Cardiac complications in infectious endocarditis (IE) are seen in nearly 50% of cases, and systemic complications may occur. The aim of the present study was to determine the characteristics of inpatients with IE who suffered acute neurologic complications and the factors associated with early mortality.
MethodsFrom January 2004 to May 2010, we reviewed clinical and imaging charts of all of the patients diagnosed with IE who presented a deficit suggesting a neurologic complication evaluated with Computed Tomography or Magnetic Resonance within the first week. This was a descriptive and retrolective study.
ResultsAmong 325 cases with IE, we included 35 patients (10.7%) [19 males (54%), mean age 44-years-old]. The most common underlying cardiac disease was rheumatic valvulopathy (n=8, 22.8%). Twenty patients survived (57.2%, group A) and 15 patients died (42.8%, group B) during hospitalization. The main cause of death was septic shock (n=7, 20%). There was no statistical difference among groups concerning clinical presentation, vegetation size, infectious agent and vascular territory. The overall number of lesions was significantly higher in group B (3.1 vs. 1.6, p=0.005) and moderate to severe cerebral edema were more frequent (p=0.09). Sixteen patients (45.7%) (12 in group A and 4 in group B, p=0.05) were treated by cardiac surgery. Only two patients had a favorable outcome with conservative treatment (5.7%).
ConclusionsIn patients with IE complicated with stroke, the number of lesions observed in neuroimaging examinations and conservative treatment were associated with higher in-hospital mortality.
Las complicaciones cardíacas por endocarditis infecciosa (EI) se presentan en casi 50% de los casos y pueden presentarse complicaciones generalizadas. El interés del estudio fue determinar las características de los pacientes hospitalizados con EI que presentaron complicaciones neurológicas agudas y factores asociados a mortalidad temprana.
MétodosRevisamos expedientes y estudios de imagen desde enero del 2004 hasta mayo del 2010 de todos los pacientes con EI y complicaciones neurológicas evaluadas con tomografía computarizada o resonancia magnética durante la primera semana después de la complicación. El estudio fue descriptivo y retrolectivo.
ResultadosDe 325 casos con EI, incluimos 35 (10.7%) [varones 19 (54%), media 44 años]. La cardiopatía subyacente más frecuente fue valvulopatía reumática (n=8, 22.8%). Veinte pacientes sobrevivieron (57.2%, grupo A) y 15 fallecieron (42.8%, grupo B) durante su hospitalización. La principal causa de muerte fue choque séptico (n=7, 20%). No hubo significado estadístico entre ambos grupos independientemente de presentación clínica, tamaño de vegetación, agente infeccioso o territorio vascular del ACV. La cantidad total de lesiones cerebrales fue mayor en el grupo B (3.1 vs. 1.6, p=0.005) y el edema cerebral moderado a grave fue más frecuente (p=0.09). Dieciséis pacientes (45.7%) (12 grupo A y 4 grupo B, p=0.05) fueron tratados con cirugía cardiaca. Sólo 2 pacientes tuvieron resultados favorables con tratamiento conservador (5.7%).
ConclusionesEn pacientes hospitalizados por EI complicada con ACVs, la cantidad de lesiones observadas en estudios de neuroimágen y el tratamiento conservador se asociaron a una mayor tasa de mortalidad intrahospitalaria.
Infectious endocarditis (IE) is an inflammatory disease of the endocardium that most frequently involves the cardiac valves, but it may also occur at chordae tendinae or mural endocardium.1 The reported in-hospital mortality is 16% (range 11–26%).2 The variability in clinical presentation of IE requires a diagnostic strategy that is both sensitive for disease detection and specific for its exclusion across all forms of the disease. At present, diagnosis of IE is based on the presence of modified Duke criteria.3
Cardiac complications in IE are frequent in 30–50% of the cases, but systemic complications may occur.4,5 According to some studies, up to 65% of embolic events involve the central nervous system. Neurologic complications not only include embolic events but also cerebral hemorrhage, cerebral abscess or cerebritis, acute encephalopathy, mycotic aneurisms, meningoencephalitis and aseptic purulent meningitis. These complications are associated with a greater mortality.6 Although not yet determined in clinical trials, but also in retrospective cohorts, traditional risk factors for embolization include the number of vegetations, their location and morphologic characteristics. In particular the size of the lesion, as well as the underlying microorganism and presence of antiphospholipid antibodies.7,8
The aim of the present study was to determine the characteristics of in-patients with IE who suffered acute neurologic complications and the factors associated with early mortality.
