RENASICA III is a prospective, multicenter registry on acute coronary syndromes (ACS). The main objective will be to identify the outcome in tertiary and community hospitals and perform strategies to improve quality of care in Mexico.
MethodsRENASICA III will enroll 8000 patients in public health and private hospitals. The registry began in November 2012 with a planned recruitment during 12 months and a 1-year follow-up. The study population will comprise a consecutive, prospective cohort of patients >18 years with ACS final diagnosis and evidence of ischemic heart disease. The structure, data collection and data analysis will be based on quality current recommendations for registries. The protocol has been approved by institutional ethics committees in all participant centers. All patients will sign an informed consent form.
Currently in Mexico, there is a need of observational registries that include patients with treatment in the everyday clinical practice so the data could be validated and additional information could be obtained versus the one from the clinical trials. In this way, RENASICA III emerges as a link among randomized clinical trials developed by experts and previous Mexican experience.
RENASICA III es un registro prospectivo multicéntrico en síndromes coronarios agudos (SCA). El principal objetivo será identificar en México la evolución en hospitales de segundo y tercer nivel para establecer estrategias para mejorar la calidad de la atención.
MétodosRENASICA III ingresará 8000 pacientes en hospitales de instituciones de salud y privados. El registro inició en noviembre de 2012 con un reclutamiento durante 12 meses y un seguimiento al alta hospitalaria de 12 meses. La población en estudio incluirá una cohorte prospectiva de pacientes >18 años con diagnóstico final de un SCA y evidencia objetiva de cardiopatía isquémica. La estructura del registro, la recolección de datos y el análisis se basó en las recomendaciones actuales para la calidad de los registros en enfermedad cardiovascular. El protocolo fue aprobado por los comités institucionales de ética de todos los centros participantes. Todos los pacientes firmarán un consentimiento informado.
En la actualidad existe en México la necesidad de registros observacionales que incluyan pacientes sometidos a tratamiento en la práctica clínica contemporánea para validar los datos y obtener información complementaria de los grandes estudios aleatorizados controlados. RENASICA III emerge como un vínculo entre estudios aleatorizados controlados conducidos por expertos y la experiencia mexicana previa.
In the last decades, ischemic heart disease and acute coronary syndromes (ACS) remain part of chronic degenerative diseases. In developed and less developed countries they could be seen also as an expression of demographic and epidemiological transition with a deep impact in terms of mortality, quality of life and resource use. In countries with strong economies and capacities, mortality reduction has been achieved through changes in socioeconomic status, risk factors control, effective treatments and resources that translate clinical studies results into clinical practice. Recent evidences from GRACE and CRUSADE registries show that guidelines compliance improves the outcome of ACS patients.1
In Mexico, the first national registry of acute coronary syndromes2 (RENASICA I) identified epidemiologic characteristics, therapeutic trends and risk stratification. Through the second national registry (RENASICA II3), RENASCA4 and ACCESS5 registries, previous observations were confirmed and better therapeutic approaches and high-risk groups were identified.6,7 A substudy of RENASICA II8 showed similar antithrombotic treatment compliance compared with CRUSADE in non-ST elevation ACS patients. As an interesting observation, no difference in mortality among Mexicans (4%), Hispanics (4%) and White (5%) patients was observed.
Considering previous evidences in Mexico,3–8 time reduction between onset of symptoms and first hospital contact (>3.5h), increased pharmacological (<35%) and mechanical (<10%) reperfusion and more patients under fibrino-specific lytic agents and better anticoagulation is a challenge. However, in spite of long ischemia times and low access to reperfusion approaches, in-hospital mortality (10%,3 8%,4 2%5) remains low probably due to an underestimation of the total deaths in our tertiary centers and lack of follow-up at discharge; as a consequence of all this process ventricular dysfunction (17%,3 39%4 and 30%5) was the most frequent in-hospital complication. Similar results have been observed in developed countries.5 RENASICA III intends to identify a high-risk stratification, diagnosis and treatment approaches in community and tertiary hospitals to optimize resources and to define strategies to improve quality of health care.
MethodsRegistry designRENASICA III is a prospective, multicenter registry on ACS male and female patients. The project is an initiative of the Mexican Cardiology Society supported by Sanofi and it was designed to obtain a sample free of trends with statistical impact. The main objective will be to identify outcome in tertiary and community hospitals and perform strategies to improve quality of care. The registry is planned to enroll 8000 patients from public health and private hospitals.
