Background. Bacterial infections are often associated with significant morbidity and mortality in cirrhosis. The common practice of outdoor barefoot walking in the developing world may predispose cirrhotic individuals to skin infection.
Aims. To determine the prevalence, risk factors, spectrum of infective organism and outcome of bacterial skin infection in cirrhosis.
Methods. Consecutive newly diagnosed patients with cirrhosis (n = 200) between September 2007 and September 2008 were studied. Patients with congestive heart failure (n = 50) and chronic kidney disease (n = 50) on follow up at the same institution served as controls. Baseline demographic details, history of outdoor barefoot walking, details of skin infection along with cultures from skin and blood were obtained. The association between patient factors and risk of skin infection was evaluated using logistic regression.
Results. Alcoholism was the predominant etiology for cirrhosis. (50%) Most of them were of Child B cirrhosis. Walking on barefoot was found to be similar in cases and controls. 21(10.5%) patients with cirrhosis had skin infection, three fourth of them had a history of barefoot walking. None of the controls had skin infection. Cellulitis with hemorrhagic bullae, leg ulcers, infected callosity and abscess were observed. The infective organism could be isolated in 17 patients. Escherichia coli was the most frequent organism identified. Logistic regression showed outdoor barefoot walking and serum albumin < 2.5 gm/dL as risk factors for skin infection. Four patients died.
Conclusion. The prevalence of skin infection in cirrhosis was 10.5% with a mortality of 19%. Escherichia coli was the commonly implicated organism. Outdoor barefoot walking was a strong risk factor for skin infection in cirrhosis.
Bacterial infection, irrespective of its etiology is an important concern in patients with cirrhosis since it is associated with increased morbidity and mortality.1 Literature on cirrhotic patients from developed nations indicate urinary tract infection (12-29%) to be the most frequent cause for bacterial sepsis followed by spontaneous bacterial peritonitis(7-23%), respiratory tract infection (6-10%) and bacteremia (4-9%).2 Severe soft tissue infections are common among cirrhotic patients in developed countries3 but are not comparable in magnitude with the above mentioned causes for bacterial sepsis. A significant proportion of Indians from the lower socio economic strata walk barefoot while going out for work. It is also a religious custom to walk barefoot without using foot wear during visits to temples located on hills or mountains in South India. This common practice of outdoor barefoot walking in the developing world may predispose cirrhotic individuals to skin infection. The present study was initiated to determine the prevalence, risk factors, spectrum of infective organism and outcome of bacterial skin infection in cirrhosis.
Materials and MethodsStudy design and settingObservational study of case control type conducted in a tertiary care teaching hospital in South India between September 2007 and September 2008.
Study participantsCases were consecutive patients with cirrhosis (n = 200) who were evaluated for the presence of skin infection at the time of their first enrolment in our liver clinic. Consecutive patients with chronic pedal edema due to congestive heart failure (n = 50) and chronic kidney disease (n = 50) on follow up at the same institution served as controls. Patients with filarial infection of lower extremities, diabetes, history of significant trauma and those on steroids and immunosuppressants were not included.
Method of patient evaluationAll patients were questioned about their age, sex, social habits, and literacy status and per capita income. In addition they were interviewed regarding outdoor barefoot walking and recent pilgrimage on bare foot.
Patients were clinically evaluated for skin infection which when present was assessed for its site, nature and severity. All patients with clinical evidence of infection were admitted for inpatient treatment. Patients were additionally evaluated for etiology of cirrhosis and were staged as per Child-Pugh class. Culture of aspirate from skin and blood were taken in patients with skin infection.
The study was approved by the institutional review board. Written informed consent was taken from all the patients for completion of the questionnaire and collection of blood and tissue samples.
Statistical analysisBaseline characteristics of study patients were expressed in number and percentage for discrete variables while continuous variables were expressed as mean ± standard deviation. Association between patient factors (age, sex, smoking, alcoholism, history of outdoor bare foot walking, serum albumin less than 2.5 g/dL and prolonged prothrombin time beyond 6 sec of control) and skin infection was evaluated using logistic regression. A p value of less than 0.05 was considered statistically significant. All statistical analysis were done using SPSS version 11.