Materials and methodsFrom January 2004 to May 2010, we reviewed the clinical and imaging charts of all of the patients diagnosed with IE admitted to our institution, a cardiovascular referral and third care facility. We defined IE according to previously published modified Duke criteria.2 Inclusion criteria consisted of any patient with IE who coursed with a deficit suggesting a neurologic complication of IE and who was evaluated by Magnetic Resonance or Computed Tomography within the first week after the clinical presentation. Medical records were reviewed for patients’ demographics, clinical and neurologic presentation, cardiac status and history (including congenital heart disease), blood cultures, echocardiographic findings (systolic function, number, location and size of vegetations, and presence of abscesses or perforations) and treatment. The clinical course was recorded and overall mortality was used as the measure of major outcome. Patients were divided in two groups depending on the outcome (group A if survived, and group B if death occurred).
Imaging evaluation included Magnetic Resonance (1.5T Magnetom Avanto, Siemens, Erlangen, Germany). Intravenous contrast administration of gadolinium was used at discretion of the radiologist if no contraindication for its use was noted. The acquisition protocol included T1W, T2W, FLAIR and DWI but additional sequences were obtained if requested by the neuroradiologist. Images were retrolectively analyzed in an indicated workstation (Syngo Viewer, Leonardo, Siemens Medical Systems, Germany) by one neuroradiologist with 10 (JHC) years of experience and blinded to clinical information. Image analysis was obtained only for acute lesions and included their vascular territory, number and size of the lesions, associated brain edema and its mass effect, presence of aneurysms and intracranial hemorrhage or infarction with hemorrhagic transformation. In addition, we obtained the ARWMD scale (Age Related White Matter Disease)9 to rule-out presence of potentially confounding microvascular disease.
For the statistical analysis we used SPSS, version 17.0 (Chicago, Illinois). IRB approval was obtained but no patient consent was required due to the retrospective nature of the study. Parametric variables were evaluated with mean and standard deviation as a measurement of central tendency. Differences between qualitative variables were analyzed with the Chi-square test and t test was used for continuous variables. Statistical significance was considered when p value was <0.05.
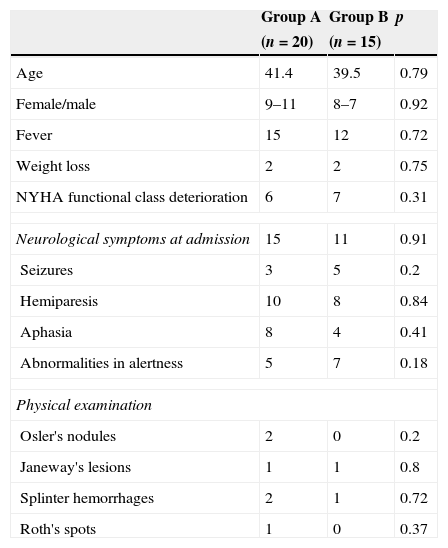
ResultsClinical and demographic dataAmong 325 cases identified with IE we included 35 patients (10.7%) [male 19 (54%), mean age 44 years (range 1–79 years)] with a documented cerebrovascular event. The most frequent symptom at admission was fever (n=27, 77%) followed by neurologic manifestations (n=26, 74%). However, during the hospital stay, almost all of the patients presented with a neurologic deficit, with the exception of one patient who developed papilledema and another one with amaurosis fugax. Seventeen patients presented hemiparesis (51.4%) while aphasia and progressive neurological impairment was noted in 12 cases (34.7%). The rest of the symptoms are shown in Table 1.
