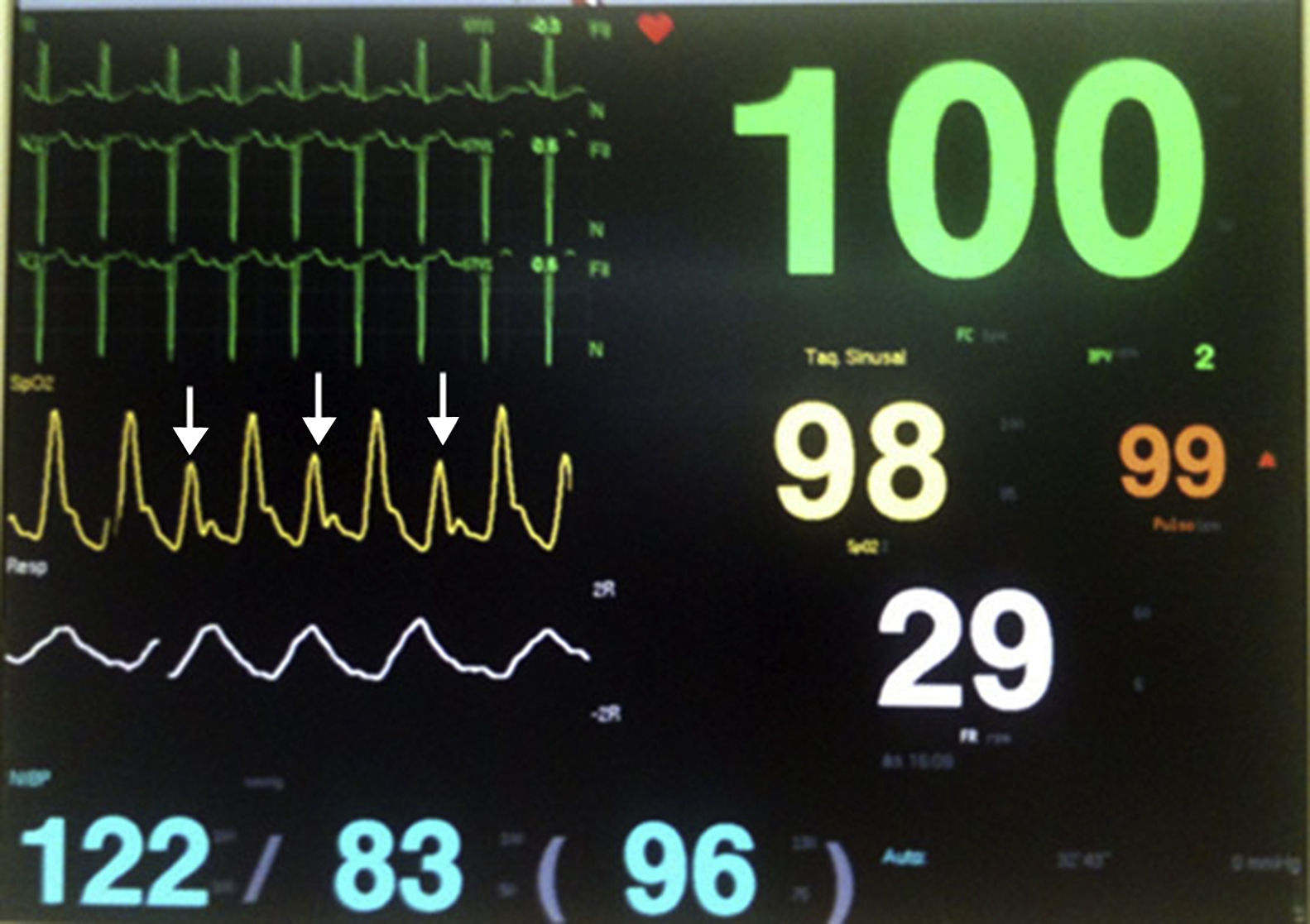
A 46-year-old man with idiopathic dilated cardiomyopathy was admitted to the intensive care unit because of acute decompensated heart failure. He complained of dyspnea at rest and peripheral edema, which was aggravated over the last week. His physical examination showed an elevated venous pressure, bilaterally reduced lung sounds at the pulmonary bases and symmetrical lower extremity edema. Despite the volume overload, his peripheral perfusion and blood pressure were normal, defining his hemodynamic profile as wet and warm. Continuous EKG monitoring confirmed the presence of normal sinus rhythm and his plethysmographic waveform obtained from the pulse oximeter revealed alternating wave amplitudes, suggesting pulsus alternans (Fig. 1, arrows). He was treated with intravenous diuretics and responded well to therapy over a few days.
Pulsus alternans is a sign of severe left ventricular failure, and is represented by alternating high and low systolic stroke volumes at every other cardiac cycle, which in turn affects the arterial pulse amplitudes in the same pattern.1 At the bedside setting, it can be detected by palpation, assessment of oximetry or arterial waveforms or even by sphymomanometry.2 Although it was first described in the nineteenth century by Traube, the exact pathophysiology remains obscure.1,3 Possible explanations include variations in intracellular calcium or diastolic volume, which could affect subsequent stroke volumes by Frank–Starling's mechanism.2