The purpose of this investigation is to determine the efficacy of orthokeratology (OK) compared to orthokeratology combined with atropine (AOK) for the control of myopia in children. A systematic review that included systematic reviews with meta-analyses, as well as randomized and controlled clinical trials, was carried out in the PubMed, Web of Science, Scopus, Cochrane Library, ProQuest, Taylor & Francis, Science Direct databases, as well as a manual search. Of the Q1–Q4 journals of the Scimago Journal & Country Rank, published in the last 5 years in English and Spanish. Eighteen studies that met the eligibility criteria were considered. The articles selected included 6,866 patients for analysis, where orthokeratology combined with 0.01% atropine was found to be more effective due to its ability to reduce the progression of myopia and axial elongation. In our investigation, it was determined that there could be an additive effect in the combination of 0.01% atropine with orthokeratology in a period of 1–2 years of treatment in patients with mild myopia; however, more multiethnic studies should be carried out, in where a correct evaluation of the progression of myopia, genetic and environmental factors that may influence the results is considered.
El propósito de esta investigación es determinar la eficacia de la ortoqueratología (OK) en comparación con la ortoqueratología combinada con atropina (AOK) para el control de miopía en niños. Se realizó una revisión sistemática que incluyó revisiones sistemáticas con metaanálisis, además de ensayos clínicos aleatorizados y controlados, en las bases de datos PubMed, Web of Science, Scopus, Cochrane Library, ProQuest, Taylor & Francis, Science Direct, además de una búsqueda manual de las revistas Q1–Q4 del Scimago Journal & Country Rank, publicadas en últimos 5 años en idioma inglés y español. Se tomaron en cuenta 18 estudios que cumplieron con los criterios de elegibilidad. Los artículos seleccionados incluyeron 6.866 pacientes para el análisis, en donde se encontró mayor eficacia de la ortoqueratología combinada con atropina al 0,01% debido a su capacidad de reducir la progresión de miopía y alargamiento axial. En nuestra investigación se determinó que podría existir un efecto aditivo en la combinación de atropina al 0,01% con ortoqueratología en un periodo de 1 a 2 años de tratamiento en pacientes con miopía leve, sin embargo, se debe realizar más estudios multiétnicos, en donde se considere una correcta evaluación de la progresión de miopía, factores genéticos y ambientales que puedan influir en los resultados.
Refractive errors are a mismatch between the axial length of the eye and its refractive power, resulting in reduced visión.1 The National Agency for Health Accreditation and Evaluation (ANES) in conjunction with the National Institute of Health and Medical Research (INSERM) in their data collection estimated that the prevalence of visual impairment occurs before the age of 6 years in 20% of cases, where myopia is the most prevalent refractive error worldwide in preschool children.2,3
Myopia has been on the rise in recent years. In data collected in 2000, approximately 1.4 billion people were short-sighted and it is estimated that by 2050 this figure will reach 4.8 billion.4 The epidemic of myopia in children and young adults is characterised by early onset at the age of 6–12 years, combined with high rates of disease progression in adulthood resulting in the risk of developing high (malignant) myopia.2,5
Axial lengthening (AL) is the main risk factor for the development of pathological complications in adulthood, as it is accompanied by thinning of the choroid and sclera, especially in the anterior pole, leading to long-term myopic maculopathy and optic neuropathy associated with high myopia.6 This is why it is useful to reduce the prevalence and progression to high myopia or magna myopia, and to this end, among the measures used for its control is the topical application of atropine eye drops, as well as multifocal lenses, multifocal contact lenses and orthokeratology.6
Management for the control of myopia progression includes atropine eye drops in low doses of 0.01%, 0.025%, 0.05% or higher doses of 0.1%, 0.25%, and 0.5%6–8 in addition to orthokeratology (OK) treatment consisting of the application of gas permeable contact lenses, with the aim of flattening the central cornea to produce mid-peripheral steepening and peripheral myopic defocus, when used at night in order to eliminate daytime myopia.6,7
In the pharmacological field, atropine is the only drug that has shown efficacy in myopia progression, with rates of about −1 D per year in East Asians and about −0.5 D per year in Caucasians.9,10 It was evaluated in 1989 by Yen et al.11 where he mentions that its topical mechanism of action is not yet known but it is believed to produce up- and down-regulation of retinal and scleral muscarinic receptors in the scleral matrix.
The use of OK lenses was first evaluated in 1970 by Kerns, who concluded that changes in refractive error were unpredictable and uncontrollable.12 After several changes in lens design, in 1997 Mountford published a report on overnight reverse geometry contact lenses showing more predictable and sustained reductions in myopia and myopic astigmatism with a retention and regression effect of 8–9 h.12
Subsequent studies helped to establish that overnight OK with rigid gas permeable contact lenses has demonstrated full or partial efficacy in temporarily reducing refractive errors from −4 D to −10 D and was approved by the US Food and Drug Administration (FDA) in 1994.12
Due to the great repercussion of myopia in children and complications in ophthalmic health, it is necessary to maintain control of its progression, which is why this study aims to compare orthokeratology vs. orthokeratology combined with atropine for the control of myopia in children.