Patients’ demographics and clinical/neurological presentation.
| Group A | Group B | p | |
|---|---|---|---|
| (n=20) | (n=15) | ||
| Age | 41.4 | 39.5 | 0.79 |
| Female/male | 9–11 | 8–7 | 0.92 |
| Fever | 15 | 12 | 0.72 |
| Weight loss | 2 | 2 | 0.75 |
| NYHA functional class deterioration | 6 | 7 | 0.31 |
| Neurological symptoms at admission | 15 | 11 | 0.91 |
| Seizures | 3 | 5 | 0.2 |
| Hemiparesis | 10 | 8 | 0.84 |
| Aphasia | 8 | 4 | 0.41 |
| Abnormalities in alertness | 5 | 7 | 0.18 |
| Physical examination | |||
| Osler's nodules | 2 | 0 | 0.2 |
| Janeway's lesions | 1 | 1 | 0.8 |
| Splinter hemorrhages | 2 | 1 | 0.72 |
| Roth's spots | 1 | 0 | 0.37 |
Thirty-one patients (88.5%) had an underlying cardiac disease, but only in 19 cases (54.2%) this was previously known; arrhythmias were present in 10 (28.5%) patients. The most common underlying cardiac disease was rheumatic valvulopathy (n=8, 22.8%) followed by bicuspid aortic valve (n=7, 20%), complex congenital heart disease (n=4, 11.4%) and degenerative valve disease (n=2, 5.7%). In addition, 13 patients (37.1%) had a history of cardiac surgery, but only 3 were recent (less than 1 year, 1 in group A and 2 in group B), and of the total, 9 patients (25.7%) had a valve replacement. Fifteen patients (42.9%) had at least one comorbidity being hypertension (n=7, 17%) and type 2 diabetes (n=5, 14.3%) was the most frequently found.
Twenty patients (57.2%, group A) survived while the other 15 patients (42.8%, group B) died during hospitalization.
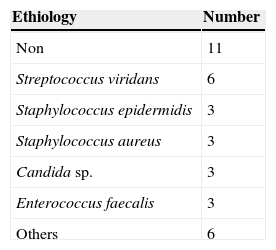
Microbiology and echocardiographic findingsThe etiologic agent was identified in 14 (71.4%) patients. The most prevalent microorganism was Streptococcus viridans (n=6, 17.1%). Only one patient had polymicrobial infection (Streptococcus. mitis and Escherichia coli) (Table 2). Nine patients (31.5%) received antibiotic therapy previous to the event. Nevertheless, only three had more than 2 weeks of treatment. No correlation was found between the type of microorganism and the use of previous antibiotic therapy (p=0.179) or mortality (p=0.689).
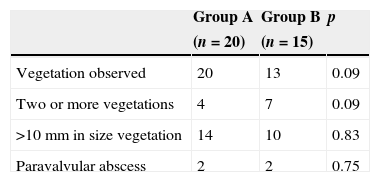
All patients had transthoracic echocardiography and in 23 patients transesophagic echocardiography was also obtained. Thirty-three patients (94.3%) had at least one vegetation identified by this method. More patients in group A had large vegetations (>10mm) when compared to group B. However, this difference was not statistically significant (14 vs. 10, p=0.83). There was a tendency of having two or more vegetations in group B (7 vs. 4, p=0.09). Vegetations were more frequently found in left valves (n=29, 87.9%) with a prevalence of mitral valve involvement of 57.6% (n=19), while in the aortic valve was 42.4% (n=14) (Table 3). Three patients (9%) had right-sided valve vegetations and only one patient with a patent foramen ovale. There was no difference in vegetation location between the groups (Table 2). Intracardiac abscess was diagnosed in 11.4% (n=4) of the patients without difference among the groups (2 vs. 2, p=0.75).