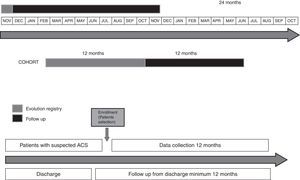
The registry began in November 2012 with a planned recruitment during 12 months and 1-year follow-up (Figure 1). The protocol has been approved by institutional ethics committees in all participant centers. The registry will be conducted in accordance with the Declaration of Helsinki, International Conference on Harmonization-Pharmaco-Epidemiology and Good Clinical Practices. National requirements coming from COFEPRIS will be considered as well. As an observational registry, no specific treatments, tests, or procedures will be mandated or withheld from the patients; participants will be free to withdraw from the registry at any time. All patients will sign an informed consent.
Study populationThe study population will comprise a consecutive, prospective cohort of patients >18 years with ACS final diagnosis and objective evidence of ischemic heart disease. Patients admitted to emergency departments, coronary care units, intensive care units, hospital and hemodynamic laboratories with high clinical suspicion and subsequently proven diagnosis will be eligible. The initial diagnosis will be established by physician in charge based on clinical and electrocardiographic findings in all cases. The structure, data collection and data analysis were based on current quality recommendations for registries.9 ACS nomenclature will be standardized at admission and for epidemiologic reasons unstable angina or infarction at discharge. Principal investigators will be selected in community and tertiary hospitals with a geographical distribution covering the entire country (Figure 2).
ObjectivesPrimary: To identify clinical diagnostic and therapeutic characteristics in Mexico. Secondary: (a) to assess adherence to guidelines for diagnosis and treatment of ACS; (b) to identify issues and establish health system strategies to improve patient care; (c) to identify standards of acute and in-hospital patient care in participating centers; (d) to propose therapeutic approaches according to available resources and technology; (e) establish accessible risk stratification in ACS through mortality predictive variables observed in RENASICA II.3
Patient screeningAll patients with high-clinical suspicion of ACS will be included through risk factors, chest pain symptoms and ECG findings. At the beginning four groups will be considered based on ST segment electrocardiographic findings: normal or unspecific ECG, ST depression, transient ST elevation,10 or persistent ST elevation. At discharge objective evidence of ischemia by invasive or noninvasive testing must be proved. Patients with secondary ischemia (anemia, pulmonary embolism, myocarditis, and etcetera) and type II infarction will not be included.
Quality criteriaThe following criteria will be used to improve quality data: (a) standardized definitions, data and reports; (b) tools for immediate feedback; (c) meetings among the scientific and executive committee; (d) ethics procedures review; e) electronic, simple and accessible data collection; (f) randomized centers selection; (g) consecutive patients enrollment to obtain representative sample; (h) random centers audit; (i) centralized data and statistical analysis; (j) report all data and consistent conclusion; and (k) transparency of funds for any publication.9 Furthermore, the quality of this registry will also be measured by the number of publications and presentations in national and international meetings as previously done.11
Follow-upClinical adverse events, therapeutic approaches and revascularization procedures will be included (Figure 1). The standardized definitions can be explored in Appendix A.
Data collectionData will be sent to the registry coordinating center through a web site addressed at http://www.renasica.mx/. All patients will have a unique personal identification to ensure their anonymity. A simple format to facilitate data entry using the most relevant variables of previous registries will be used.3,4 Electronic case report forms will be reviewed by the coordinating center to determine data quality and to generate queries that will be sent to each center. All participating institutions will have regular access to a data entry clerk; to ensure data quality, monitoring will be randomly made in 20% of the centers.
Technical supportOngoing programs to update, maintain, and improve the electronic database have been established. Every center will have a timely provision of case report forms. Training meetings will be scheduled for electronic database and definitions. The coordinating center will have a 01–800 number to provide technical advice online. Monthly newsletters with statistical reports of the main variables will be coordinated by the executive committee. Follow-up by telephone contact visit will be achieved through coordinating center. In specific cases, follow-up will be made by the physician in charge. Monthly cleaning database will be scheduled for a correct and expeditious final analysis. The system has searching tools by criteria and generates reports plotted in real time.
