Introduction
Data coming from reperfusion era showed,1 that bundle branch block (BBB) in early acute phases of ST-elevation myocardial infarction (STEMI) had close relationship with high mortality.2 Although, the evidences3 suggesting that the real incidence of a BBB is variable, higher incidence of right bundle branch block (RBBB) over left bundle branch block (LBBB) has been identified. In patients with RBBB extensive jeopardized myocardium involving interventricular septum, could induce a worse in-hospital outcome. In addition, on ECG bases it is not possible to separate new or presumably new conduction disturbances from a pre-existing condition. The purpose of this post-hoc subs-tudy was to identify in-hospital outcome and prognostic value of RBBB in STEMI from the largest Mexican acute coronary syndromes registry .4
Methods
The characteristics of RENASICA II registry has been previously published,4 in brief: it is a prospective and observational registry of the Mexican Cardiology Society that included 8098 patients with final diagnosis of acute coronary syndrome. The main target was to identify a representative population to know diagnosis, stratification and treatment trends. Patients were enrolled in primary and tertiary hospitals. To improve the quality of data, criteria of Alpert were used. The hospital varied in terms of access to on-site cardiac catheterization, number of acute care beds and the type of practice setting. Patients were selected during the hospital admission if they had high clinical suspicion of acute coronary syndromes with symptoms and signs of acute ischemia, with or without electrocardiographic changes, with necrosis or not and proved ischemic heart disease by invasive or non invasive test at discharge. Patients with symptoms precipitated by anemia, hypertension, and heart failure or another secondary condition were not considered. On admission and discharge nomenclature with or without ST elevation was standardized. All treatment decisions were made at discretion of treating physicians. In RENASICA tertiary hospitals with capabilities for coronary arteriography, percutaneous transluminal coronary angioplasty (PTCA) and coronary artery bypass graft (CABG) surgery enrolled 90% of the patients.
In this substudy, STEMI patients plus LBBB or RBBB were compared in terms of in-hospital outcome and MACE (cardiovascular death, recurrent ischemia and reinfarction).
Clinical and electrocardiographic criteria: 1) Characteristics and definitions of STEMI patients in RENASICA II have been previously published,4 2) LBBB under universal criteria with ≥ 120 msc QRS duration. Exclusion criteria: a) acute ischemia precipitated by anemia, hypertension, heart failure or another secondary condition, b) well identified previous BBB and pacemaker rhythm.
RBBB definition: QRS duration ≥ 120 msc, with an rsr', rsR' in V1 or V2 leads, R wave notched in V1 with prolonged R wave peak time > 50 msc in V1 and normal peak time in V5 and V6. Leads DI and V6 had to show a QRS complex with a wide S wave > R duration or > 40 msc.5 ST segment deviation was measured at maximum J point. Abnormal Q waves were interpreted according to the European Society of Cardiology / American College of Cardiology consensus.6
Statistical Analysis: To analyze the clinical characteristics through non-parametric and parametric variables chi-squared test and Student t test were used. To determine a normal or abnormal distribution, Wilcoxon rank sum test was considered. To analyze the relationship among mortality and mortality markers Pearson's correlation analysis was performed. Through univariate, logistic and multivariate regression analysis, we examined the relationship between variables for atherosclerosis (smoking habit, diabetes mellitus, systemic hypertension and dislipidemia, etc.) and bad outcome (> 60 years of age, diabetes mellitus, anterior or extensive infarct, LBBB, ventricular dysfunction, and expulsion fraction < 40%) with mortality. To evaluate the relationship between each marker and other variables a multivariate Cox proportional hazard model was used. A p <0.05 was considered statistically significant. Data are presented in percentages, mean standard deviation or median values, odds ratio (OR) and confidence intervals 95% (CI).
