A 12-year-old girl with symptoms of fatigue, decreased exercise tolerance and progressive dyspnea (New York Heart Association functional class III) with a possible diagnosis of dilated cardiomyopathy secondary to viral myocarditis. Because of incessant wide QRS tachycardia refractory to antiarrhythmic drugs, she was referred for electrophysiological study. The diagnosis was idiopathic left ventricular tachycardia involving the posterior fascicle of the left bundle branch. After successful treatment with radiofrequency catheter ablation guided by a Purkinje potential radiological and echocardiographic evaluation showed complete reversal of left ventricular function in the first 3 months and no recurrence of arrhythmia during 2 years of follow up.
Niña de 12 años de edad con síntomas por fatiga, disminución de la tolerancia al ejercicio y disnea progresiva (clase funcional III de la New York Heart Association) con un posible diagnóstico de miocardiopatía dilatada secundaria a miocarditis viral. Debido a taquicardia con QRS ancho de comportamiento incesante refractaria a diversos fármacos antiarrítmicos fue referida para estudio electrofisiológico. El diagnóstico final fue taquicardia ventricular izquierda idiopática con participación del fascículo posterior de la rama izquierda. Después del tratamiento exitoso con ablación transcatéter con radiofrecuencia guiado por un potencial de Purkinje la evaluación radiológica y ecocardiográfica demostró reversión completa de la función ventricular izquierda en los primeros 3 meses y sin recurrencia de la arritmia durante 2 años de seguimiento.
Incessant or persistent tachycardia can lead to a clinical picture of dilated cardiomyopathy with left ventricular enlargement and impairment of systolic function. This phenomenon is particularly apparent in children with specific types of incessant supraventricular tachycardia as focal atrial tachycardia and permanent junctional reciprocating tachycardia.1–5 Reversibility of cardiac dysfunction has been shown after successful catheter ablation.1,2,6–9 On the other hand, ventricular tachycardia (VT) is relatively uncommon in children, but, idiopathic is the most frequent form in the observed cases of pediatric VT and most had right bundle branch block (RBBB) configuration with left superior axis deviation (LSAD), VT usually occurs in young individuals with structurally normal hearts and generally carries a good prognosis.10 Idiopathic incessant VT leading to a tachycardia-mediated cardiomyopathy is a very rare form of clinical presentation. We report reversal of myocardial dysfunction after catheter ablation of an incessant fascicular VT.
