Hepatic sinusoidal dilatation (HSD) is a pathological entity that is characterized by peliosis hepatis (PH) like lesions, with vascular lesions that consist of multiple cyst-like, blood-filled cavities within the liver. To the best of our knowledge, neither PH nor HSD have been associated with systemic vasculitis. We describe herein two cases of idiopathic HSD associated with Takayasu arteritis (TA), diagnosed at an early stage of vas-culitis. The same endothelial target in HSD and TA, and the favorable outcome of HSD with treatment of TA, suggest a pathogenic link between the two diseases.
Takayasu arteritis (TA) is a chronic, inflammatory vasculitis that affects aorta and its major branches of unknown etiology. TA predominantly affects young women. The clinical presentation is characterized by an acute inflammatory phase with nonspecific and vascular symptoms (vascular injury, absence of pulse, ischemia) followed by a chronic phase (vascular fibrosis, occlusion or aneurysm). Therapy is based on corticosteroids and immunosuppressive drugs. Hepatic sinusoidal dilatation (HSD) is a rare pathological entity that is characterized by peliosis hepatis (PH)-like lesions, with vascular lesions that consist of multiple cyst-like, blood-filled cavities within the liver. We describe herein two cases of HSD associated with TA, which was diagnosed prior to any treatment of vasculitis.
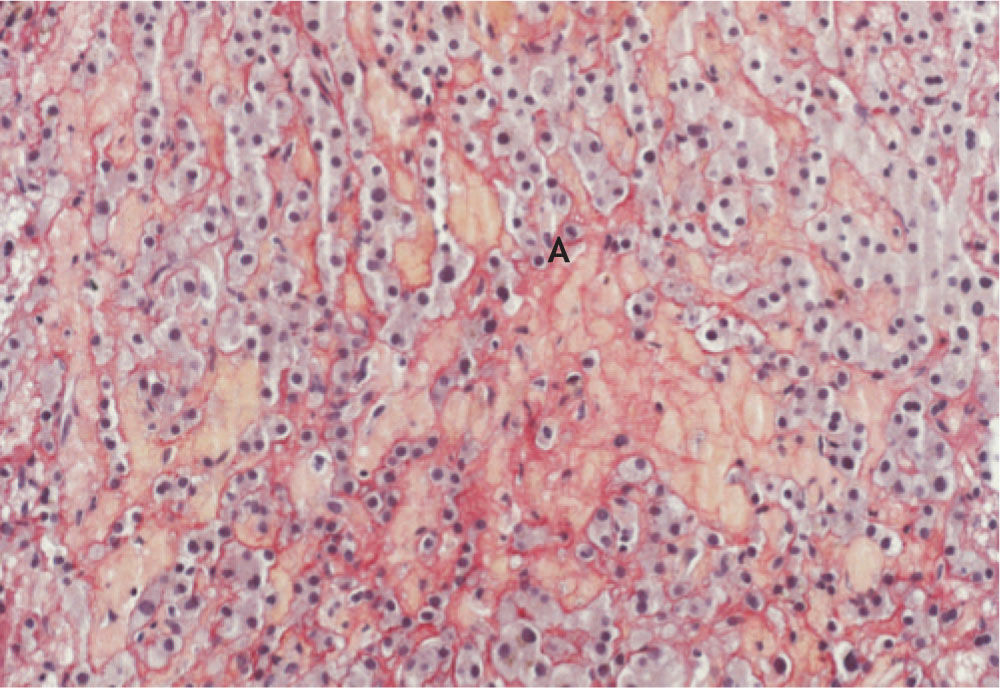
Case ReportCase 1An 18-year-old woman, without significant medical history or medication (including oral contraceptives) was hospitalized for persistent fever and 6 kg weight loss. She complained of precordial and abdominal pain. Physical examination disclosed hepatomegaly. Laboratory analysis revealed 7.8 g/dL haemoglobin (Hb), normal white blood cell (WBC) and platelets count, C-reactive protein (CRP) was elevated at 168 mg/L. She had cholestasis, (γ-GT 1.50 μkat; PA 3.60 μkat) and cytolysis (ASAT 2.4 μkat/L, ALAT: 2.6 μkat/L). Blood and urinary cultures and viral serology were negative, as were antinuclear and anti-neutrophilic cytoplasmic antibodies. Total computed tomography (CT) revealed thoraco-abdominal aortitis with thickening of the aortic wall, and heterogeneous liver enlargement. Vascular Doppler ultrasonography disclosed inflammatory arteritis of the aorta, carotid (Figure 1), mesenteric and renal arteries, in accordance with a diagnosis of TA. Liver biopsy disclosed HSD with round intralobular cavities filled with red blood cells, and hemorrhagic suffusion (Figure 2) without granuloma or neoplastic lesions. She was treated by 3 pulses of IV methylprednisolone (5 mg/ kg) followed by 1 mg/kg/day prednisone. The biological hepatic parameters were normal 2 months later.