Results
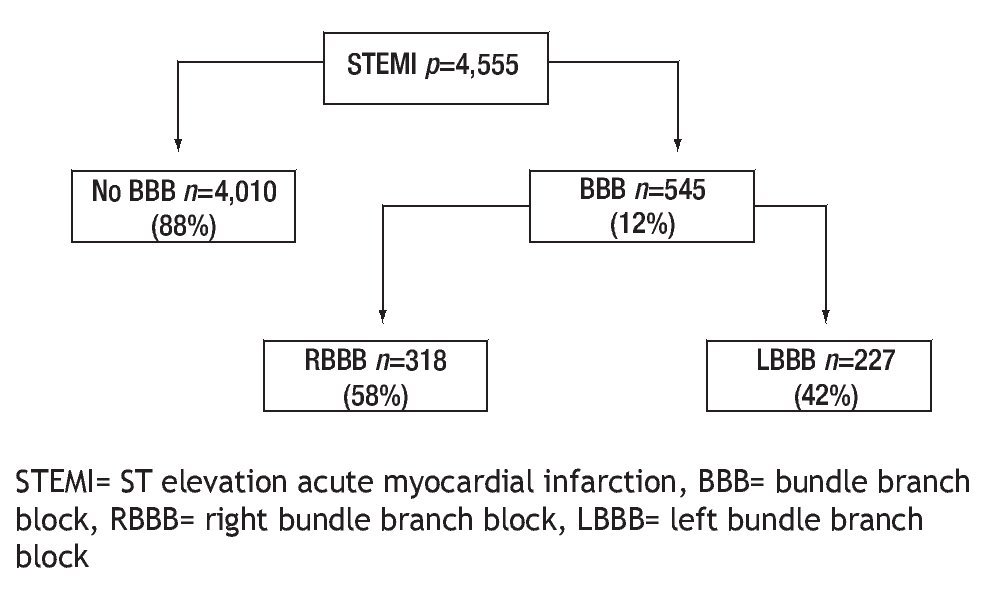
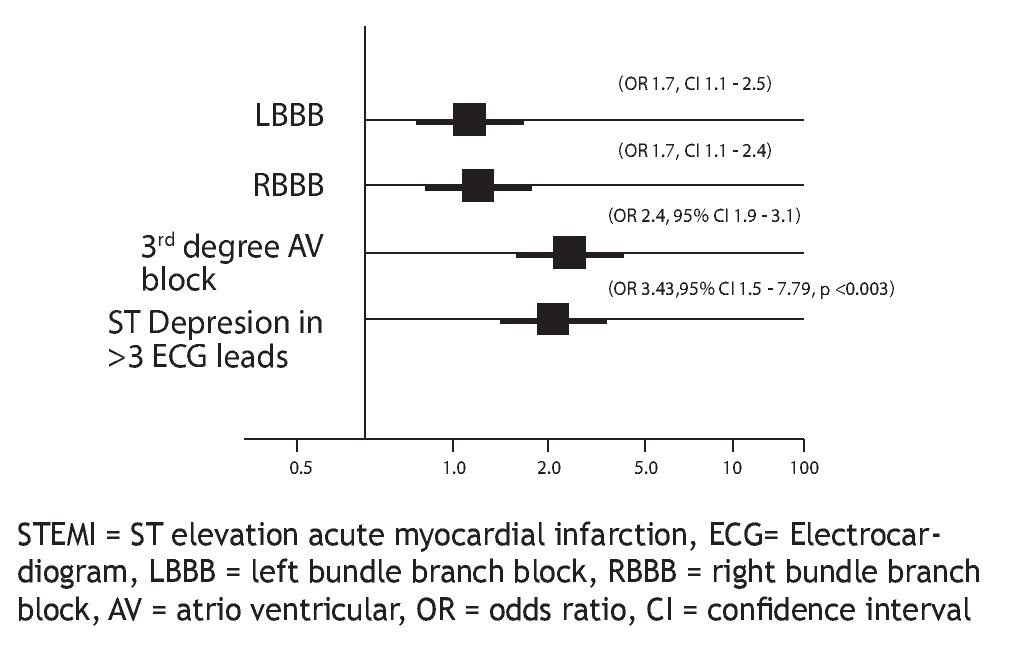
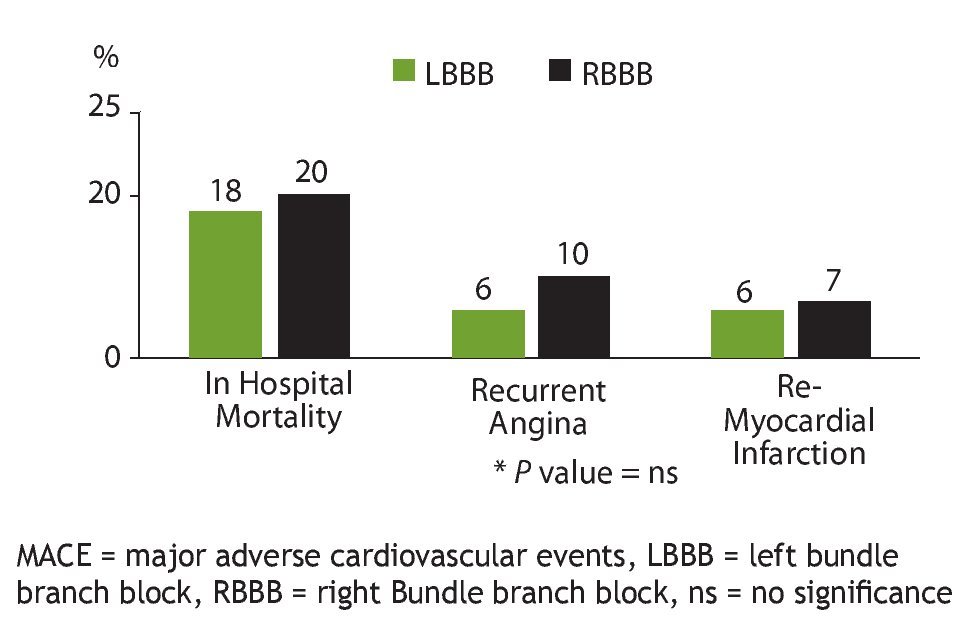
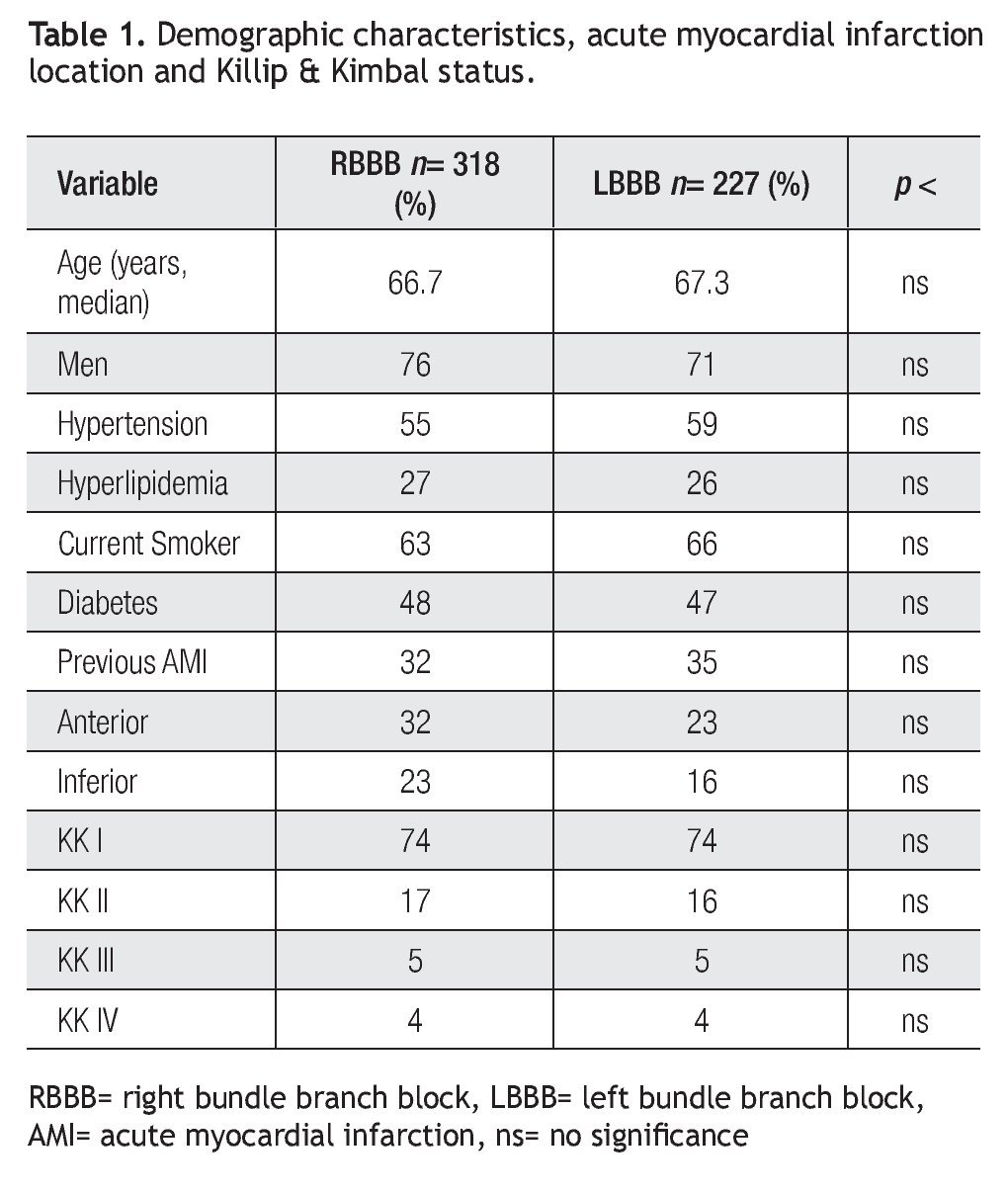
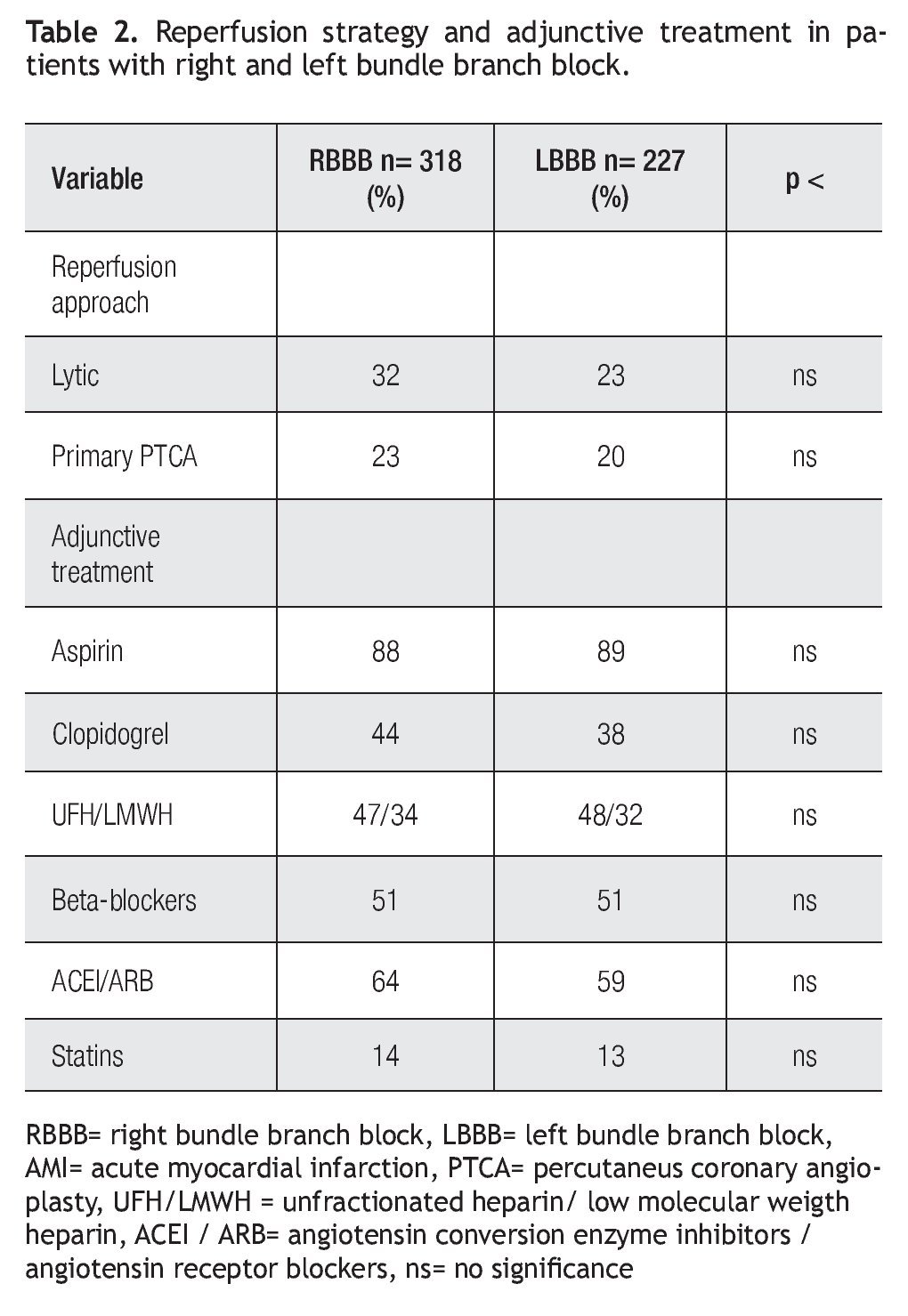
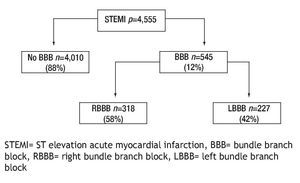
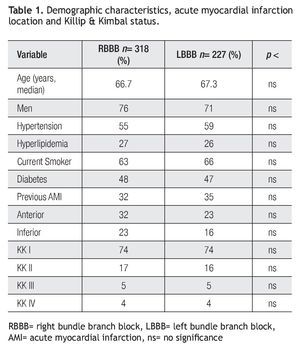
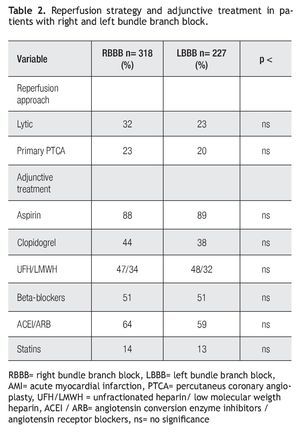
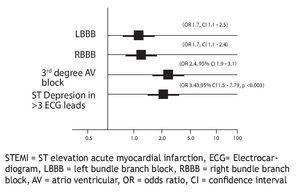
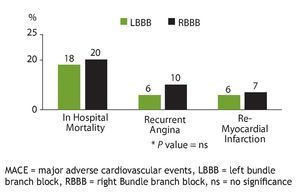
RENASICA II registry enrolled a total of 8098 patients, 4555 with final diagnosis of STEMI, of these; 4010 patients without BBB (88%) and 545 patients with BBB (11.9%) were analyzed in this sub-study (Figure 1). In this group, 318 (58.3%) had RBBB and 227 (41.6%) LBBB. Table1 shows demographic characteristics in both groups, AMI location and Killip & Kimbal status. Table 2 shows reperfusion strategy and adjunctive treatment. Regarding age, major risk factors, AMI location, clinical expression