ResultsThe baseline characteristics of cirrhotic patients with and without skin infection is shown in table 1. The study cohort was predominantly male (71%). 50% were alcoholics and 30% were smokers. Most of them were of Child B cirrhosis (63%) followed by Child C (21%) and Child A (17%). Alcoholism was the predominant etiology for cirrhosis (50%). Nearly one-third of our patients (32%) gave a history of recent outdoor barefoot walking. Mean age of controls [Male (n = 74): Female (n = 26)] was 48.6 ± 5.2 yrs. 30% of them were walking on barefoot. Cases and controls were of similar socioeconomic status falling either in lower class or upper lower class as per the conventional definitions for economic status.
Baseline characteristics of study population.
| Variable | With skin infection | Without skin infection |
|---|---|---|
| N = 21 | N = 179 | |
| Age in years (Mean ± SD) | 40.6 ± 11.7 years | 46 ± 7.9 years |
| Sex-no (%): | ||
| Male | 16 (76.2) | 126 (70.4) |
| Female | 5 (23.8) | 53 (29.6) |
| Alcoholism-no (%) | 10 (47.6) | 90 (50.3) |
| Smoking-no (%) | 5 (23.1) | 54 (30.2) |
| Literacy status-no (%) | 7 (33.3) | 62 (34.6) |
| History of outdoor barefoot walking or recent pilgrimage on barefoot-no (%) | 16 (76.9) | 48 (26.8) |
| Etiology of Cirrhosis-no (%): | ||
| Alcohol | 10 (47.6) | 90 (50.3) |
| HBV* | 4 (19.0) | 37 (20.7) |
| HCV** | 3 (14.4) | 12 (6.7) |
| Others | 4 (19.0) | 40 (22.3) |
| Child’s stage-no (%) | ||
| A | - | 34 (19.0) |
| B | 13 (61.90) | 112 (62.6) |
| C | 8 (38.10) | 33 (18.4) |
| Albumin < 2.5 mg/dL-no (%) | 16 (76.2) | 59 (33.0) |
| Prolongation of prothrombin time > 6 secs-no (%) | 11 (52.4) | 41 (22.9) |
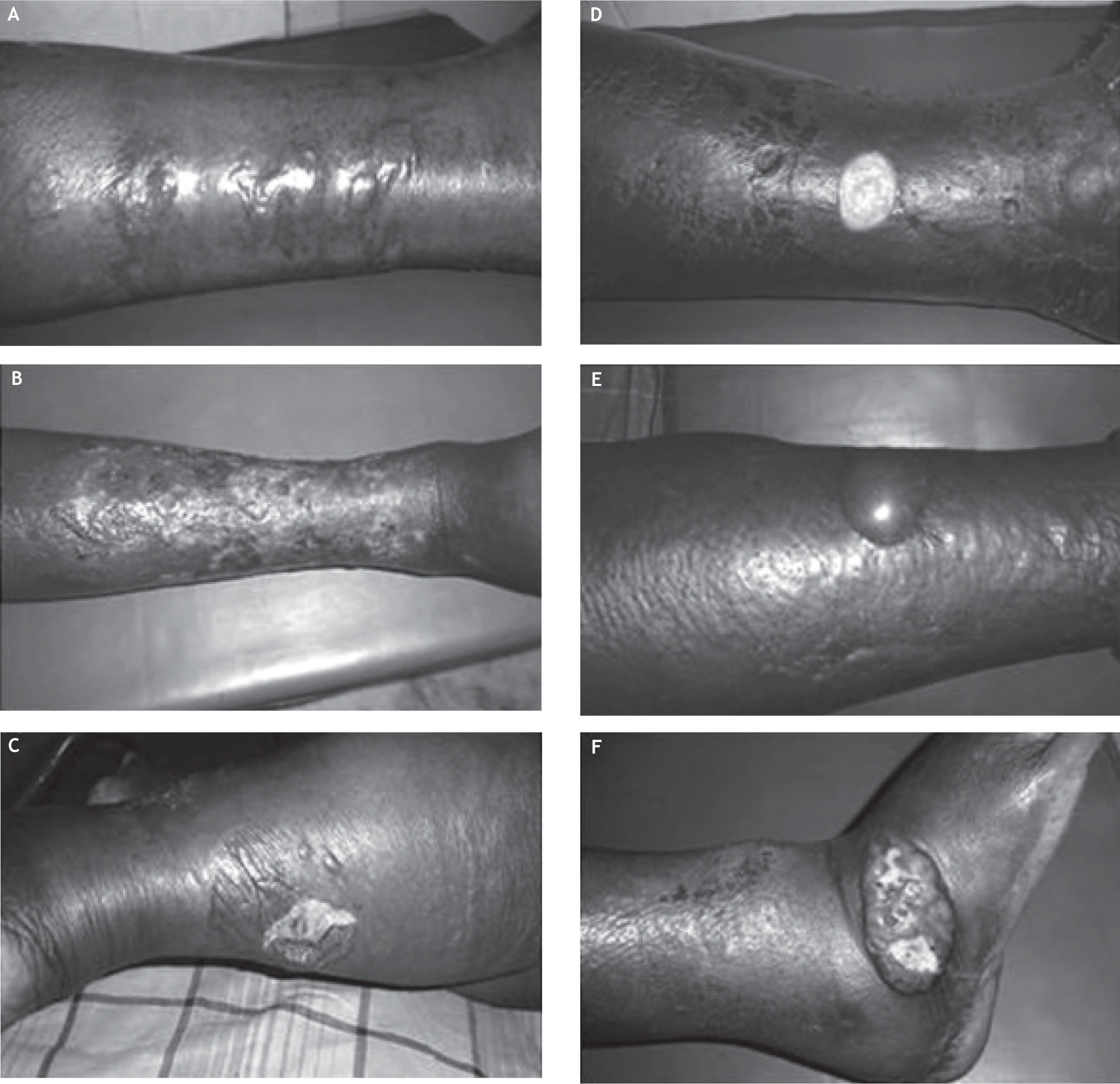
10.5 %(21 of 200) patients with cirrhosis had skin infection. The clinical picture of skin infection widely varied among the study cohort (Figure 1). The nature of skin infection were:
Pattern of skin infection in cirrhosis. A. Multiple hemorrhagic bullae due to Escherichia coli.B. Cellulitis with healing superficial lesions. C. Marked limb edema with ruptured bullae. D. Shallow ulcer with skin hyperpigmentation. E. Cellulitis with a bulla. F. Edema with ulcer in lateral malleolus.
- •
Cellulitis of lower limbs (n = 7).
- •
Hemorrhagic bullae (n = 3).
- •
Leg ulcers (n = 9).
- •
Infected callosity over the lateral malleolus (n = 3).
- •
Recurrent abscess in the arm and the chest wall (n = 1).