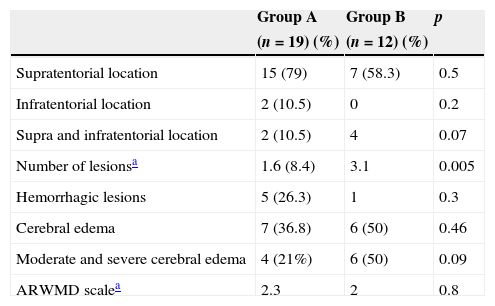
Neuroimaging findingsFour patients were excluded from the neuroimaging analysis because the quality of the scan was considered insufficient due to motion artifacts. In the remaining 31 cases, supratentorial lesions were more frequent (n=22, 71%; 15 in group A and 7 in group B, p=0.5), and infratentorial lesions were present only in 2 (6.5%). Both supra and infratentorial lesions were found in two (10.5%) and four (33%) patients in the group A and B, respectively (p=0.07).
The most frequently affected supratentorial vascular territory was the middle cerebral artery (MCA) in 83.8% (n=26), while superior cerebellar artery was the most frequently affected infratentorial territory (n=4, 12.9%). The overall number of lesions was significantly higher in group B (3.1 vs. 1.6, p=0.005). Hemorrhagic lesions were found in six (19.3%) patients, without difference between the groups (Table 4). The mean ARWMD scale was 2.3 and 2 in groups A and B, respectively (p=0.8). The most common possible etiology was thromboembolism in 79% (n=15) and 58.3% (n=7) of the cases in groups A and B, respectively. Brain edema was observed in nearly one-third of the cases in group A (n=7, 36.8%), while present in 50% of the cases in group B (n=6, p=0.46). Moderate and severe cerebral edema were more frequent among group B (6 and 4 cases, respectively, p=0.09).
Neuroimaging findings.
| Group A | Group B | p | |
|---|---|---|---|
| (n=19) (%) | (n=12) (%) | ||
| Supratentorial location | 15 (79) | 7 (58.3) | 0.5 |
| Infratentorial location | 2 (10.5) | 0 | 0.2 |
| Supra and infratentorial location | 2 (10.5) | 4 | 0.07 |
| Number of lesionsa | 1.6 (8.4) | 3.1 | 0.005 |
| Hemorrhagic lesions | 5 (26.3) | 1 | 0.3 |
| Cerebral edema | 7 (36.8) | 6 (50) | 0.46 |
| Moderate and severe cerebral edema | 4 (21%) | 6 (50) | 0.09 |
| ARWMD scalea | 2.3 | 2 | 0.8 |
During hospitalization 16 patients (45.7%) (12 in group A and 4 in group B, p=0.05) were treated with cardiac surgery. Only two patients (5.7%) had a favorable outcome with conservative treatment and surgery was not required. According to the clinical records, 17 patients (48.5%) had a surgical indication. Nevertheless, this was not performed due to one of the following contraindications: cardiac disease with elevated surgical risk (2 patients), septic or cardiogenic shock (4 patients), the neurological condition and complication itself (7 patients), liver disease (3 patients with Child-Pugh C) or transfer to another hospital (1 patient).
Septic shock, cardiogenic shock and cerebral herniation were the main causes of death in 20% (n=7), 11% (n=4) and 8% (n=3) of the patients, respectively. Fifteen patients (42.8%) died.
DiscussionIn this descriptive and retrolective study, we conducted an in-depth analysis of the in-hospital mortality of patients with IE and stroke considering clinical presentation, characteristics of the vegetation evaluated by echocardiography, underlying pathogen and neuroimaging findings. We found that mortality was associated with the number of lesions observed in imaging studies (p=0.005) and reduced in patients treated with cardiac surgery (p=0.05).