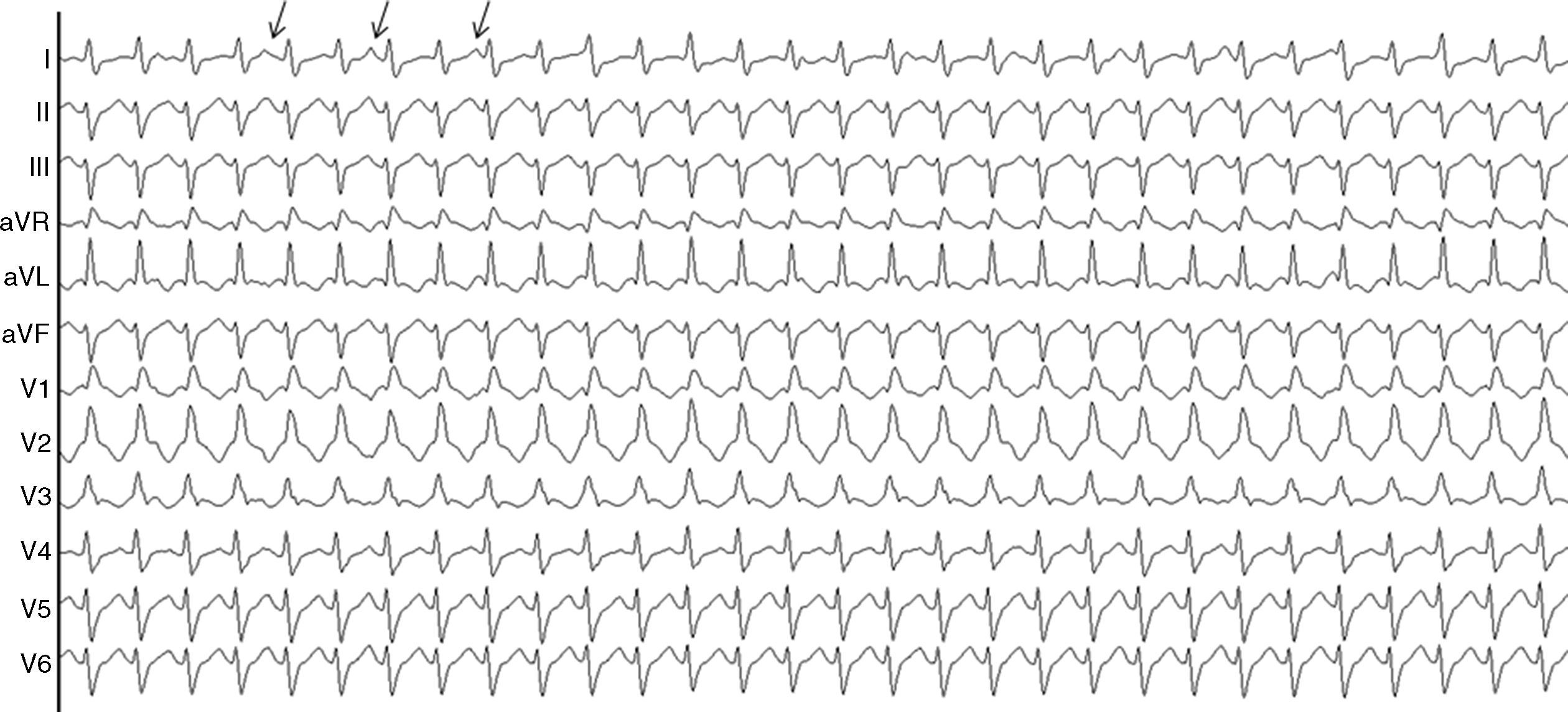
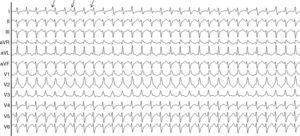
Case reportA 12-year-old girl was referred to the pediatric cardiology department for symptoms of fatigue, decreased exercise tolerance and progressive dyspnea (NYHA functional class III). She had a history of initially asymptomatic palpitations of undetermined date. A 12-lead electrocardiogram (12-lead ECG) (fig. 1) showed a regular and sustained wide complex tachycardia (mean heart rate: 167beats/min; QRS duration: 105ms) with LSAD in the frontal plane and RBBB morphology in the horizontal plane with a pattern of qR in V1, R in V2–V3, RS transition in V4 and rS in V5–V6 interpreted initially as supraventricular tachycardia with aberrant conduction due to characteristic response to intravenous verapamil. At that time, the tachycardia had a clinical paroxystic pattern. Chest X-ray on admission revealed cardiomegaly and cephalization of pulmonary blood flow. Two-dimensional and Doppler echocardiography showed bi-ventricular dilatation, left ventricle dimensions: end-diastolic 60mm; end-systolic 52.5mm, severe global hypokinesis with mild mitral and tricuspid regurgitation, pulmonary arterial pressure 54mmHg, and left ventricular ejection fraction (LVEF) 33% and fractional shortening 12.5% suggesting dilated cardiomyopathy.
12-lead ECG. Wide complex tachycardia (QRS 105ms, heart rate, 167beats per minute) with right bundle branch block morphology in the horizontal plane and left superior axial deviation in the frontal plane. Posterior fascicular ventricular tachycardia based on atrioventricular dissociation (arrows).
Medical therapy included digoxin, furosemide, spironolactone, enalapril, propranolol and amiodarone. Due to only mild clinical improvement, prednisone and azathioprine were indicated for possible diagnosis of dilated cardiomyopathy secondary to viral myocarditis. Immunosuppressive therapy was ineffective, thus, the patient was proposed to heart transplantation program.
