Hepatic epithelioid hemangioendothelioma (HEH) is an unusual, low-grade malignant vascular tumor of the liver. Here we describe a case of a 40-year-old woman who presented with abdominal pain in the upper right quadrant and giant hepatomegaly, in which imaging studies and a fine-needle liver biopsy confirmed the presence of a large EHE with an isolated lung metastasis. After balancing all possible therapeutic modalities the patient was treated conservatively with thalidomide (300 mg/day). The drug was well tolerated with minimal toxicity and thepatient continues on therapy 109 months after treatment was started with no disease progression. Current therapeutic options for HEH are discussed in light of the clinical case with particular emphasis on anti-angiogenic therapies.
Epithelioid hemangioendotheliomas are rare, low-grade malignant neoplasms of endothelial origin that belong to a group of soft tissue vascular tumors with an intermediate clinical course between benign hemangioma and angiosarcoma. This group of tumors was first described by Weiss and Enzinger in 19821 and has been observed in both soft tissues and solid organs including liver, lungs, bones, spleen and brain. Although the liver is among the commonest viscera where the tumor has been found, primary hepatic epithelioid hemangioendothelioma (HEH) is considered an extremely rare neoplasm with a reported incidence of less than 0.1 per 100,000 population and less than 200 cases reported in the literature. The first series of 32 HEH patients was reported in 1984 by Ishak. et al.2
Presentation, clinical course and prognosis of HEH can vary widely.3 Although some patients with HEH will present with exclusive hepatic disease, the majority have multifocal disease at diagnosis with extensive intrahepatic tumor burden and extra-hepatic metastases.4 Given the low frequency of the disease and its variable natural history, there are no current guidelines for management and therapeutic interventions are generally decided on a case by case analysis. In patients with limited intrahepatic disease, local resection is the treatment of choice, with liver transplantation being an alternative in patients with significant tumor burden.5-7 In metastatic disease, treatment options include chemotherapy, radiotherapy, hormone therapy, thermoablation, percutaneous ethanol injection and follow-up with no therapy.3,8
