Aortic valve stenosis is becoming the most common valvular heart disease, with an increasing incidence in most countries.1 Coronary artery disease is highly prevalent in patients with aortic stenosis and could be present in up to 50% of the cases.2 Treatment with percutaneous implantation of a trans-catheter prosthetic aortic valve (TAVI) now offer an effective alternative with and acceptable survival rate in high to moderate risk severe aortic valve stenosis.3 So physicians and interventional cardiologists in particular, will soon be confronted with patients with these implanted prosthetic-valves that will need coronary angiography or intervention because of progression of ischemic heart disease.
We present a case of a patient with a previously implanted self-expandable aortic CoreValve® (Medtronic Inc., MN, USA), in whom a coronary angiography was done because of an acute coronary syndrome. We review some of the technical aspects of the procedure in this situation and review the literature.
A 68-year-old woman with severe symptomatic aortic stenosis and a high Euroscore, was treated successfully with TAVI using a CoreValve® system. The pre-implantation coronary angiography at the time revealed no significant lesions. She remained asymptomatic and in NYHA Class I. Two years after valve replacement, she began with a typical progressive effort-related chest discomfort. The physical exam was normal, with a minor grade I ejective aortic murmur and a normal carotid pulse with adequate-amplitude. The troponin-I levels were elevated 10 times the reference values and the electrocardiogram showed sinus rhythm, left bundle branch block with no abnormal ST-segment changes and an episode of self-limited ventricular tachycardia. The echocardiogram revealed a functionally normal prosthetic valve with no insufficiency, moderate ventricular hypertrophy with normal ejection fraction and no regional motion abnormalities.
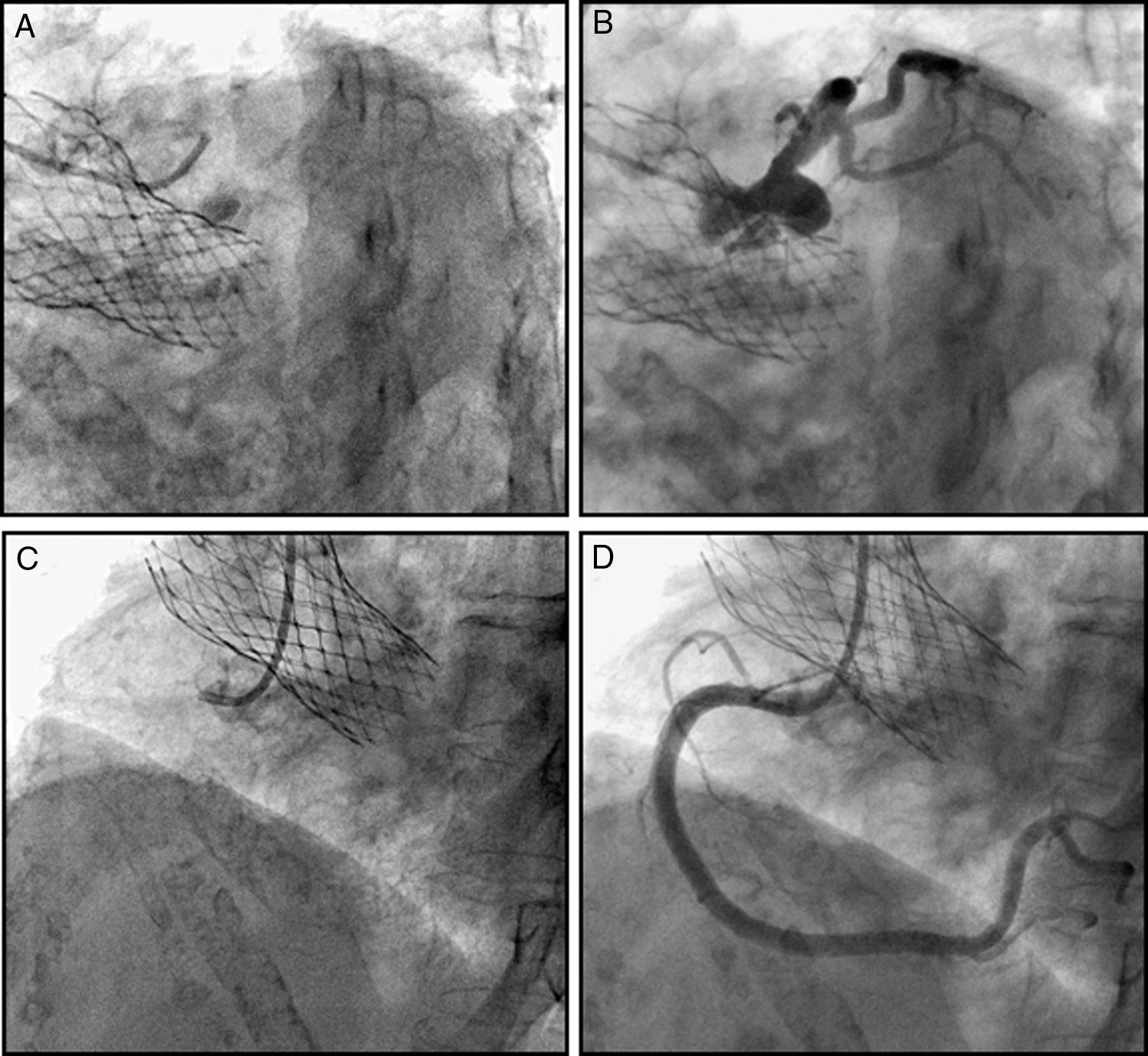
With the diagnosis of a non-ST segment elevation acute coronary syndrome (NSTE-ACS), coronary angiography was performed using the right radial approach. A pigtail angiographic catheter was initially used. The prosthetic valve was easily crossed and no trans-valvular pressure gradient was seen. Angiograms of the proximal aorta and left ventricle were done with the standard technique. No aortic insufficiency was observed. For the coronary angiography, a Tiger® (TIG) radial coronary catheter (Terumo Interventional systems) was