of left ventricular dysfunction, reperfusion strategies and adjunctive treatment no statistical differences were observed. A trend for male gender, incidence of anterior or inferior AMI, pharmacological or mechanical reperfusion was observed in patients with RBBB compared to LBBB group. Low use of reperfusion strategies and optimal treatment was observed in both groups. In terms of mortality no statistically significant difference was observed among RBBB group compared with LBBB patients (20% vs. 18%, p = ns). Among 4555 STEMI patients, 1685 (37%) were under fibrinolytic therapy, the time to onset symptoms and drug administration was < 2 hours in 31%, from 2 to 4 hours in 36%, 4 to 6 hours in 19% and finally > 6 hours in 15%. Primary or facilitated PTCA were performed in 15%. A logistic regression analysis performed to assess the effect of independent variables on mortality while adjusting for potentially confounding factors identified ECG findings as in-hospital mortality predictors (Figure 2) including RBBB (OR 1.70, 95% CI 1.19 - 2.4, p < 0.0003), LBBB (OR 1.7, 95% CI 1.1 - 2.5, p = 0.007), AV block high-degree (OR 2.99, 95% CI 1.9-3.1) and STEMI plus ST depression > 3 ECG leads (OR 3.43, 95% CI 1.51 - 7.78, p = 0.003). Several multivariate regression models were applied to identify stronger correlation and a higher statistical significance for mortality. In-hospital outcome and MACE are shown in Figure 3. A high incidence of cardiovascular mortality and MACE were observed in both groups.
Figure 1. RENASICA II Substudy patients recruited.
Figure 2. ECG findings and logistic regression in hospital mortality predictors in ST elevation acute myocardial infarction.
Figure 3. Outcomes and in hospital comparison of MACE in both bundle branch block.
Discussion
Our data show four important findings. First, in-hospital outcome of STEMI patients with BBB was characterized by a high mortality. Second, as compared with LBBB, RBBB ECG finding was a mortality predictor too. Third, focus in low use of reperfusion strategies and optimal adjunctive treatment is mandatory. Fourth, this could be the first evidence about the outcome of STEMI patients complicated with BBB coming from a Mexican representative population.4
In the setting of STEMI, the clinical relevance of BBB has been established before and after reperfusion era.7 In the Fibrinolytic Therapy Trialist's,8 the mortality with or without thrombolysis was 19% and 24% respectively in the first 35 days. The studies did not establish any distinction between RBBB or LBBB and did not specify if BBB were new or not. Different types of BBB occurring during the initial hours of AMI with different prognostic implications that is independent of other prognostic factors.