Training strategies to improve careThe executive and scientific committees will coordinate workshops to standardize care process in first contact area patients.
Publications policiesExecutive committee established appropriate guidelines to allow all investigators an expedited process for publication or presentation at national and international meetings following the appropriate channels.
Sample size determinationRisk stratification in ACS patients has shown high prediction of major cardiovascular events. According to the findings of RENASCA4 50% of patients do not receive adequate treatment, and only 8% of patients have percutaneous coronary intervention (PCI), leading to 30% of left ventricular failure as a complication. In RENASICA II3 only 15% of patients received PCI and 17% had left ventricular failure as a complication. This difference will allow us to calculate the smaller sample size for this outcome: statistical power 80%, alpha value 0.05, delta value 13%, relationship between exposed and unexposed 1:1, confidence interval (CI) 95%. It will require 182 patients per group, plus 20% loss yields 220 patients per group. Lower delta value for mortality of 2% requires 3975 patients treated and not treated with PCI. This implies that the registry requires 8000 subjects to be included.
StatisticsDifferences between continuous variables with normal distribution will be examined by Student's t test. The test of Wilcoxon rank sum will be used when continuous variables have failed in normality tests. To analyze categorical variables X2 will be used by Fisher's exact test or Yates correction. A two-tailed test with a p value ≤0.05 will be considered as statistically significant. Logistic regression analysis will be used to select independent predictors in those variables that by univariate regression analysis had obtained a p≤0.05. To avoid confusion, through logistic regression the relationship between historical variables for atherosclerosis and cardiovascular events will be examined. With the Cox proportional risk multivariate model will assess the relationship between each of these variables. Kaplan–Meier survival curves to cumulative survival curves for the risk of mortality and differences between the curves for significance by the log-rank statistic. The Cox proportional risk model will be used for adjusted survival analysis. A p value ≤0.05 will be considered as statistically significant. Data will be expressed as percentages, mean, standard deviation, odds ratio and confidence interval (CI) 95%.
ConsiderationsIn Mexico, ischemic heart disease is being the leading cause of death in the elderly and second in the general population. In 2011, ischemic heart disease was responsible for 71,072 deaths, accounting for approximately 11% of all deaths in Mexico.7 The RENASICA III registry will describe the management and clinical outcomes of a cross section of patients with a broad clinical spectrum of ACS in real-life practice. Data will be collected from newly diagnosed patients with ACS irrespective of whether they were receiving any reperfusion approach and will offer insights into outcomes of non-reperfused patients. Considering previous evidence from RENASICA II,3,8 RENASCA4 and ACCESS,5 we are able to know the epidemiologic characteristics, therapeutic trends and risk stratification in the last decade. Currently, it is important to identify if more invasive and pharmacologic reperfusion are used in STMI and compliance guidelines in terms of anticoagulation and antithrombotic treatment. Additionally, it will be interesting to know the role of new antiplatelet agents (prasugrel and ticagrelor) in the setting of ACS. In the transition of therapeutic approaches of ACS, through RENASICA III several questions will be answered: will non-specific fibrinolytic drugs be used in the majority of ST-elevation myocardial infarction? Or unfractionated heparin is the anticoagulant choice?
RENASICA III will show if invasive and pharmacologic reperfusion, anticoagulation and antithrombotic treatment have been improved in ACS patients. In randomized controlled clinical trials of ACS, regulatory authorities mandate very close or strict control of inclusion and exclusion criteria and will be conducted by an expert. This strategy will result in lower rates of in-hospital mortality and bleeding complications than those usually observed in real-life clinical practice. Thus, accurate assessment of reperfusion and antithrombotic approaches is more difficult to reach. Currently, there is, therefore, a need for a national observational registry of patients treated in everyday clinical practice to test the external validity of the trial data and provide complementary information to that from the trials.11 RENASICA III emerges as a link among randomized controlled trials conducted by experts and previous Mexican experience.2–8
Chest pain with ischemic profile: chest tightness or anterior chest at rest or exercise radiating to the neck, left arm, or both during >1min with or without adrenergic manifestations.
Chest pain with non-typical ischemic profile: does not meet the criteria of pain with ischemic profile, however suggesting myocardial ischemia as tightness in lower jaw, anterior neck, epigastrium, etc.