From the total of 325 cases with IE, 35 (10.7%) patients had a documented cerebrovascular event, which is different from the reported prevalence (22–65%).10,11 This could have been explained because prior studies included not only stroke as a neurological complication but also any type of neurologic disorder presented at the time that IE was diagnosed (i.e. meningitis, encephalitis, spinal abscesses, seizures and psychiatric disorders). In addition, we only included those patients with confirmed stroke by neuroimaging, excluding patients with a doubtful clinical presentation, postoperative stroke, transient ischemic attacks and silent events. The latter two according to a recent report, were not associated with a higher mortality in this group of patients. However, this prevalence was similar to the study of Anderson et al. (9.6%),10 who used similar inclusion criteria and excluded nearly one-fifth of the cases who were erroneously described as having had a stroke. This also may be explained because we only considered for analysis patients who met the criteria for definite IE. To determine the true incidence of brain injury in patients with IE, neuroimaging would have to be performed to every patient. It should also be mentioned the high mortality associated to stroke in patients with IE. In our series, 42.8% died which is similar to prior reports (range 35–52%).10
The most common underlying cardiac disease was rheumatic valvulopathy, a common disorder in many countries. Surprisingly, from the group of patients with congenital heart disease, the most frequent associated disorder was bicuspid aortic valve (20%) which in recent years has been considered a low risk factor for infectious endocarditis.13–15 According to these results, it might be appropriate to reconsider as adequate the use of antibiotic prophylaxis in this group of patients.16 However, further studies addressing this particular question are needed. The etiologic agent was identified in 71.4% of the patients. The most prevalent microorganism was S. viridans (16%), while previous reports describe S. aureus and C. albicans as the most frequent etiology.1,17 Nevertheless, no correlation was found between the type of microorganism, use of previous antibiotic therapy or mortality.
More than 90% of the cases had at least one vegetation seen by echocardiography. Vegetations on mitral valve were more prevalent than in the aortic valve, which is consistent with prior reports.10,12 The development of stroke is believed to be due to the larger vegetations in patients with mitral valve disease.7,12,18 However, we did not find a significant difference in size of the vegetation as a predictor of mortality in patients with stroke, but a tendency of having more vegetations was noted in the group who died (7 vs. 4, p=0.09).
Neuroimaging evaluation should include MR in those cases with normal or nearly normal CT scans, a common and well-known event in early phases of vascular brain lesion. The distribution and prevalence of the neurological complications was similar to previous reports, being supratentorial regions more affected and MCA territory the most frequent localization. We believe it might be relevant to mention the worst prognosis we found among those patients with both supra and infratentorial lesions with a tendency to have a statistical significance. Moderate to severe cerebral edema was more prevalent among patients in group B also with tendency to statistical significance. Nevertheless, the only variable associated to mortality was the number lesions observed. Hemorrhage and underlying white matter disease showed no difference between the two groups.
More than 40% of patients died, being septic shock and cerebral herniation the main causes of death in 31.4% and 8% of patients, respectively.10–12 As previously reported by Thuny et al., we also found that survival was better in patients treated surgically when compared to medical treatment. The main reason to delay surgery was the neurologic status itself. Therefore, it is difficult to determine the isolated effect of treatment or severity of the neurological complications due to collinearity.11 The impact of cardiac surgery (i.e. valve replacement) on outcome in patients with stroke in IE has been largely debated. There is a risk of postoperative neurologic exacerbation when surgery is performed early after the vascular event because hypotension and total heparinization during cardiopulmonary bypass. Nevertheless, according to recent reports12,19 this risk remains low. Even though further investigation with controlled studies are needed to make any recommendation in this regard, we believe that our study as well as previous reports, raise the possibility of modifying surgical indications in patients with IE and cerebral vascular events.10,11
There are some limitations in our study. The retrospective analysis may have limited the selection of patients because some individuals with mild signs or symptoms and with an atypical neurologic presentation may not have been included. In addition, we did not include patients with silent or transient ischemic events, which could have reduced the true prevalence of neurologic events in this group. Finally, this study may suffer from a referral bias because our institution represents a tertiary medical center for cardiac disease.
ConclusionsIn patients with IE complicated with clinically evident stroke, the number of lesions observed in neuroimaging examinations and a conservative treatment are associated with higher in-hospital mortality. Additional controlled trials are needed to definitely determine the safety period to perform surgery after a stroke complicating endocarditis.
FundingNo endorsement of any kind was received to conduct this article
Conflict of interestThe authors declare no conflict of interest.