used, and the left coronary artery was easily approached selectively through the prosthetic struts without any additional manipulation. The right coronary ostium could not be initially engaged with the same catheter even with the help of the guide-wire technique, but it was done directly with a JR4 Launcher® coronary catheter (Medtronic Inc.) (Fig. 1). No significant lesions were appreciated in either coronary artery. The sinus and ostia were not compromised and the distal coronary flow was normal. No additional imaging or provocative test was done in this case. The diagnosis of NSTE-ACS without obstructive coronary disease was established, either because of micro-vascular disease or secondary to the documented arrhythmia.
Coronary angiography with a CoreValve® implanted. Note the catheters passing through the prosthetic struts into the sinuses of Valsalva and into the coronary ostia, for a selective engagement (A, B) pre and post angiography of the left coronary artery in antero-posterior caudal view. (C, D) Pre and post angiography of the right coronary in left anterior oblique view.
Trans-catheter aortic valve implantation is a new therapy for patients with aortic stenosis, with a trend to be used not only in high-risk cases but more broadly in the low to intermediate risk group.3 By 2015, more than 80,000 Corevalve® systems have been implanted in more than 60 countries, and the numbers will increase dramatically.4 Coronary artery disease and aortic stenosis often co-exist and the severity of both pathologies is associated with worse clinical outcomes. With the long-term survival now achieved, the progression in severity of coronary lesions will certainly occur, and cardiologists and interventional cardiologists will be soon confronted with cases that will need coronary angiography in patients with a previous TAVI procedure.
In dealing with patients treated with TAVI it is important to know the characteristics and structure of each prosthetic valve (Table 1). The CoreValve® platform is a self-expandable nickel-titanium structure in which the tri leaflet bio-prosthesis made out of porcine pericardium is manually mounted. Above the 12mm conforming frame and sealing skirt at the aortic annulus, it has clear wide spaces between the rhomboid-shaped struts to allow adequate flow to the valve cusps and coronary arteries. It is important to note that some distance is left between the structure of the CoreValve® and the coronary ostia through the sinus of Valsalva.