At 14 years of age due to an incessant tachycardia pattern and refractory to antiarrhythmic drugs she was referred for electrophysiological study. The 12-lead ECG analysis was at first sight considered as fascicular ventricular tachycardia based on atrioventricular dissociation and typical pattern of RBBB QRS configuration with LSAD (fig. 1).
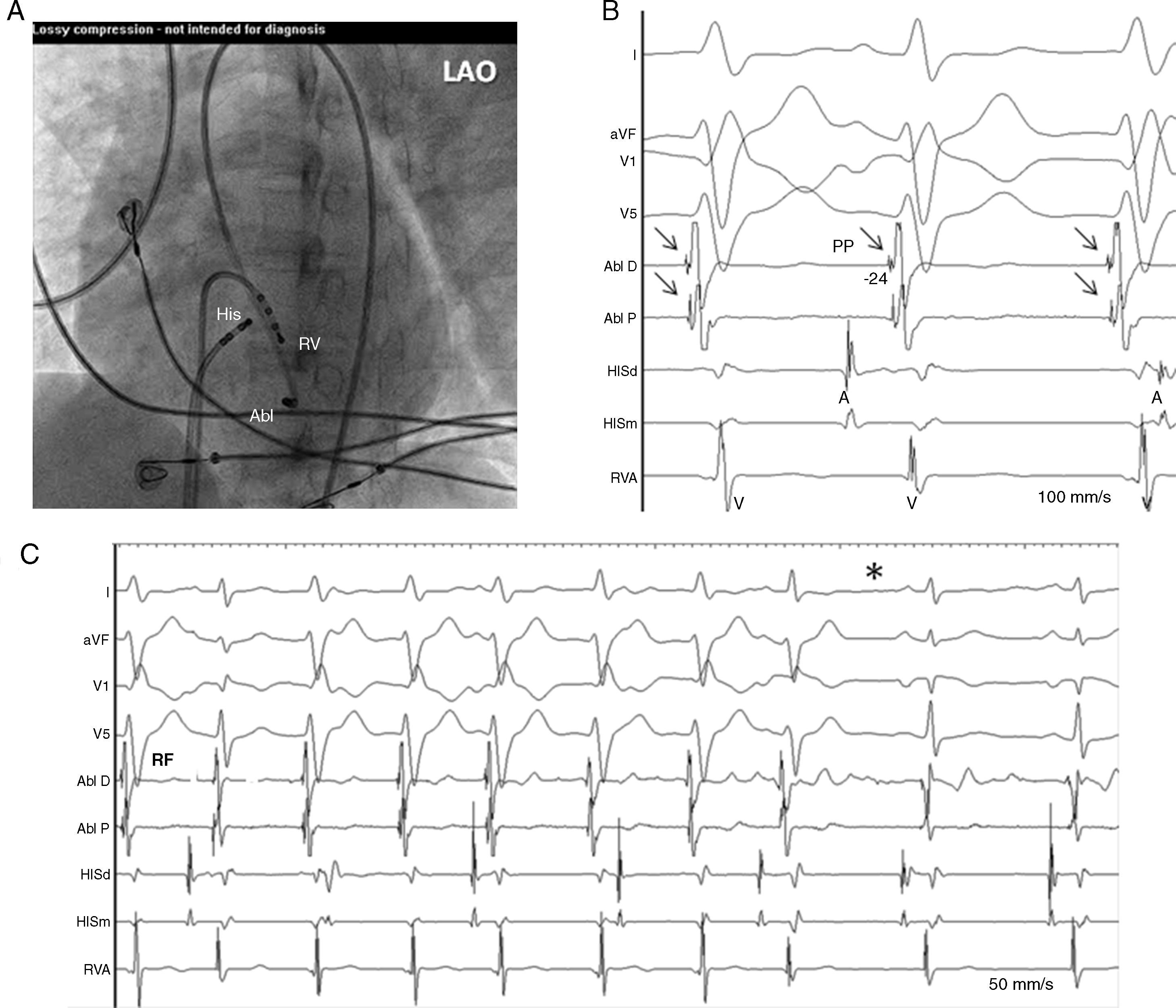
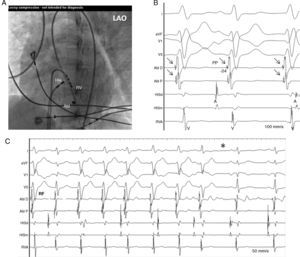
After written informed consent, electrophysiological testing was performed in a fasting and sedated state, Two 6-Fr Josephson quadripolar catheters (Biosense-Webster, USA) were inserted into the right femoral vein and placed under fluoroscopic guidance in the His bundle position and right ventricular apex. Endocardial mapping was performed during VT using a 5-Fr 2–5–2mm spaced decapolar catheter (Torqr, Medtronic, USA) introduced into the right femoral artery and advanced retrogradely into the postero-infero-apical septum of the left ventricle searching for the activation sequence and Purkinje potentials (Pp-QRS) during VT. Intracardiac mapping confirmed a reentry mechanism of tachycardia located in the posterior fascicle of the left bundle branch. Afterwards, the decapolar catheter was replaced with a 7-Fr, 4mm tip radiofrequency (RF) catheter (Stinger M curve B, Bard, USA) for TV mapping and ablation. RF catheter ablation was performed guided by a Pp-QRS recording (-24ms at