Several major conceptual advances influence contemporary evaluation and management of patients with a myocardial infarction. We now consider myocardial infarction one element in the spectrum of acute coronary syndromes.1 The term "acute coronary syndromes" is currently used to denote individuals who present without ST-segment elevation on the 12-lead electrocardiogram (unstable an-gina/non-ST-elevation myocardial infarction [NSTEMI]) and with ST-elevation on the 12-lead electrocardiogram (ST-elevation myocardial infarction - STEMI). In 2000, the definition of a myocardial infarction was updated, with a major focus on the use of cardiac specific troponins as the preferred biomarker indicating myocardial necrosis.2 The introduction of cardiac specific troponins had a greater influence on distinguishing unstable angina from NSTEMI rather than impacting on the diagnosis and management of patients with STEMI. It is also recognized that myocardial infarction is not a fixed process at the time of occlusion of the coronary artery but rather is a dynamic process with a wavefront of necrosis sweeping through the zone of the myocardium at risk. Despite the many promising interventions identified in laboratory studies for modification of infarct size, relatively few have been adopted into routine clinical practice with the exception of timely reperfusion of the infarct related artery.1
Evidence that drives our thinking about the approach to management of patients with ST-elevation myocardial infarction comes from several sources: randomized controlled trials and registries. We learned from randomized controlled trials that administration of a fibrinolytic is associated with 18% reduction in 35-day mortality compared with placebo.3 Numerous randomized controlled trials documented the superiority of primary percutaneous coronary intervention (PCI) over fibrinolysis for reducing mortality in STEMI, provided primary PCI can be performed by a skilled operator, supported by an experienced team, and delivered in a timely fashion.1
Against the background described above, one must also note the advances in treatment of risk factors for heart disease. This includes more widespread use of sta-tins for lowering cholesterol, more aggressive treatment of hypertension, and greater use of aspirin both in primary prevention and secondary prevention, and public health campaigns to promote cessation of cigarette smoking.4 Evidence exists in the United States that there is a decline in hospitalizations for acute myocardial infarction.5,6 The studies focusing on this epidemiologic observation usually do not distinguish between NSTEMI and STEMI, because the information comes from administrative databases with limited clinical information.5,6
The decline in hospitalization rates for acute myocardial infarction in the United States is seen both in patients greater than age 65 as well as those between ages 45 and 64.6 Much of the improvement appears to be due to better primary prevention of the risk factors noted above.6 Of note, a disturbing trend of an alarming increase in obesity and type II diabetes mellitus may blunt some of the gains in reductions in hospitalization for acute myocardial infarction as well as reduction in mortality from cardiovascular diseases.7
Registry reports provide information on the use of treatments in a real world situation. They complement randomized controlled trials since they are less restrictive and are not affected as much by the enrollment criteria so central to a randomized controlled trial. National registries that span multiple geographic locations in a given country are of particular interest since they provide data on a range of treatments for patients with heart disease; can help identify regional variations in treatment; and may serve as the stimulus for community based efforts to provide improved systems of care for patients with heart disease. For example, the French nationwide USIC 2000 registry prospectively collected all cases of STEMI in November 2000.8 A total of 369 intensive care units in France (83%) of the 443 centers treating patients with myocar-dial infarction participated. In 2004, an important observation from the USIC 2000 registry was published; the 1-year outcome of patients treated with prehospital thrombolysis compared favorably with that of patients treated with other modes of reperfusion therapy, including in-hospital thrombolysis and primary PCI.8