In this report, we describe a case of a patient with HEH metastatic to the lungs who was treated with oral thalidomide therapy and presented no evidence of disease progression after 109 months of follow-up. In light of this case, we discuss current therapeutic options for HEH with emphasis on using anti-angiogenic therapy which seems to have been successful in arresting the progression of the disease in the current case.
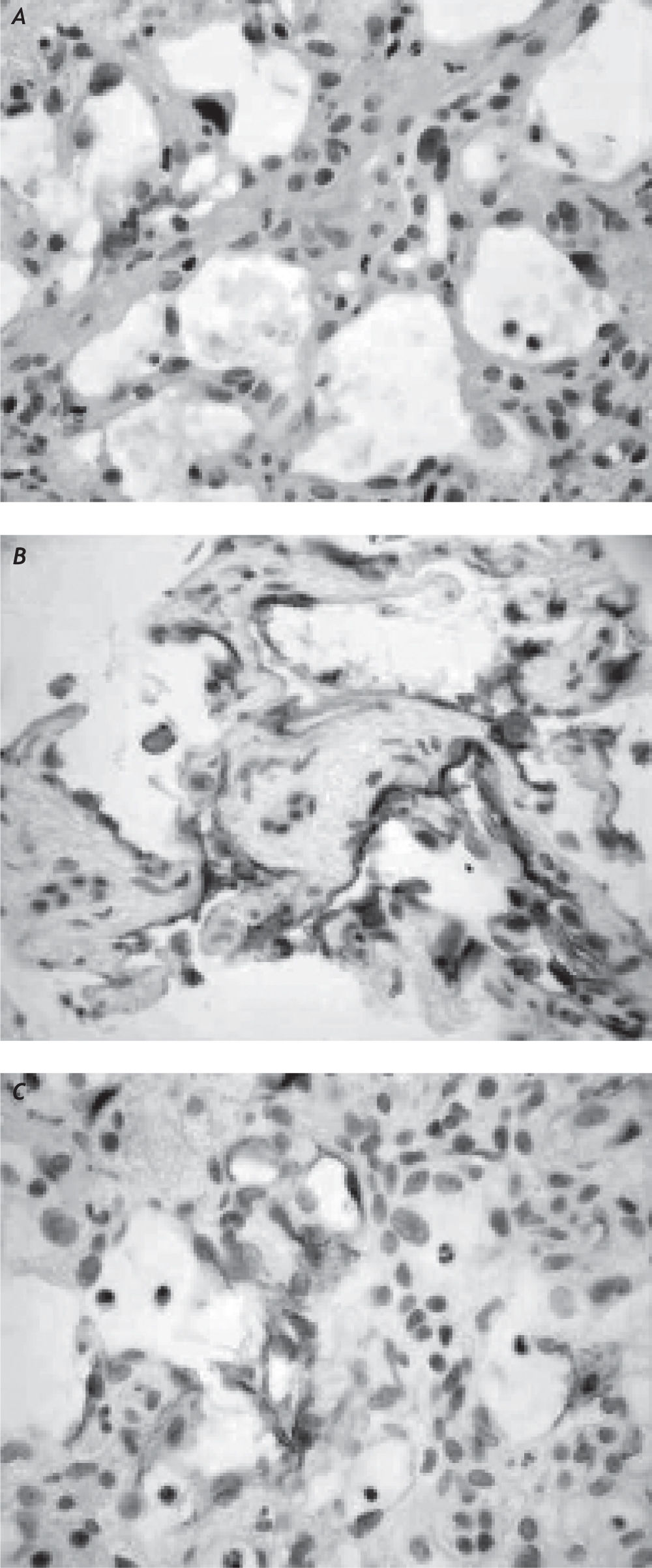
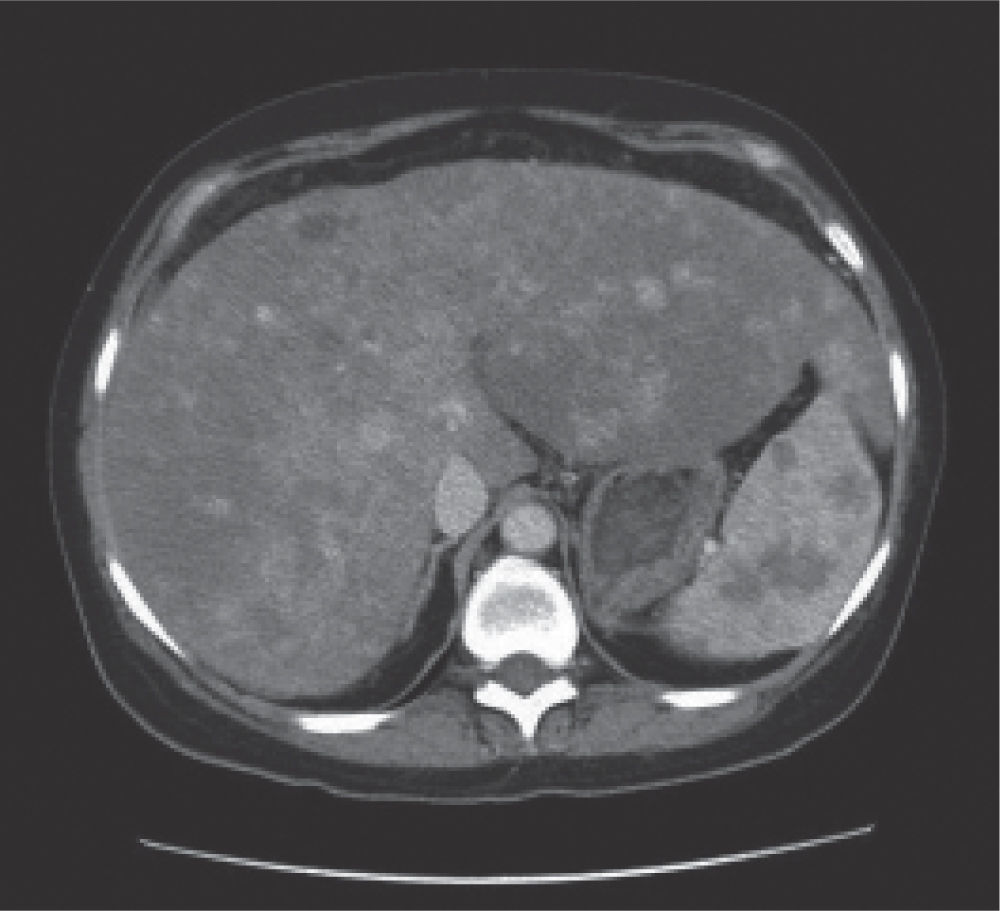
Case ReportA 40-year-old Caucasian woman with HEH was evaluated at the Liver Unit of the Pontificia Universidad Católica de Chile in June 2001. She presented with abdominal pain in the upper right quadrant, asthenia, anorexia and weight loss (15 Kg in six months) and a Karnofsky index of 70 due to limited physical activity that rendered her unable to work with varying amount of assistance needed on daily basis. She had received oral contraceptives for the previous seven years and she had no history of alcohol abuse. The physical examination was remarkable for giant hepatomegaly up to the right pelvis and splenomegaly 8 cm below costal margin. Body weight was 44 kg, she was 1.65 m tall and her body mass index (BMI) was 16.2 kg/m2. Laboratory studies showed slightly increased (less than two-times upper normal limit) alkaline phosphatase and γ-glutamyl-transpeptidase. Other standard hematological and biochemical tests were normal. An abdominal CT scan showed diffuse liver enlargement with a single mass that infiltrated extensively the right lobe of the liver with extension into the left lobe. The patient had a secondary lesion in her left lung as well as splenic metastases. An upper endoscopy was normal. A fine-needle liver biopsy was performed and histopathological examination (Figure 1) showed marked cellular atypia and positive staining for the endothelial markers CD31 and CD34 confirming the vascular nature of the tumor and contributing to the diagnosis of HEH. The single lung nodule suspicious for metastasis was excised using a videothora-coscopic approach and histological examination confirmed the diagnosis of epithelioid hemangioendothelioma. After evaluation in the liver clinic, the patient was considered unsuitable for liver transplantation due to confirmed metastatic HEH and not a candidate for loco-regional therapies due to the large tumor burden. Thus and based on its anti-angiogenic effects, thalidomide-based therapy was offered. The starting dose of thalidomide was 200 mg per day, which was increased up to 300 mg per day after a month. The treatment was well tolerated without significant toxicity and with no evidence of peripheral neuropathy. After 3 months of therapy, she