roche Pharmaceuticals.IntroductionChronic hepatitis C can be associated with extrahepatic manifestations including cryoglobulinemia, lymphoma, thyroiditis, and membranoproliferative glomerulonephritis.1-5 An association between chronic hepatitis C and cardiomyopathies has also been reported.6-10
Myocarditis is an inflammation of the myocardium that can be caused by several cardiotropic viruses and that can lead to dilated cardiomyopathy and heart failure.11-13 A high prevalence of hepatitis C virus infection has been reported in patients from Japan with hypertrophic cardiomyopathy, dilated cardiomyopathy and myocarditis.6,8-10,14-16 Recently, the case of a patient with cardiomyopathy and chronic hepatitis C in whom the treatment of the viral hepatitis had been associated with disappearance of the hepatitis C virus from serum and the resolution of his symptoms of heart failure was reported.17 According, to explore further this association, we studied the prevalence of chronic hepatitis C in a group of patients with dilated cardiomyopathy from the United States.
MethodsThis was a prospective study of patients with ischemic and non-ischemic cardiomyopathy who were being followed at the cardiology clinic of a tertiary public hospital in Central Brooklyn. Cardiomyopathy was defined as an ejection fraction of less than 40% as evaluated by a transthoracic echocardiogram. All the patients signed an informed consent prior to participating in the study. The study period was from December 2006 to March 2007.
Serum samples were sent to a commercial laboratory for determination of hepatitis C antibody by an enzyme linked immunosorbent assay and for quantitation of hepatitis C viral RNA by the COBAS Taqman real time by PCR methodology.
The study was approved by the Institutional Review Board.
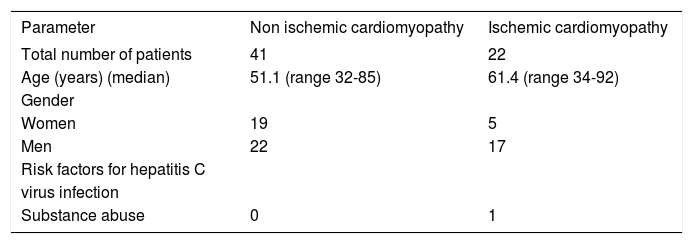
ResultsSixty-three patients were recruited. The study group was comprised of 41 patients with non ischemic and 22 patients with ischemic cardiomyopathy.
The median age was 61.4 years (range 32 to 85) in the patients with ischemic cardiomyopathy, and 51 (range 32 to 85) in the group with non-ischemic cardiomyopathy. There were nineteen women and 23 men in the group of patients with non-ischemic cardiomyopathy, and five women and seventeen men in the group of patients with ischemic cardiomyopathy (Table I).
Characteristics of the patients included in the study.
| Parameter | Non ischemic cardiomyopathy | Ischemic cardiomyopathy |
|---|---|---|
| Total number of patients | 41 | 22 |
| Age (years) (median) | 51.1 (range 32-85) | 61.4 (range 34-92) |
| Gender | ||
| Women | 19 | 5 |
| Men | 22 | 17 |
| Risk factors for hepatitis C | ||
| virus infection | ||
| Substance abuse | 0 | 1 |
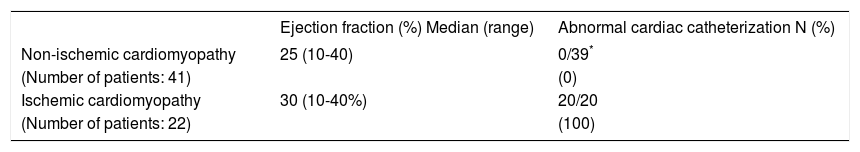
The diagnosis of cardiomyopathy had been made by a transthoracic echocardiogram showing findings of muscular dysfunction consistent with the different patterns of cardiomyopathy. The median ejection fraction in the patients with non-ischemic dilated cardiomyopathy was 25% (range 10 to 40); four patients in this group had features consistent with hypertrophic cardiomyopathy. The median ejection fraction of the group of patients with ischemic cardiomyopathy was 30% (10 to 40). Thirty nine of the 41 patients with non-ischemic cardiomyopathy had had a cardiac catheterization, which had been normal in all. All the patients with ischemic cardiomyopathy had had an abnormal cardiac catheterization revealing vessel disease (Table II).