Previous angina: chest pain with ischemic profile, characteristic or not, or equivalent prior to current index event.
Equivalent of ischemia: this kind of ischemia clinical expression has different age-related variations. Ventricular arrhythmias, first event of heart failure without a clear etiology, sudden pulmonary edema, dyspnea at rest or exercise, syncope, mental confusion, asthenia, adynamia, anorexia associated with objective evidence of ischemia, micro, macronecrosis or both (Appendix B).12
Nonspecific: ST depression <0.05mV or negative asymmetrical T wave <0.2mV, ventricular hypertrophy, pacemaker rhythm.13–15
ST depression: depression >0.05mV in two underlying leads or negative symmetrical T wave >0.2mV.13,16
Transient ST elevation: J point positive slope (>0.2mV in V1–V3 and >0.1mV in other leads) in two underlying leads with ST normalization or residual negative deep T wave, spontaneously or secondary therapeutic action.13,16
Persistent ST elevation: positive slope at J point (>0.2mV in V1–V3 and >0.1mV in other leads) in two underlying leads.13,16
According to the Mexican electrocardiography school in the context of a left bundle branch block bundle the presence of Q wave in DI, aVL, V5 or V6 leads this suggests a septal infarction; loss of QRS voltage with Q wave in V4, V5 and V6 may correspond to an anteroseptal infarction. The presence of RS or rs with negative T wave (intracavitary lead) in V4–V6 could translate a left ventricular transmural infarction. In Appendix C criteria of Sodi Pallares and Sgarbossa can be observed.14,15
J point moving in the opposite direction to the predominant QRS deflection (negative in the presence of R wave, positive in the presence of S wave) with a magnitude of displacement up to 5mm is required. The ST and T wave will show the same polarity, behaving as a single pathophysiological entity. A ST elevation in an acute myocardial infarction associated with this conduction disturbance is divided into concordant and discordant. ST elevation ≥0.1mV (1mm) in leads with R wave or ST negative slope ≥0.1mV in leads V1–V3 (with dominant S wave) is called concordant. ST elevation 0.5mV (5mm) in leads with S wave is called discordant.15
- a)
Normal or nonspecific
- b)
Negative ST depression
- c)
Transient ST elevation
- d)
Persistent ST elevation
- a)
History of chest pain or discomfort with ischemic profile or not, ≥20min.
- a.
Equivalent associated with persistent ST elevation and abnormal biomarkers.
- b)
ECG with persistent ST elevation >1mm in at least two underlying leads or left bundle branch block or tall R wave (40ms) in V1 and V2 leads associated with ST depression V1–V3 and right leads.
- c)
Elevation of cardiac biomarkers serum levels (preferably troponin) with at least one value above the upper reference limit of 99th percentile.
- d)
Two-dimensional echocardiogram demonstrating new or presumably new abnormality of regional or global mobility.
Ischemia evidence: Demonstration and objective documentation of myocardial ischemia by echocardiography or nuclear medicine.13,16
Uncomplicated: normal blood pressure without left ventricular dysfunction signs, EF >40%, brain natriuretic peptide type-B (BNP) <100pg/dL, or both.
Complicated with left ventricular dysfunction without clinical manifestations: normal blood pressure or lower limits, no third left ventricular heart sound, EF <40%, or both, BNP >100pg/dL, or both.
Complicated with ventricular dysfunction with clinical manifestations: acute pulmonary edema or pre-cardiogenic shock suspicion (borderline blood pressure, hypotension, or both, clinical expression of -renin-angiotensin-aldosterone-vasopressin system activity, oliguria, delayed capillary refill, lower lobes crackling rales, EF <30%, BNP >600pg/dL.
I: without left ventricular dysfunction signs
II: left ventricular third heart sound, basal crackling rales, or both
III: acute pulmonary edema
IV: cardiogenic shock
Pulmonary edema: increased work of breathing with or without severe desaturation (saturation <90%), left ventricular gallop or tachycardia, crackling rales or wheezes >50% in lung fields. Chest X-ray with interstitial, alveolar, or mixed pulmonary edema.
Cardiogenic shock: (1) systolic blood pressure <90mmHg without support of vasoactive substances or 100mmHg with vasopressors use; (2) clinical, radiographic expression of pulmonary venocapillary hypertension, or both; (3) signs of peripheral vascular hypoperfusion; (4) metabolic acidosis; (5) cardiac index <2.2L/min/m2; (6) pulmonary capillary pressure >18mmHg; and (7) arteriovenous oxygen difference >5.5ml/dL.
