Introduction
Clopidogrel is a potent inhibitor of ADP induced platelet aggregation and is recommended to prevent both acute and late thrombotic complications after percutaneous coronary intervention (PCI). Patients pretreated with clopidogrel had fewer peri-procedural myocardial infarctions in PCI-CURE.1 However, without a loading dose, achieving optimal inhibition can take several days. A loading dose of 300mg, showed superior clinical outcomes in patients who were pretreated more than 6 hours before PCI and at a higher loading dose of 600mg, clopidogrel can be administered less than 6 hours before PCI.2-4 Based on this general agreement, the recent update of the ACC/ AHA PCI guidelines recommends a 600mg loading dose of clopidogrel before or during PCI.5 Nevertheless, despite the positive body of data, the clopidogrel loading dose is controversial, since it may increase coronary artery bypass graft (CABG) surgery related bleedings.6,7 Most of the bleedings occur if the CABG is performed within 3-5 days of clopidogrel loading.6,7 The ACC/AHA guidelines therefore recommend delaying the surgery for 5 or more days after clopidogrel exposure.8 However, concerns have been raised regarding adherence to these guidelines in practice. For example, a study of 264 hospitals found that almost 90% of patients who were pretreated with clopidogrel had CABG within 5 days of exposure.9 We sought to investigate the current single center experience regarding CABG surgery in patients pretreated with clopidogrel and its possible association to increased hemorrhagic complications and longer hospital stay.
Methods
Study population and design: After obtaining approval from the Institutional Review Board of the University of Oklahoma Health Sciences Center and the VA Research and Development committee, we reviewed charts of patients who underwent diagnostic heart catheterization between March 2007 and August 2007 at the Veterans Affairs (VA) Hospital, Oklahoma City, OK (n = 493), and identified all the patients who subsequently underwent CABG (n = 56). To include only patients after the index diagnostic catheterization, we excluded any patient with a prior CABG indication; therefore, one patient was excluded because he had concomitant aortic stenosis. Additionally, one patient was lost to follow up. The remaining (n = 54) patients were classified into two groups based on whether they received a clopidogrel pretreatment (clopidogrel group, n = 20) or not (no-clopidogrel group, n = 34). Clopidogrel pretreatment most commonly consisted of a 300 mg loading dose approximately 12-24 hrs prior to catheterization, or in some cases the patient already had been on a 75 mg daily dose.
Definitions and endpoints: The primary endpoints were incidence of major hemorrhagic complications and the median post-surgical hospital stay. Hemorrhagic events were measured using the Thrombolysis in Myocardial Infarction (TIMI) Bleeding Index [hemoglobin (Hgb) loss adjusted for any blood transfusion (preoperative Hgb - minimum post-transfusion Hgb + units of blood transfused)]. According to the TIMI bleeding definitions, major bleeding was defined as TIMI Bleeding Index greater than 5. We also used two alternative definitions - major hemoglobin loss, and major blood transfusion. Major hemoglobin loss was defined as peak hemoglobin loss greater than 5 g/dL (peak Hgb loss = preoperative Hgb - minimum postoperative Hgb), and major blood transfusion as more than 4 units transfused.
Statiscal analysis: Continuous variables are expressed as mean ± standard deviation (SD). Dichotomous variables are shown as percentages. Comparison between continuous variables was done using Student's t test if normally distributed and Wilcoxon rank-sum if not. One-sample Kolmogorov-Smirnov test was used to test for normality, with p < 0.1 as an indication of non-normal distribution. Medians with 25th and 75th percentile are used to express such variables. Categorical variables were compared using chi-square with normal approximation, chi-square test for trend when categories were ordered, or Fisher's exact test when appropriate. Linear (TIMI Bleeding Index, peak hemoglobin loss, and length of stay), exact logistic (TIMI Bleeding Index > 5, hemoglobin loss > 5 g/dL, blood transfusion > 4 units, any blood transfusion), or cumulative logistic (blood transfusion units categorized at tertiles) regression models were fit to adjust the clopidogrel versus no-clopidogrel group comparison for confounding baseline characteristics. Length of hospital stay was transformed using the natural log to better satisfy linear model assumptions. Given the limited complication rates, clopidogrel was fit as an independent term with adjustment for each individual baseline characteristic that was significantly associated with the log odds of each categorical response at the 0.1 alpha level to identify confounding factors for the logistic models. Linear regression models included clopidogrel treatment as an independent factor along with all baseline characteristics that were significantly associated with the mean continuous response at the 0.1 alpha level and the model was reduced by dropping non-significant baseline confounding factors relative to an alpha level of 0.05. Regression coefficient estimates from unadjusted and adjusted models are reported. All p-values for statistical tests are 2-tailed with p < 0.05 considered significant.