A 20-year-old woman was hospitalized for a 6-month fever and inflammatory syndrome. She had no previous medical history. She complained of sweating, asthenia and weight loss. Physical examination was normal. CRP was at 80 mg/L. She had cholestasis, (γ-GT 2.50 μkat; PA 3.20 μkat; ASAT, ALAT: normal). Cultures and viral serology were negative, as were anti-nuclear, mitochondrial, smooth muscle, and LKM antibodies. CT scan showed a voluminous hepatomegaly. Pathological analysis of the liver revealed HSD with enlargement of portal area, and a hepatocytic degeneration. One year later, she complained of carotidodynia. Physical examination disclosed diffuse vascular murmurs. A CT scan showed aortic and carotid inflammatory arteri-tis evocative of TA. She was treated with 3 pulses of IV methylprednisolone (5 mg/kg) followed by 1 mg/ kg/day prednisone. Hepatic parameters were normal 3 months later.
DiscussionLiver manifestations are reported in rheumatic diseases such as systemic lupus erythematosus, primary antiphospholipid syndrome, polymyositis, Sjogren’s syndrome, scleroderma, rheumatoid arthritis and Felty’s syndrome.1 These manifestations include association with chronic active hepatitis, primary biliary cirrhosis, primary sclerosing cho-langitis, and nodular regenerative hyperplasia. Our patients are believed to be the first cases of HSD reported in association with TA. In both cases, there was hepatomegaly and unexplained cholestasis that required liver biopsy, which led to diagnosis of HSD. These young women had no other etiology for HSD. The cholestasis arose during steroid treatment, which suggested a cause-and-effect relationship. Peliosis hepatitis is a rare condition, characterized by the presence of blood-filled cavities of variable size, which often lack an endothelial lining. HSD is characterized by PH-like lesions. The distinction between the HSD and PH is not always sharp. PH and HSD are often accidentally found on biopsies, with no clinical significance but in some cases, hepatic dysfunction is associated. Rarely, hemorrhage or portal hypertension can occur. Imaging features are non-specific.2,3 HSD results of blood flow impairment (veno-occlusive disease, Budd-Chiari syndrome, or right-sided heart failure) or can be associated with sinusoidal infiltration. In 2004, Kakar, et al. reviewed 51 HSD liver biopsies4 and found only 6 patients with inflammatory disease. Chronic wasting diseases or infections (tuberculosis, HIV and B. henselae), advanced neoplasms, renal transplantation and adverse effects of various drugs (steroids, azathioprine, 6-thioguanine, 6-mercaptopurine and oral contraceptives) are the most frequent causes of HSD and PH in adults. Isolated cases of HSD associated with inflammatory disease have been reported.5,6 PH remains unexplained in 20-50% of cases. In inflammatory disease, the pathophysiology of HSD is really unknown.
ConclusionHSD is a rare hepatic manifestation in vasculitis such as TA. It has to be added to the spectrum of hepatic manifestations that occur in autoimmune disease. We propose that the HSD could reflect endo-thelial cell damage observed in TA.
Conflicts of InterestNone.