Ejection fraction and cardiac catheterization results in the study group.
| Ejection fraction (%) Median (range) | Abnormal cardiac catheterization N (%) | |
|---|---|---|
| Non-ischemic cardiomyopathy | 25 (10-40) | 0/39* |
| (Number of patients: 41) | (0) | |
| Ischemic cardiomyopathy | 30 (10-40%) | 20/20 |
| (Number of patients: 22) | (100) |
None of the patients had evidence of acute viral hepatitis based on the hepatic profile available at the time of serum collection. Of the 41 patients with non-ischemic cardiomyopathy, two (4.8%) had serum antibodies to the hepatitis C virus and one of those had hepatitis C RNA (2.4%) in serum, consistent with chronic hepatitis C. In the ischemic cardiomyopathy group, one of the 22 patients (4.5%) had serum antibodies to the hepatitis C virus but the hepatitis C RNA was not detected in their serum, consistent with prior infection and resolution of the hepatitis.
DiscussionIn this study, the prevalence of chronic hepatitis C, defined by positive hepatitis C virus RNA in serum in patients with ischemic cardiomyopathy was 0%, and in patients with non-ischemic cardiomyopathy it was 2.4%. This prevalence is not much higher than the reported for the US population, not suggesting an association between non-ischemic cardiomyopathy and chronic hepatitis C. This finding is in contrast with the reports from Japan, in which a 16% prevalence of chronic hepatitis C in patients with non-ischemic cardiomyopathy was reported.10
The association between chronic hepatitis C in various types of cardiomyopathy was originally reported in Japan, from where most of the literature in this subject has emerged. A study conducted in Italy reported a prevalence of hepatitis C antibodies in patients with cardiomyopathy to be 3.9%,18 which was not significantly different from that of patients without dilated cardiomyopathy. A study from Brazil reported a prevalence of hepatitis C carrier state of 2.9%,19 similar to our results, not suggesting an association between the two conditions. A publication that reported a literature review on the publications that had revealed an association between dilated cardiomyopathy and chronic hepatitis C stated that a significant association between dilated cardiomyopathy and hepatitis C virus had been found in only two papers, both from Japan and by the same author.20 On the surface, the data published so far, including our paper, do not support an association between chronic hepatitis C virus infection and dilated cardiomyopathy; however, the patient we reported17 had such a dramatic response to the treatment of his chronic hepatitis C, which was associated with documented improvement of his ejection fraction and disappearance of symptoms of cardiomyopathy, that the potential for this association cannot be ignored as the option to treat with antiviral therapy exists. An association between hepatitis C and cardiomyopathy was also supported another case report from the United States.21
A limitation of this study is that the only test collected prospectively was the blood sample for antibody and hepatitis C virus RNA determination; all other information was collected retrospectively from the medical records. The review of the data, however, did not suggest that the patients with HCV RNA in serum had acute hepatitis C; thus, it is very likely that the patient who had hepatitis C RNA in serum had chronic hepatitis C.
Dilated and hypertrophic cardiomyopathies in patients with chronic hepatitis C were reported to be more prevalent in subjects who had HLA-DPB1*0901 and HLA-DRB1*1201.22,23 A Non-HLA gene locus spanning from the NFKBIL1 to the MICA gene loci within the MHC class III-class I boundary region was also reported to be characteristic in patients with dilated cardiomyopathy associated with chronic hepatitis C.23 The majority of the patients studied in our study were black, either from the United States or from the Caribbean Islands, consistent with the population of central Brooklyn; accordingly, it is very likely that the HLA make up of these patients was different from that of the patients from Japan in whom a significant prevalence of chronic hepatitis C has been reported.10
Patients with chronic hepatitis C and cardiomyopathy tend to be excluded from the treatment of the hepatitis because the cardiac comorbidities increase their vulnerability to serious consequences from the side effects of the medications (e.g. from the anemia). On the other hand, if the hepatitis C virus infection is the cause of the cardiomyopathy, treating the hepatitis with antiviral medications offers the opportunity to eliminate the virus, and for the recovery of cardiac function in association with the treatment, as exemplified in a previously reported case.17 As treatment of chronic hepatitis C can deter the progression of liver disease, and it may also treat the cardiomyopathy, which is associated with an increased risk of cardiovascular and all mortality,24 it is important to determine if indeed, cardiomyopathy is one of the extrahepatic manifestations of chronic hepatitis C. Thus, studies that explore this association in different ethnic and racial groups properly powered to detect difference in prevalence are warranted.