Results
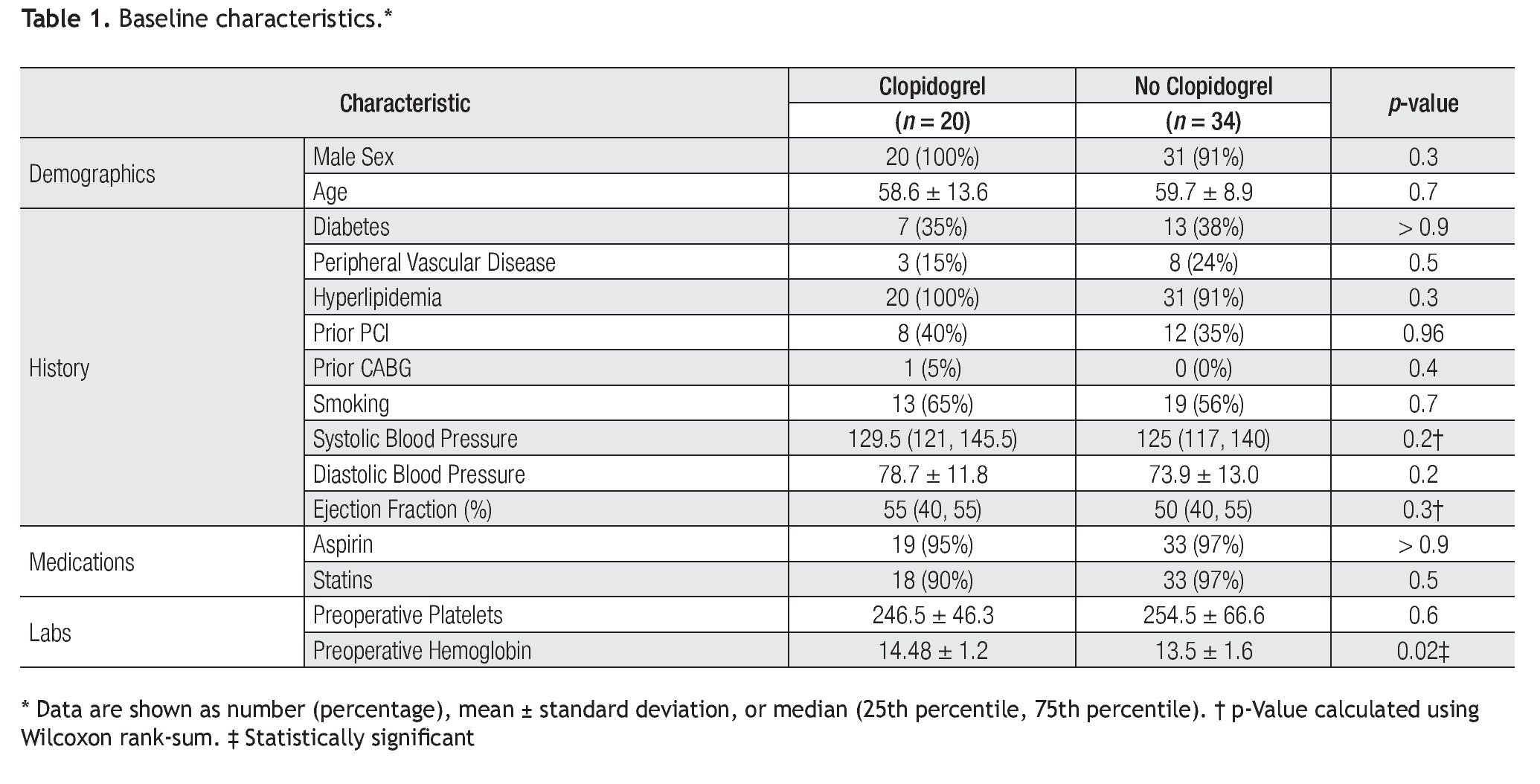
Baseline characteristics of patients: In the clopidogrel and no-clopidogrel groups are shown in Table 1. All characteristics were well matched between the two groups, except pre-surgical hemoglobin which was higher in the clopidogrel group (p = 0.02). Patients were predominantly male with mean age of approximately 59 years. Most of them had hyperlipidemia, and 35-40% had prior PCI.