In our substudy, patients with RBBB had trend to major incidence of anterior or inferior infarction compared to LBBB group. In these patients ECG criteria for diagnosis of STEMI with LBBB possibly were not used. An analysis based on simple ST segment changes, may help identify patients with acute myocardial infarction who can then receive an appropriate reperfusion treatment .9
In the earliest phase of STEMI, independently of other prognostic factors, several types of BBB occurred with different prognostic implications. In our study it was not possible to identify the new appearance of BBB. This abnormal conduction disturbance in a patient with acute chest pain is highly suggestive of infarction. Ischemic changes superimposed on a pattern of chronic LBBB are easy to recognize when a previous ECG is available for comparison. The timely availability of a previous ECG, however, is the exception rather than the rule. An important issue of this study is that physicians at emergency room department have to decide to administer appropriate reperfusion strategy on the basis of only the most recent ECG.9
An interesting finding in this study was the relationship among STEMI, RBBB and high incidence of MACE. Several anatomic conditions could explain this outcome. a) Abnormal conduction disturbance traverses the interventricular septum toward the cardiac apex; b) in anterior acute myocardial infarction, the proximal occlusion of the left anterior descending artery produces ischemia of the septum and RBBB; c) sometimes, RBBB and LBBB divide into multiple portions with an atrio-ventricular branch, constituting a true bifascicular conduction abnormality, with a distribution network of anterosuperior and central fibers.10 This variable anatomy in the conduction system produces variations when ischemia or necrosis occurs and causes conduction disturbances in STEMI, explaining the variable incidences and prognostic meanings of the left fascicular blocks occurring simultaneously to RBBB.11 The contributions from the Mexican school of electrocardiography in the diagnosis of RBBB has been described in three elegant terms: a) without "jumping-wave" phenomenon or minor grade block , b) with "jumping-wave" phenomenon , and c) with limited "jumping-wave" phenomenon or intermediate grade block. The last two types are associated to ischemic conditions and dead septal tissue.12, 13
In the present study patients with RBBB with anterior location AMI had a trend to high in-hospital mortality compared to LBBB patients. This mortality in STEMI and RBBB may be explained by septal ischemia from a more proximal left anterior descending artery occlusion (before the large septal branch). It is important to emphasize than RBBB was a consistent risk marker, as strong as, LBBB for in-hospital mortality. A wider QRS duration (≥ 160 msec) during anterior STEMI and RBBB may reflect more extensive ischemia in the conduction system; currently this ECG finding has been used in the risk stratification.14 In addition, the observed mortality rates in STEMI were higher than expected and higher than reported previously,4 this was not unexpected since a substantial proportion of patients had not access to reperfusion facilities. Left ventricular dysfunction was the most important MACE and the strongest mortality predictor, which is in line with the low incidence of reperfusion approaches and possible long ischemia time. New pharmacological reperfusion directions including FT bolus, as is currently used in several countries, might improve even further STEMI outcome. Current evidence to use an optimal treatment (clopidogrel, enoxaparin and statins) was obtained after RENASICA.15 -17
Clinical Implications: Abnormal conduction disturbances plus ST depression > 3 leads, in the setting of STEMI allowed to identify a high risk group to in-hospital mortality (Figure 2). Prompt recognition and reperfusion strategies should improve survival. In addition, physicians have to have in mind that the timely availability of a previous ECG is the exception rather than the rule. At emergency room department, physicians in charge have to decide reperfusion strategies on the basis of only the most recent ECG. Considering the significant proportion of patients without any reperfusion strategy, new directions from the Health System and Mexican Cardiology Society are required to improve quality of care.
Limitations: As in all clinical trials, a selection bias could have occurred in RENASICA II resulting in under-representation of very high-risk patients, including those with RBBB accompanying anterior STEMI in the trial cohort. In addition, the ECG interpretation was not performed in all centers by experts in electrocardiography. Thus, it is not possible to study the different types of RBBB. As this was a transversal study, it was not possible to identify if BBB was a new condition.
Conclusion
In STEMI RBBB was an independent predictor of high inhospital mortality and had at least the same risk implication than LBBB. Both should be considered in risk stratification to identify high risk patients.
Corresponding author: Carlos Martínez-Sánchez.
Coronary Care Unit of Instituto Nacional de Cardiología Ignacio Chávez. Juan Badiano No. 1. Tlalpan. Mexico City. Col Secc. XVI ZC 14080
Tel-Fax (+52+55) 54 85-99-99.
E-mail:carlos.martinez@cardiologia.org.mx
Received in June 1, 2009;
accepted in February 15, 2010.