Variables predictors of poor in-hospital outcome according to odds ratio (OR) and confidence intervals (CI) were selected from RENASICA II3 multivariate analysis: diabetes (OR 3.1, CI 1.94–5.06, and p<0.0001); ischemic chest pain >20min (OR 2.3, CI 1.43–3.69, and p 0.0006); heart failure history (OR 2.2, CI 1.16–4.23, and p 0.01); age >65 years old (OR 1.8, CI 1.27–2.67, and p 0.001); positive troponin (OR 1.7, CI 1.05–0.97, and p 0.02); and ST depression >3 leads (OR 1.6, CI 1.08–2.61, and p 0.02).
Electrocardiographic: ST decreased >70% in the most meaningful leads in an ECG taken 90min after pharmacological fibrinolysis the fibrinolytic regarding index event ECG.13
Major bleeding: Fatal bleeding, documented retroperitoneal, intracranial, or intraocular bleeding, bleeding resulting in hemodynamic compromise requiring specific treatment, bleeding requiring surgical intervention or decompression of a closed space to control the event, any transfusion >1 unit red packed cells or whole blood or a hemoglobin drop >3g/dL or more or hematocrit >10%.17
Minor bleeding: microscopic hematuria not associated with trauma by ureteral procedures. Prolonged or recurrent epistaxis requires plugging or intervention; gastrointestinal or subconjunctival bleeding or hemoptysis. Hematoma >5cm related with length in-hospital stay or new hospitalization. Bleeding decreasing hemoglobin drop <3g/dL or considering duration requires protamine sulfate.17
Fibrinolysis inducing hypotension: Blood pressure ≤90/60mmHg during or at the end of the fibrinolytic infusion without other apparent reason.
Primary angioplasty: with or without stent; without prior or concomitant fibrinolytic therapy or glycoprotein IIb/IIIa use.13
Rescue angioplasty: coronary intervention in patients after unsuccessful fibrinolytic therapy (persistent chest pain, ST elevation or decrease <70%, or both on an ECG at 90min).
Residual lesion: ≤30% and epicardial TIMI flow 3.
Suboptimal: Residual lesion: >30% and epicardial TIMI flow 2.
Failed: obstructive residual lesion ≥70% and TIMI flow 0–2 or when the guide wire fails through the atherosclerotic lesion.13
TIMI 0: total absence of flow
TIMI 1: slight penetration of the contrast medium without reaching the obstructive lesion or the terminal portion of the vessel
TIMI 2: penetration of the contrast medium reaches the obstructive lesion but not exceeded or the entire artery and typically presents with low flow
TIMI 3: normal coronary flow.13
TIMI 0: total absence of flow
TIMI 1: slight penetration of the contrast medium without reaching the obstructive lesion or the terminal portion of the vessel
TIMI 2: penetration of the contrast medium reaches the obstructive lesion but not exceeded or the entire artery and typically presents with low flow
TIMI 3: normal coronary flow.13
TMPG 0: No or minimal blush
TMPG 1: Stain present. Blush persists on next injection
TMPG 2: Dye strongly persistent at end of washout. Gone by next injection
TMPG 3: Normal ground glass appearance of blush. Dye mildly persistent at end of washout.18
TMPG 0: No or minimal blush
TMPG 1: Stain present. Blush persists on next injection
TMPG 2: Dye strongly persistent at end of washout. Gone by next injection
TMPG 3: Normal ground glass appearance of blush. Dye mildly persistent at end of washout.18
Recurrent ischemia: new chest pain episode with ischemic profile (treatment with two antiischemic drugs at least) >5min, with ST dynamic ECG changes, and without myocardial necrosis.
Reinfarction: Two or more of the following criteria: (1) chest pain with ischemic profile ≥20min; (2) new ST elevation (>0.1mV) in two underlying leads or new Q wave; (3) CK–MB new elevation ≥50% normal high upper limit or ≥50% of baseline.