The infective organism could be isolated either from skin or blood in 17 patients (81% of patients with clinical sepsis). Escherichia coli was isolated from blood or skin aspirate in 11 patients (both blood and skin aspirate in 3, blood alone in 3 and skin alone in 5). Klebsiella and Staphylococcus aureus were isolated from the skin in four and two patients respectively. The infective pathogen could not be isolated in 4 patients. All patients were initially treated with intravenous cefazolin which was later revised according to in vitro culture sensitivity. Logistic regression identified outdoor barefoot walking (p = 0.001) and serum albumin < 2.5 g/dL (p = 0.002) as risk factors for skin infection. Four patients (19%) with skin infection died. All the patients who died were suffering from Child C cirrhosis and were infected with Escherichia coli. The etiology of cirrhosis was Hepatitis C in two, Hepatitis B in one and alcohol related in one patient. Hemorrhagic bullae (n = 2) and cellulitis with ulcers (n = 2) was observed in patients who succumbed to the infection. None of the controls had skin infection.
DiscussionBacterial infections account for about 25% of deaths in cirrhosis.2 Patients with decompensated cirrhosis are more susceptible to infection compared to compensated cirrhosis.4,5 Despite the widespread use of empirical antibiotics, sepsis in cirrhosis often follows a deteriorating clinical course with an in-hospital mortality of approximately 15%.6
Skin and soft tissue infections occur in 2-11% of patients with liver disease.3 Our observation in a cohort of predominantly male alcoholics suffering from cirrhosis showed a 10.5% prevalence of skin infection.
Escherichia coli was the most frequent pathogen identified from skin aspirate or blood culture in the present study. Bacterial skin infections among non-cirrhotic individuals are frequently caused by gram positive pathogens (mainly group A streptococci and Staph. aureus) and infrequently due gram negative pathogens.7,8 Skin infection due to Escherichia coli has been frequently reported in patients with cirrhosis.9,10 Other Gram negative pathogens associated with cellulitis in cirrhosis include Klebsiella, Pseudomonas, Proteus, Aeromonas and Vibrio species.3,11 Furthermore, they suffer from severe skin infections like cellulitis with hemorrhagic bullae often caused by gram negative bacteria and carry a high case fatality.12 This makes gram-negative pathogens (especially Escherichia coli and Klebsiella) the most probable cause of cellulitis when a clinician encounters a cirrhotic patient with suspected bacterial skin infection.