Risk assessment is an integral part of the care of patients with acute coronary syndromes. A thorough evaluation of risk informs decisions regarding triage among levels of hospital care, and the need for transfer to tertiary centers. Increasing economic pressures have intensified attention to these triage decisions as well as to allocation of clinical resources more broadly. Estimates of patient risk impact the selection between alternative therapeutic strategies and provide valuable information for patients and their families. Tools that aid in accurate risk stratification are useful for emergency medicine physicians, internists, and cardiovascular specialists. Risk stratification in myocardial infarction can be based on clinical examination as proposed by Killip and Kimball in 1967,9 hemodynamic monitoring as proposed for Forrester et al. in 1976,10 or an integrated assessment of clinical and laboratory findings.11 Although it occurs in a minority of patients with STEMI, bundle branch block has been consistently identified as a predictor of adverse outcome. The HERO-2 investigators reported that bundle branch block was seen in 5.11% of subjects in that randomized controlled trial; 1.76% had left bundle branch block and 3.3% had right bundle branch block.12 Right bundle branch block accompanying anterior STEMI at presentation and new bundle branch block (including left bundle branch block) early after fibrinolytic therapy were identified as independent predictors of high rates of 30-day mortality.12
In this issue of Archivos de Cardiologia de Mexico, Juarez-Herrera and colleagues provide an important contribution from the RENASICA II national multicenter registry in Mexico.13 In this registry of 8098 patients with an acute coronary syndrome enrolled in 66 primary and tertiary care Mexican hospitals, 4555 (56%) were found to have STEMI. Patients with a previous bundle branch block were excluded. A total of 318 (7%) patients had a right bundle branch block in association with STEMI and 227 (5%) had a left bundle branch block in association with STEMI. In a multivariable regression analysis, both left and right bundle branch block were associated with significant increase in-hospital mortality (OR 1.7).13 Although not statistically significant, the rates for in-hospital mortality, recurrent angina, and recurrent myocardial infarction were all numerically higher in the subjects who had a right bundle branch block compared with a left bundle branch block.13
How should we use this information about the increased risk of bundle branch block in patients with STEMI, in one case reported from the randomized trial (HERO-2) and in another case from a national registry (RENASICAII)?12,13 First, in contrast to the general clinical cardiology observation outside of the setting of STEMI, where left bundle branch block is associated with a higher rate of adverse events than right bundle branch block, in the setting of STEMI both forms of bundle branch block carry adverse prognostic information and right bundle branch block may even be slightly worse. Juarez-Herrera and colleagues provide an excellent summary of the potential biologic explanations relating bundle branch block and adverse prognosis.13 Essentially, these explanations reduce down to bundle branch block being a surrogate marker for extent of left ventricular dysfunction, probably resulting from more proximal occlusion of the infarct related artery (usually the left anterior descending coronary artery). It is likely that inclusion of right bundle branch block in future iterations of risk scores for patients presenting with STEMI will help refine the predictive ability of such risk scores to discriminate among STEMI patients along a continuum of risk of adverse outcomes.
But the situation is not as simple as inserting a temporary or permanent pacemaker to deal with the bundle branch block and presumed increased risk of higher grade AV block. Since it is really the underlying amount of left ventricular myocardium that becomes necrotic in the setting of STEMI, it is unlikely that pacemaker therapy will have a significant beneficial impact on the long-term outcome of patients with bundle branch block and STEMI.