successful site) during tachycardia and RF current was applied (Atakr II, Medtronic, USA) with an average power of 33 Watts and maximum temperature 51°C. (fig. 2). After a second successful application of RF current, programmed ventricular and atrial stimulation were performed without VT reinduction. Intravenous heparin in a bolus of 50U/kg and as an infusion of 1000U/h was administered during the procedure.
(A) Electrograms during VT showing recordings from distal to proximal sites (LV1–2, LV9–10) of decapolar mapping catheter located along the left ventricular septum. Earliest Purkinje potential (PP, arrows) was recorded at apical sites and activation sequence was toward the basal sites (long dotted arrow). (B) Fluoroscopic view showing catheter electrode positions. I, aVF, V1, V5 ECG leads; HIS; His bundle; RV, right ventricle; LAO, left anterior oblique.
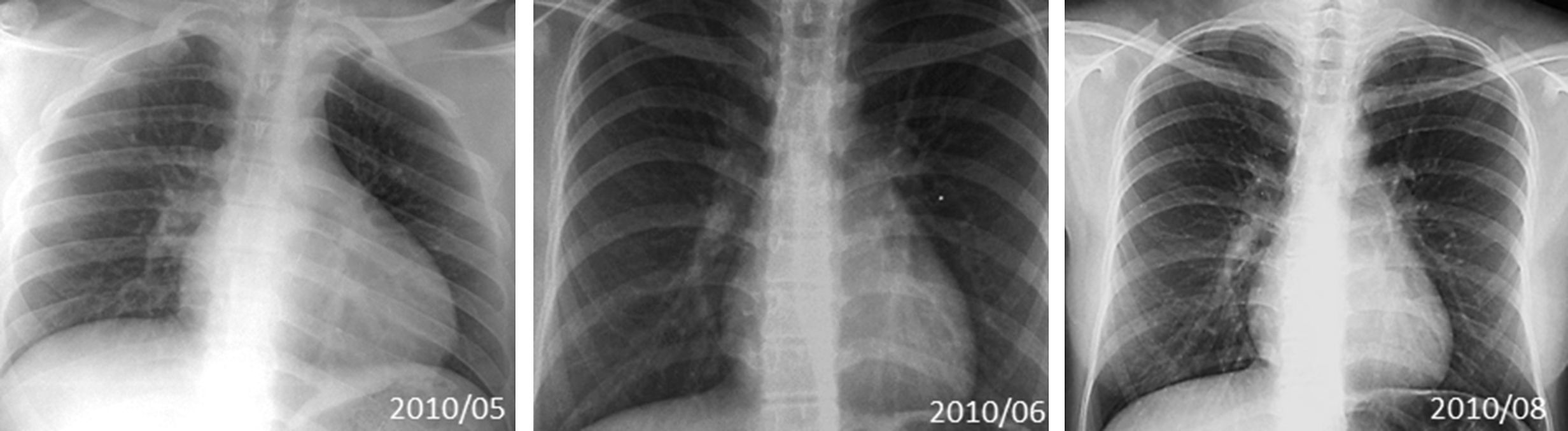
The patient was monitored for 2 days after catheter ablation and followed without any antiarrhythmic drugs. 24-hour Holter, chest x-ray, echocardiogram and treadmill exercise test were obtained in an outpatient basis at monthly intervals during the first three months. Follow-up showed progressive improvement until normalization of cardiac function by echocardiography with LVEF 68%. Fig. 3 shows the sequence of chest x-ray. The patient remained asymptomatic and tachycardia free after 2 years of follow-up.