reported relief of abdominal pain and a subjective reduction in hepatosplenomegaly. After six months of receiving thalidomide, the patient was asymptomatic recovering her normal weight of 62 kg with a BMI of 22.8 kg/m2. Physical activity was completely normal with a Karnofsky index of 100 and a successful return to work life. Serial abdominal CT scans performed during the follow-up (at 6, 12, 24, 36, 48 and 91 months). The last CT scan performed after 91 months of treatment showed reduction of the tumor burden of up to 50% of the initial volume (Figure 2). No evidence of recurrent pulmonary metastases was found. After 109 months, the patient remains clinically stable and continues receiving thalidomide at a dose of 300 mg per day with no significant side effects.
Contrast-enhanced CT scan of the abdomen after 91 months of treatment with thalidomide in a patient with hepatic epithelioid hemangioendothelioma. The tumor burden diminished after therapy compared with baseline CT. Characteristic’s findings show diffuse hepatosplenomegaly with multiple focal hipervascular, with a target pattern of enhancement in larger lesions in the liver and hipovascular lesions in the spleen.
Epithelioid hemangioendothelioma is an uncommon vascular tumor of the liver with an unpredictable malignant potential and an intermediately aggressive biological course in between benign hemangioma and the highly malignant angiosarcoma.38 Its etiology and risk factors are not clearly known, but some possible etiologic factors include exposition to oral contraceptives, vinyl chloride, asbestos and the radioactive compound thorium dioxide, major trauma to the liver, viral hepatitis, primary biliary cirrhosis and alcohol consumption.3 Clinical presentation may vary from asymptomatic to the manifestations of portal hypertension or hepatic failure.1,2 At the time of diagnosis, up to 25% of patients are asymptomatic, incidentally diagnosed by radiology images, such as ultrasound, CT scan or MRI of the abdomen.9 Common clinical manifestations are right upper quadrant pain, hepatomegaly and weight loss. Physical examination may be normal or reveal hepatomegaly, splenomegaly, jaundice or signs of portal hypertension. In a recent review of 434 HEH cases reported in literature the most common clinical manifestations were right upper quadrant pain (48.6%), hepatomegaly (20.4%), and weight loss (15.6%).3 Most of these signs and symptoms previously described were present in our patient at the time of the diagnosis, but jaundice and portal hypertension were absent.