This brings us to the broader implications of the report by Juarez-Herrera et al.13 Mexican investigators made an important contribution to the international study ExTRACT-TIMI 25, investigating the low molecular weight heparin enoxaparin compared with unfractionated heparin as adjunctive antithrombotic therapy to support fibrinolytic therapy for STEMI.14 Several of the sites participating in the ExTRACT-TIMI 25 study also participated in the ExTRACT-TIMI 25 registry, enrolling patients in an international STEMI registry outside the boundaries of the clinical trial - 245 subjects were enrolled in the ExTRACT-TIMI 25 registry from Mexico.15 Comparing the clinical characteristics of patients in the ExTRACT-TIMI 25 trial, ExTRACT-TIMI 25 registry and the individuals with right and left bundle branch block in the RENASICA-II registry, several notable observations can be made. The patients with bundle branch block in RENASICA II had much higher rates of cigarette smoking and diabetes mellitus - two important risk factors that probably translate into more extensive coronary artery disease. In addition, the patients with bundle branch block in RENASICA II had lower rates of treatment with beta blockers, inhibitors of the rennin-angiotensin-aldosterone system, thienopyridines, and statins than patients in the ExTRACT-TIMI 25 reports.13,15 (Compare Table II in the paper by Steinberg et al. with Tables 1 and 2 in the paper by Juarez-Herrera et al.) Of critical importance, only 29% of patients in the ExTRACT-TIMI 25 Registry failed to receive reperfusion for STEMI, while about 50% of the patients with bundle branch block in RENASICA II did not receive reper-fusion treatment.13,15
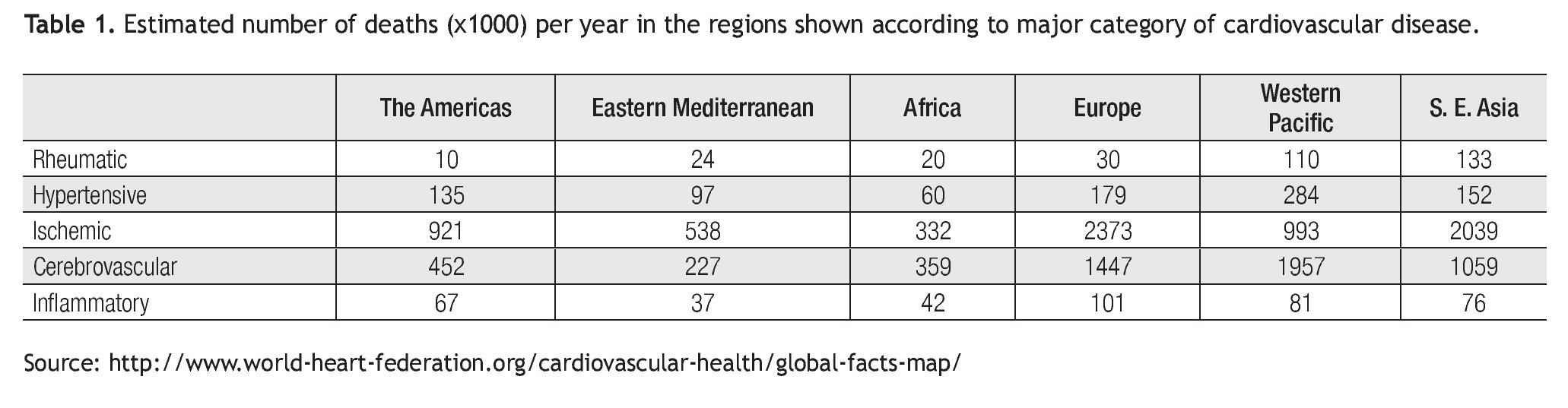
Thus, the data on bundle branch block and morbidity/mortality in STEMI in RENASICA II provide the evidence for a call to action. It is now recognized that chronic illnesses such as coronary heart disease account for a substantial portion of the global burden of disease (Table 1).16 Although there are gratifying trends towards a reduction in heart disease-related deaths in high income/high technology countries such as the United States, it is a disturbing fact that heart disease remains the leading cause of death in the United States and a major source of healthcare expenditures.17 Chronic diseases affect low and middle income countries severely and may account for twice as many deaths compared with communicable diseases, maternal/fetal conditions, and nutritional deficiencies combined.16
What action items are needed in Mexico based on these reflections on the RENASICA II data? There is an urgent need to develop systems of care to increase the proportion of patients with STEMI who receive reperfusion therapy.18 A major focus should be directed to providing optimal medical therapy after myocardial infarction - a proven approach to reduce mortality.19
The report by Juarez-Herrera and colleagues is to be commended for its important scientific contribution and insights it provides in the path forward for improving outcomes of Mexican patients with STEMI.13 There is a strong precedent in Mexico for improvement in health-related affairs. The efforts of the Secretariat of Health of Mexico were associated with an improvement in the proportion of patients in the State of Veracruz with good control of diabetes from 28% to 39%.16 Air pollution, a contributor to the development of coronary heart disease, has been dramatically reduced in Mexico City compared with the 1990s.20 The leadership and foresight that envisioned the need for a national registry such as RENASICA II must now be channeled into an action plan to translate the findings into public policy to improve cardiovascular health in Mexico.
Corresponding author: Elliott M. Antman,
Brigham and Women's Hospital. Cardiovascular Division. Francis Street, Boston, MA. USA 02115.
617-732-7149 (Office) 617-975-0990 (Fax).
E-mail: eantman@partners.org
Received: April 12, 2010;
accepted: June 17, 2010.