DiscussionTachycardia-mediated cardiomyopathy (TMC) is defined as atrial or ventricular dysfunction caused by persistent abnormal high rates, but is reversible with cure of tachyarrhythmia.1,3,6,7 Different tachyarrhythmias have been reported to result in ventricular dysfunction especially in the context of supraventricular tachycardias.1–4,8,9 Notably, the automatic atrial tachycardia, which is a common cause of incessant tachycardia in children, is resistant to pharmacologic therapy and represents one of the most common etiologies of cardiomyopathy.11,12 Another common arrhythmia is the permanent junctional reciprocating tachycardia (Coumel) that is commonly incessant in infancy, even though it may not be recognized until adulthood and its persistent nature may lead to TMC.7
Few reports have described TMC secondary to ventricular tachycardias, mostly related with idiopathic right ventricular outflow tract tachycardia.13–15 Idiopathic fascicular ventricular tachycardia characterized by a pattern of QRS with RBBB and LSAD has a typical clinical presentation as paroxysmal and recurrent episodes and is intravenous verapamil-sensitive and is associated with good long-term prognosis.16,17 Clinical picture as an unusual incessant form is extremely rare and symptoms of congestive heart failure have been published in only some pediatric cases with normalization of left ventricular function after treatment with catheter ablation in a 17-year-old boy,18 15-months-old infant,19 12-year-old boy20 and 12-month-old baby21 all with a behavior similar to our case.
Several pathological changes have been described but it remains unclear as to whether they play an etiologic role or they arise as a consequence of the tachycardia. Sustained VTs are more common in structural heart disease, such as primary cardiomyopathy and cause-effect relationship may be confusing. Others, such as scar VTs after congenital heart disease repair, may compromise ventricular function. Sustained VT originating in the left ventricle in patients without detectable heart disease has been widely recognized and it has been demonstrated that the underlying mechanism is a reentry circuit that includes an anterograde slow conduction area with passive retrograde activation along the posterior fascicle during idiopathic left VT.22 A focal fibrosis not related with ischemia or myocarditis in close proximity to the left posterior fascicle was presumed to be the possible cause of the incessant behavior in an isolated case of fascicular ventricular tachycardia.23
Pathological changes include intense neurohormonal activation, high energy myocardial stores depletion, decreased beta-adrenergic responsiveness, abnormal calcium channel activity and sarcoplasmic reticulum calcium response.24,25 Histological changes include distortion of myocyte geometry, changes in myocyte contractile and relaxation properties and finally increased left ventricular wall stress and decreased left ventricular performance and myocardial fibrosis.26 TMC is a curable disease and should be suspected in any patient with decreased ventricular function in the setting of incessant tachycardia. As arrhythmias are frequently the result of cardiomyopathy, they are easily overlooked as the potential cause and it is difficult to determine whether the tachycardia is the cause or the result of cardiomyopathy, consequently, these patients can be easily misdiagnosed and potentially leading to inappropriate treatments. A high index of suspicion derived from history and clinical features remains the only available tool to diagnose a tachycardiomyopathy.
ConclusionFrom a practical standpoint, the presence of a tachycardiomyopathy should be suspected in any patient with congestive heart failure and persistent or incessant tachycardia.
FundingNo sponsorship of any kind was received to conduct this paper.
Conflicts of interestThe authors declare having no conflict of interest.