The reason for Escherichia coli to be the most frequent infective pathogen of the skin in patients with cirrhosis is not clear. However, it is well known that cirrhotic patients have impaired clearance of enteric organisms due to depressed Kuppfer cell function, porta-systemic shunt and bacterial translocation.6,13 This may produce frequent gram negative bacteremia giving an opportunity for distant tissue invasion by these pathogens under favorable conditions. This is further complicated by the defective bactericidal function of immunoglobulins including evidence suggesting deficient bactericidal activity of serum IgM for Escherichia coli.14-18
History of recent outdoor bare foot walking was identified as a strong risk factor for skin infections in our study and these infections were mostly restricted to lower limbs except in one patient. Disruption of mechanical defenses may occur following a trivial injury due to barefoot walking. As already discussed soft tissue infections secondary to trauma in non-cirrhotic individuals are often caused by gram positive pathogens which invade the tissue from the external environment. When cirrhotic patients develop soft tissue infections due to trivial trauma secondary to barefoot walking, the severity of infection is expected to be more due to their immunosuppressed status but the causative organism is supposed to be the same spectrum of gram positive and few gram negative pathogens.
In contrary, the etiology in these patients is unusually different with Escherichia coli and Klebsiella dominating in most reports. This makes us think if the culprit is the endogenous gram negative bacteremia which often happens in them due to the mechanisms already explained. Leg edema and chronic venous insufficiency are known to predispose cellulitis19 and this can often happen in cirrhotic patients due to poorly controlled ascites and functional obstruction to Inferior vena cava. Trivial injury to the foot due to outdoor barefoot walking can render the soft tissues of the leg more vulnerable to bacterial invasion by endogenous gram negative bacteria producing clinical sepsis. This mechanism reminds us the fact that systemic infections in patients with cirrhosis are also frequently gram-negative enteric pathogens.20 While this mechanism can partially explain the selective gram-negative epidemiology in barefoot cirrhotic, it may not be a plausible explanation for cellulitis due to other non-endogenous gram negative pathogens. Pathogenesis of cellulitis in cirrhotic patients probably has multiple mechanisms.
Serum albumin less than 2.5 g/dL was significantly associated with skin infection in our study. A recent study on factors influencing outcomes in soft-tissue infections among cirrhotic patients identified that appearance of band form, elevated creatinine, albumin less than 2.5 g/dL, bilirubin more than 3 mg/dL and prothrombin time prolongation more than 5 sec were associated with death.21 An earlier study identified haemmorrhagic bullae as an ominous sign in patients with cirrhosis.12 Two of our patients with hemorrhagic bullae also succumbed to the infection. Low serum albumin, gastrointestinal bleeding, intensive care unit admission for any cause, alcoholism, advanced Child-pugh stage and therapeutic endoscopy have been shown to be risk factors in association with bacterial infection in cirrhotic patients.22
Mortality in our study was 19% (4 of 21). Liu, et al., in their retrospective analysis had observed a mortality of 22% (26 of 118). It should be noted that 63% of our patients were of Child B cirrhosis. Given the short duration of the study period, newly diagnosed status of the study cohort and small sample size, a selection bias towards a less severe stage of cirrhosis is possible. On account of this, our study may not predict the expected mortality due to skin sepsis in patients who will present with Child C cirrhosis.
ConclusionThe prevalence of bacterial skin infection in a cohort of newly diagnosed cirrhotics is 10.5% with a mortality of 19%. The epidemiology of infective pathogen was dominated by Escherichia coli, raising the possibility of endogenous gram negative bacteremia in the causation of skin sepsis. The finding that outdoor bare foot walking is a strong risk factor for skin sepsis emphasizes the need for educating patients with cirrhosis about the risks of barefoot walking to help prevent significant morbidity and mortality. This assumes greater importance in the developing world as most patients diagnosed with cirrhosis receive conservative medical management due to extremely low rates of liver transplantation.
AcknowledgementWe thank Mr Vengatesan A, Lecturer in Statistics, Clinical Epidemiology Unit, Madras Medical College Hospital, Chennai, for his help.