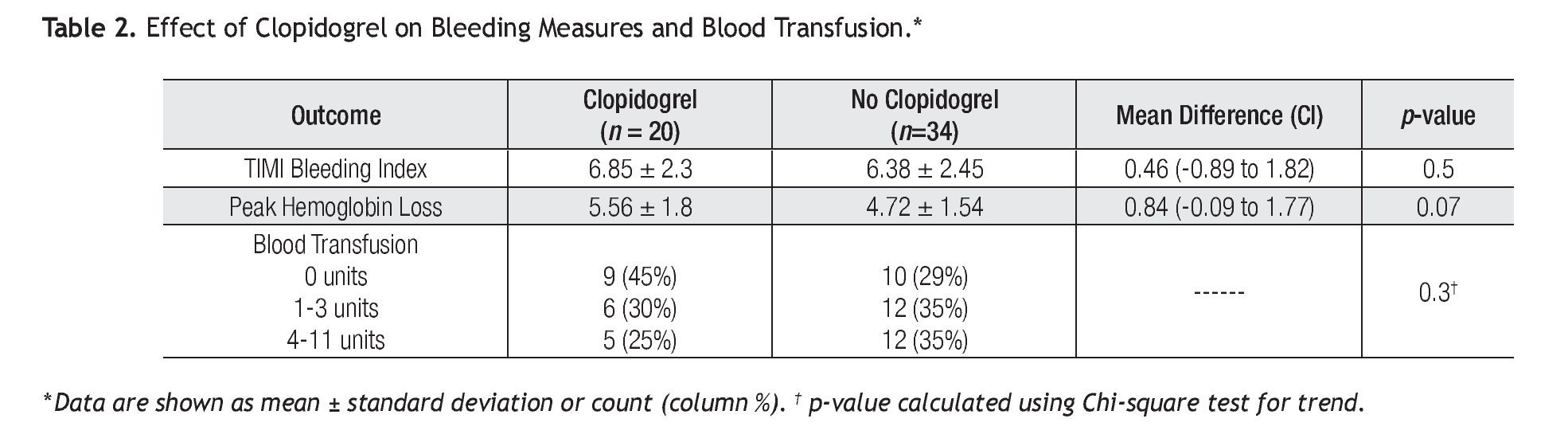
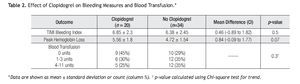
Bleeding: The data for bleeding measures, including blood transfusion, is summarized in Table 2. The mean peak hemoglobin loss had a tendency to be increased in the clopidogrel group (5.56 g/dL vs. 4.72 g/dL) (mean difference 0.84; 95% CI -0.09 to 1.77; p = 0.07). However, after adjusting for preoperative hemoglobin, the association between clopidogrel pretreatment and peak hemoglobin loss was diminished (unadjusted model coefficient: â = 0.84, p = 0.07; adjusted model coefficient: â = -0.03, p = 0.9). The TIMI Bleeding Index in the clopidogrel group was 6.85 vs. 6.38 in the no-clopidogrel group (mean difference 0.46; 95% CI -0.89 to 1.82; p = 0.5), while there was no significant difference in the distribution of the number of units of blood transfused in the clopidogrel group (p = 0.3). These conclusions did not differ after adjustment for potential confounding baseline characteristics.