Laboratory parameters are abnormal in 84% of the patients, with altered liver chemistry tests being most the most common finding.3 Tumor markers (alpha-fetoprotein, carcinoembryonic antigen, and CA 19-9) are characteristically normal and are suitable for ruling out other primary or metastatic liver tumors.
Imaging studies in HEH patients may show solitary or diffuse nodular lesions with variable features on different techniques that suggest the diagnosis.910 The use of dual-time-point hepatic FDG-PET/CT imaging has also been recently shown to be useful for HEH diagnosis.11 However, definitive diagnosis of HEH requires histopathologic examination.13 In general, open wedge or core biopsy is sufficient to encompass the architectural features of HEH. Then, diagnosis is confirmed, as it was in our patient, by immunohistochemical demonstration of endothelial differentiation (Figure 1). In fact, immunohistochemistry staining is positive for endothelial cell surface markers such as CD31, CD34 and factor VIII-related antigen in nearly all cases of HEH (4). Other markers such as the angiogenic vascular endothelial growth factor (VEGF) and its receptors have been found in HEH.12
The natural history of the disease is not well understood. Analysis of untreated patients from large series reveals a 5-year survival of only 5%.3 This poor prognosis contrast with isolated reports of no progression or even spontaneous regression of the tumor,13 emphasizing the unpredictable malignant potential of HEH. No standard therapeutic strategies are at present established for HEH. Management of the disease depends of the presence of dissemination at the time of the diagnosis.
Clinical series report that at the time of diagnosis roughly 27% of the patients already have disseminated disease.4 Tumors restricted to the liver are candidates to surgery, either local resection or liver transplant.37 At the time of the diagnosis only 9% of patients presents with tumors susceptible to be handled with local resection, consequently liver transplantation has become the treatment of choice in patients with HEH, with clinical series showing encouraging results using this option with survival rates of 73% at 10 years.7 HEH is classically considered chemo and radiotherapy resistant and, therefore, these approaches are not considered useful in HEH.12 In our patient, the presence of extrahepatic disease led us to exclude transplantation as a treatment option and the use of thalidomide as anti-angiogenic therapy was intuitively proposed.14 At that time, no literature on the topic was available. More recently, at least two reports on the use of thalidomide in patients with EHE have been published. Mascarenhas reported the case of a man of 52 years-old with hemangioendotelioma of the liver with pulmonary metastases, successfully treated with the use of thalidomide15 and Kassam and Mandell16 incorporated thalidomide to a chemotherapeutic scheme aiming to achieve an anti-angiogenic effect. In our case we observed a reduction in liver size and a significant improvement of the performance status of the patient and no deterioration after more than nine years of follow-up.
Experimental data suggest that the anti-angiogenic potential of thalidomide is related to the inhibition of VEGF pathway.14 The fact that VEGF and its receptor has been shown to be present in HEH provide a rationale for the use of thalidomide in HEH.12 In fact, to target the VEGF pathway with newly-developed agents such as bevacizumab as well as sunitinib, sorafenib, and pazopanib represent promising therapeutic approaches for HEH.1718 Obviously, more studies are needed to confirm the utility of these agents as well as to identify which patients will benefit from them. Nevertheless, given the rarity of HEH and long term follow up needed to observe the progression of the disease or appearance of new lesions, it seems unlikely that controlled studies will be available soon. Based on our limited experience, we suggest that, considering its cost and safety profile, thalidomide is a reasonable option of treatment in patients with metastatic HEH compared with other anti-angiogenic drugs such as bevacizumab.