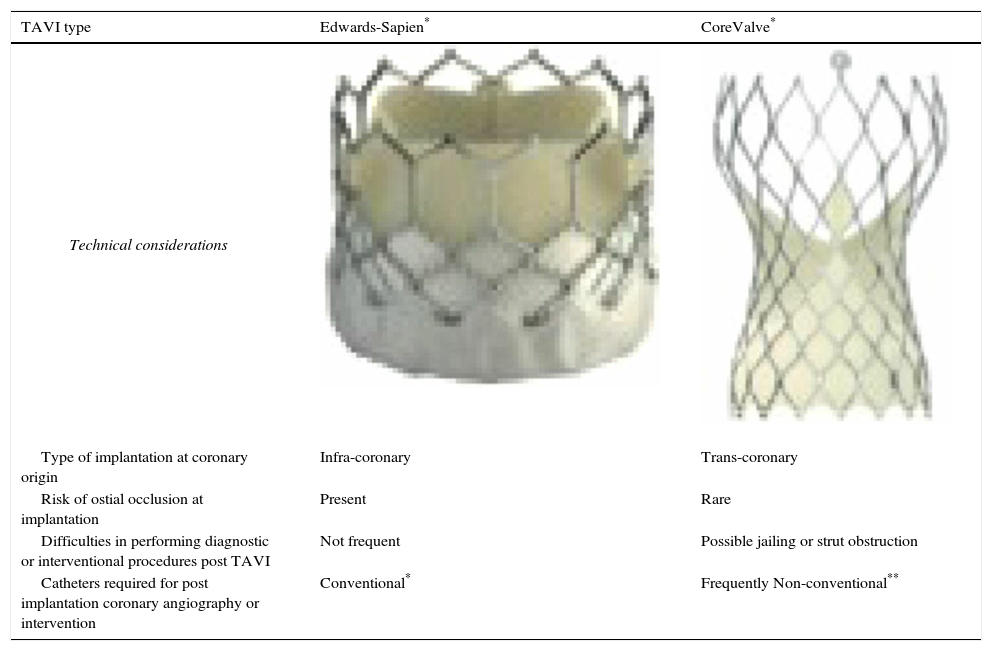
Differences between transcatheter aortic valve prosthetic systems, and technical considerations for coronary angiography or intervention post-implantation.
| TAVI type | Edwards-Sapien* | CoreValve* |
|---|---|---|
| Technical considerations | ||
| Type of implantation at coronary origin | Infra-coronary | Trans-coronary |
| Risk of ostial occlusion at implantation | Present | Rare |
| Difficulties in performing diagnostic or interventional procedures post TAVI | Not frequent | Possible jailing or strut obstruction |
| Catheters required for post implantation coronary angiography or intervention | Conventional* | Frequently Non-conventional** |
One good initial approach is to do an angiogram of the proximal aorta into the CoreValve® platform with a pigtail catheter in order to see the valve itself and locate the origin of both coronary arteries. It is important to move the angiographic catheter freely into the supra-valvular area to make sure it is not between the prosthetic metallic structure and the aortic wall.
In order to approach the coronary arteries selectively with this type of prosthesis, it is necessary to cross with the tip of the catheter through the frame of the valve's structure. As was mentioned, we could easily do so with the radial Tiger® (TIG) catheter (Terumo Interventional systems), and a JR4 Launcher® (Medtronic Corp.) without difficulties as the tip of the catheter passed though the rhomboidal strut.
It is important to note however, that selective coronary intubation is not always possible when these type of prosthesis are implanted because the struts can obstruct the access to at least one of the coronary arteries. Blumenstein et al.,5 reported a series of 1000 consecutive patients with TAVI and 35 needed coronary angiography or intervention after the implantation. Accessibility and selective coronary engagement was possible in all of the cases with sub-coronary valves (Sapien® type). Ten patients had a CoreValve® previously implanted. Coronary artery angiography in this group was more difficult and although it could be adequately evaluated in 90% of cases, most of them required the use of different “non-conventional” catheters (JL3.5, AR1), or unselective injection. In one patient the coronaries could only be displayed unselectively via aortography. No intervention was necessary in neither of these patients.
In our case no coronary intervention was needed but angioplasty and stenting could be necessary and has been described in patients with an implanted CoreValve®. In the first successful published case,6 a two-vessel angioplasty and stenting of the left anterior descending and circumflex arteries was done using a standard 6Fr JL4 Launcher® guiding catheter (Medtronic Inc., MN USA) and in other two patients even with post-CABG conventional catheters were also used.7 Other reported cases needed unconventional catheters, or in a case of an “imprisoned” ostium by the valve structure, a “mother-and-son” or “proboscis” technique was utilized with a Heartrail® 5Fr catheter (Terumo Interventional Systems) through a 7Fr JF4 guiding catheter to cross through the struts, and the angioplasty was successfully done.8
The presence of significant coronary lesions documented at the time of a TAVI procedure, can be treated in the same session in particular with the Edwards Sapien®-type infra-coronary systems,3,9 even in patients with left main proximal obstructions.10 The feasibility of doing dual valvular and coronary intervention in the same session, using a Corevalve® system will be clarified in the ongoing SURTAVI and ACTIVATION trials.
Coronary angiography and angioplasty will be required in a growing number of patients with the self-expandable CoreValve® or other percutaneous aortic prosthesis in the near future. As in this case the procedure could be done through the prosthetic struts without any complications, but the interventional cardiologist should be aware that different catheter shapes or other maneuvers can sometimes be necessary because of obstruction or imprisoning of the coronary access.