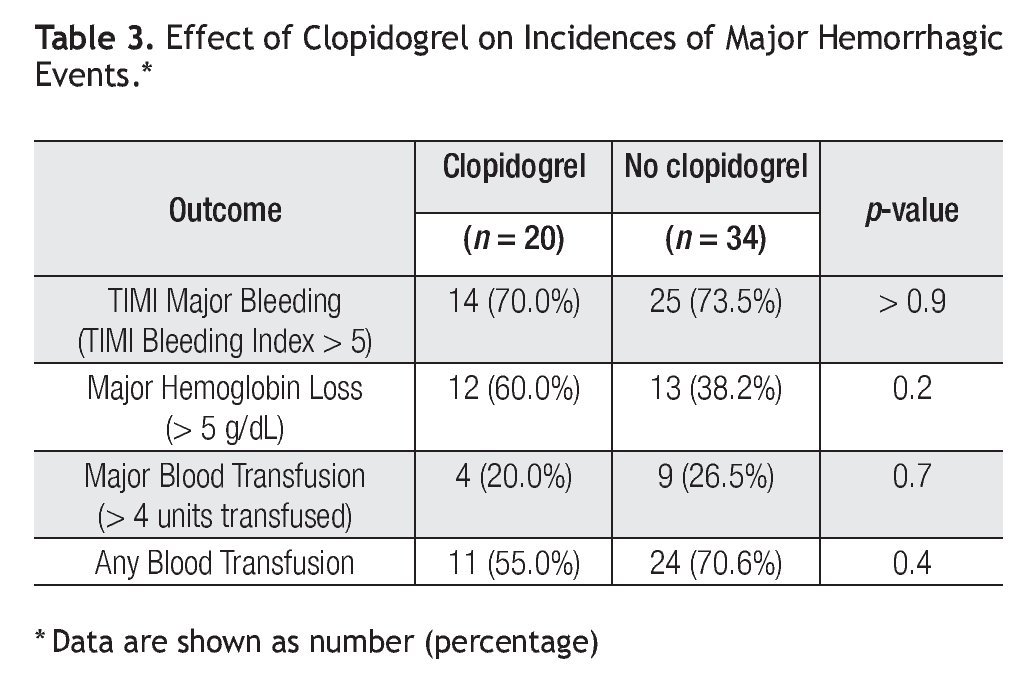
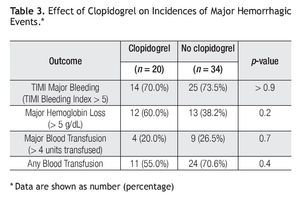
The incidences for major hemorrhagic events are shown in Table 3. Clopidogrel group had a tendency for higher incidence of major (> 5 g/dL) hemoglobin loss (60.0% vs. 38.2%; p = 0.2); interestingly, any blood trans-fusion was higher in the no-clopidogrel group, although not statistically higher (55.0% vs. 70.6%; p = 0.4). The incidence of TIMI Major Bleeding, which accounts for both hemoglobin loss and blood transfusion, was very similar in both groups (70.0% vs. 73.5%; p > 0.9). These conclusions did not differ after adjustment for potential confounding baseline characteristics.