Cardiogenic shock: (1) systolic blood pressure <90mmHg without support of vasoactive substances, or 100mmHg with vasopressors; (2) clinical, chest X-ray expression of pulmonary venocapillary hypertension, or both; (3) signs of peripheral vascular hypoperfusion manifested by oligoanuria <1ml/kg/h; (4) metabolic acidosis; (5) cardiac index <2.2L/min/m2; (6) pulmonary capillary pressure >18mmHg; and (7) arteriovenous oxygen difference >5.5ml/dL.
Cardiovascular death: Secondary to acute coronary ischemic event index or new in-hospital event or during follow-up.
Acute cerebrovascular disease: Loss of neurological function secondary to an ischemic, embolic or bleeding event. Ideally, objective evidence through computerized axial tomography or magnetic resonance must be obtained.
Ventricular fibrillation: Chaotic rhythm with total absence of isoelectric line and total absence of atrial contraction.
Ventricular tachycardia: Four or more consecutive ventricular extrasystoles; is considered as not sustained <30s or sustained >30s.
Hyperlipidemia: Cholesterol >200mg/dL or normal levels with treatment.
Previous infarction: Necrosis demonstration by ECG, echocardiography, nuclear medicine or nuclear magnetic resonance.
Mitral insufficiency: Regurgitation murmur radiating to the axilla and objective demonstration by echocardiography and ventriculography.
Renal failure: Serum creatinine >2.0mg/dL.
Renal dysfunction
Moderate: 50–30mL/min
Severe: <30mL/min
Cocroft Gault formula
Serum creatinine clearance=(140−Age expressed in years)×(Weight expressed in kilograms)
Serum creatinine (mg/dL)×72
Cardiac arrest: Electromechanical or asystole dissociation.
Pericarditis: Suggestive chest pain with or without pericardial rub and suggestive ECG changes.
Sepsis: Toxi-infectious medical condition characterized by multiple organ failure, incipient or advanced hematological alterations and clinical data of tisular hypoperfusion.
Pulmonary embolism: High risk: sudden dyspnea associated with chest pain or syncope with echocardiographic right ventricular dysfunction, BNP >100pg/d, or both, dimer D >500, and objective demonstration by radionuclide lung scintigraphy V/P, or pulmonary angiography, or CT angiogram, or magnetic resonance.19
Pulmonary embolism: common risk: sudden dyspnea, tachycardia, pleural pain, without right ventricular dysfunction by ECHO, BNP <100pg/dL, or both, dimer D >500, and objective demonstration by radionuclide lung scintigraphy V/P, or pulmonary angiography, or CT angiogram, or magnetic resonance.19
≤60 years
- •
Sudden cardiogenic acute pulmonary edema
- •
Uncontrolled hypertension with ischemic profile chest pain and dynamic ST changes
- •
Ventricular arrhythmias
60–74 years
- •
Dyspnea on exertion progressing medium to small efforts
- •
Heart failure syndrome first event
- •
First event of paroxistic flutter or atrial fibrillation with or chest pain without ischemic profile and ECG dynamic ST changes
- •
Ventricular arrhythmias
- •
Emergency hypertension with or chest pain without ischemic profile and ECG dynamic ST changes
- •
Sudden acute cardiogenic pulmonary edema
≥75 years
- •
Asthenia, adynamia and anorexia
- •
Confusion, syncope or stroke
- •
Dyspnea on exertion progressing from medium to light efforts
- •
First event of paroxistic flutter or atrial fibrillation with ischemic profile chest pain and ECG dynamic ST changes
- •
Hypertensive emergency with ischemic profile chest pain and ECG dynamic ST changes
- •
Ventricular arrhythmias
- •
Heart failure syndrome primer event
- •
AV-block and ischemia on ECG
Sodi-Pallares et al.14
- •
Septal infarction: Q wave DI, aVL, V5 and V6
- •
Anteroseptal infarction: loss of QRS voltage with Q wave in V4, V5 and V6
- •
Left ventricular transmural infarction: RS or rs with negative T wave V4, V5 and V6
Sgarbossa et al.15
- •
ST elevation ≥1mm concordant in leads with R wave or negative slope≥in V1–V3 in leads with S
- •
ST depression ≥1mm in V1, V2 and V3
- •
ST elevation ≥5mm discordant with QRS
Authors: None. The registry had unrestrictive support by Sanofi-Aventis.
The authors declare no conflict of interest.