Post-surgical hospital stay: The post-surgical hospital stay was found to be shorter in the clopidogrel group, a median of 5 days (25th, 75th percentile: 4, 6 days), compared to the no-clopidogrel group, a median of 7 days (25th, 75th percentile: 5.8, 8.3 days). Based on an unadjusted regression model, the median length of stay is 32% shorter for subjects receiving clopidogrel compared to those who did not (p = 0.03). The post-surgical hospital stay was found to be shorter in the clopidogrel group, a median of 5 days (25th, 75th percentile: 4, 6 days), compared to the no-clopidogrel group, a median of 7 days (25th, 75th percentile: 5.8, 8.3 days). Based on an unadjusted regression model, the median length of stay is 32% shorter for subjects receiving clopidogrel compared to those who did not (p = 0.03). Since it is possible that this difference in length of hospitalization is driven by sicker patients with lower ejection fractions or more blood transfusions, we decided to apply a regression model to adjust for these characteristics; we estimate that the median length of stay is 23% shorter for subjects receiving clopidogrel compared to those who did not (p = 0.07). One subject in the no-clopidogrel group had a length of stay that was very extreme (187 days). When this subject was deleted from the regression models, the estimated reduction in the median length of stay for clopidogrel versus no-clopidogrel patients was 24% (p = 0.01) for the unadjusted model and 20% for the adjusted model (p = 0.02).
Delay between last clopidogrel dose and surgery: The median number of days from diagnostic heart catheterization to CABG in the clopidogrel group was 19 (25th, 75th percentile: 9.5, 46.25 days), compared to 7 days (25th, 75th percentile: 3.75, 29.25 days) in the no-clopidogrel group, with p = 0.02. Though reasons for scheduling of CABG surgeries on specific dates were not available, the data does point to a trend towards delaying the surgery by five or more days in patients pre-treated with clopidogrel, with only one surgery within five days.
Discussion
Several studies have reported increased bleeding with clopidogrel when CABG was done within 3-5 days of loading.6,7 Delaying the surgery by 5 or more days after clopidogrel pre-treatment has been recommended by the guidelines to mitigate this effect.8 Though a study expressed concerns regarding adherence to these guidelines, reporting that almost 90% of surgeries were conducted within 5 days,9 our data suggests that the practice at VA is in accordance with the guidelines. The similar rates of bleeding between clopidogrel and no-clopidogrel treatment groups supports the current guidelines of delaying surgery for at least 5 days. The importance of following the guidelines is further emphasized with the observance of a trend of increased bleeding in the early CABG subgroup with clopidogrel pre-treatment.
We also observed that the patients in no-clopidogrel group were staying longer in the hospital postoperatively. Additionally, these patients also needed slightly more blood transfusion compared to those who were pre-treated with clopidogrel. While the precise reasons for this observation are not clear, we suspect, given subtle differences in the baseline characteristics, there might have been an overall sicker population in the no-clopidogrel group. One significant difference in the baseline characteristics was that the no-clopidogrel group had lower preoperative hemoglobin (Table 1). Several studies have identified low preoperative hemoglobin as a significant predictor of need for blood transfusion during both cardiac10-12 and non-cardiac13-15 surgeries, and could possibly explain our observation. Nonetheless, our study does show that delaying CABG for 7 or more days after clopidogrel loading downgrades clopidogrel exposure to a much lower level in the list of surgical risk items.
The retrospective observational nature of our study is one of the main limiting factors. We are unable to rule out all potential confounding factors that may have been related to clopidogrel pretreatment. Additionally, this study is limited by the small number of observations (n = 20 in clopidogrel group, n = 34 in no-clopidogrel group).
Conclusions
The results of our study suggest that the current practice of loading patients with clopidogrel before PCI does not significantly increase the risk of hemorrhagic complications provided the surgery is delayed for at least 7 days if the patient turns out to be a candidate for CABG instead of PCI.
Authors' contributions
SR, PL, and JEE conceived and designed the study. SR collected the data; SR, JEE, and LMB performed statistical analysis; SR, PL, JEE, and LMB contributed to data interpretation. SR drafted the manuscript which was revised by JEE, PL, and LMB. All authors read and approved the final manuscript.
Acknowledgements
We would like to thank Dr. Angelia C Kirkpatrick, MD for reviewing the manuscript and Dr. Julie Stoner, PhD for help with statistical analysis.
Corresponding author: J. Emilio Exaire,
920 S.L. Young Boulevard, WP# 3010. Oklahoma City, OK - 73190, USA.
Phone: (405) 271-4742 Fax: (405) 271-2619.
E-mail:Jose-Exaire@ouhsc.edu
Received: December 18, 2008;
accepted: 2 June, 2010.