Material and methodsA systematic review was conducted by searching PubMed, Web of Science, Scopus, Cochrane Library, ProQuest, Taylor & Francis, Science Direct and LILACS databases, from October 2022 to April 2023, in English and Spanish, for articles meeting inclusion criteria to compare simple orthokeratology (OK) vs. orthokeratology combined with atropine (AOK) in refractive disorders in children. We also handsearched Q1–Q4 ophthalmology journals using the Scimago Journal & Country Rank search engine.
The methodology of the Preferred Reporting Items for Systematic reviews and Meta-Analyses (PRISMA) guidelines used for systematic reviews was applied. Correct terminology was used in the search, using words obtained from the Medical Subject Headings (MeSH) and the Descriptors in the Health Sciences (DeCS).
The keywords used in the search were: "atropine", "child", "efficacy", "orthokeratologic procedures" and "refractive errors". The Boolean expression used was <
Inclusion criteria were: literature reviews with meta-analyses and randomised controlled clinical trials, analysing the efficacy of OK in the control of myopia in children, studies comparing OK with AOK for controlling myopic progression. Articles published in the last 5 years, from January 2018 to March 2023, in full text, in English and Spanish, were selected. Exclusion criteria were: literature reviews, systematic reviews, graduate theses, letters to the editor, clinical practice guidelines, animal studies and articles studied in adults.
At the end of the search, using the three equations, the selected articles were obtained, after which duplicate articles and those that were not relevant to the topic were discarded.
ResultsA systematic literature search was carried out in different databases and then the respective screening was performed to define the articles to be included in the systematic review. The screening assessed that the articles were from the last 5 years of publication, in English, Spanish, full text and that the type of study was in accordance with those established in the inclusion criteria.
Subsequently, articles were selected by title and abstract, duplicate articles were eliminated, and a total of 18 articles were chosen as a result of the three search equations established in the methodology. The results presented in Table 1 detail the efficacy and safety of OK, where effectiveness without adverse effects was demonstrated.13–16 The study by Chen Y et al.13 determined that treatment with OK lenses was effective in patients with unilateral myopia due to a greater decrease in LA, although said study did not consider environmental and genetic factors that may influence myopia progression.
Main articles used to study the effectiveness of orthokeratology for myopia control in children.
| Authors (Year) | Design | Objective | Sample | Results | Conclusions |
|---|---|---|---|---|---|
| Chen Y et al.13 (2022) | Retrospective study | To investigate the efficacy of myopia control by comparing OK with contralateral emmetropic eyes in children with unilateral myopia. | 1 628 children aged 8–16 years with a measurement of −5,25 to −1,00 D. | Over the course of one year, the LA was lower in the OK eyes than in the contralateral eyes. | OK therapy was effective in controlling LA growth in unilateral myopic eyes treated with monocular OK, especially in severe myopia regardless of age and sex. |
| Jakobsen T et al.16 (2021) | Study Control | To investigate the effectiveness and safety for myopia control composed of AL and OK lenses in a given population. | 60 children aged 6–12 years with a measurement of 0.5 and 4.75 D. | The average AL in the OK group was effective, however, no rapid progress was found. | The OK lens treatment reduced LA in myopic children without side effects requiring other treatment or compromising vision. |
| Ding C et al.15 (2021) | Clinical Trial | To investigate the usefulness of OK on accommodative function and aberrations and thus distinguish correlations between them for myopia. | 61 children aged 8–13 years with a measurement of −1,00 and −5,00 D. | During correct lens wear, the area of accommodative lag was smaller and all aberrations in each control increased. After 6 months the changes in accommodative delay were associated with the increase in LA. | Increased HOA and improved accommodative accuracy were observed during treatment with OK, but began to fail after withdrawal of therapy. |
| Jakobsen T et al.14 (2022) | Randomised controlled clinical trial | To investigate differences in peripheral and relative peripheral refraction (RPR) during OK lens wear in children and predictors of myopia progression in a randomised controlled trial. | 60 children aged 6–12 years with a measurement of −0.5 D to 4.75 D. | The OK lens wear caused a markedly myopic RPR at all eccentricities, while the peripheral refraction only changed at two of the six eccentric measurement points. | No correlations were found between change in RPR and treatment efficacy defined as change in LA. |
D, Diopter; OK, Orthokeratology; AL, Axial lengthening; HOA, Higher order total aberrations; RPR, Peripheral and relative peripheral refraction.
In the study by Jakobsen T and Moller F14,16 it was concluded that there were no side effects that require other treatment therapies or are sight-threatening. In the study by Ding C et al.15 observed that after discontinuation of OK therapy, there was no increase in total higher order aberrations (HOA) and failure of improved accommodative accuracy.
The results in Table 2, represent those articles describing the effectiveness of AOK and OK, both applied for the control of myopia progression in children. Most of these studies obtained a sample that share similar objectives focused on the retardation of AL.
Main articles used to study the effectiveness of orthokeratology vs. orthokeratology combined with atropine for the control of myopia in children.
| Authors (Year) | Design | Objective | Sample | Results | Conclusions |
|---|---|---|---|---|---|
| Tan Q et al.17 (2019) | Pilot study | To present the preliminary one-month results of a 2-year randomised trial of atropine combined with OK for myopia control. | 64 children aged 6 to <11 years with measurement of −1, −4,00 D. | No drastic differences were found initially. Mild corneal staining and mild lens fixation were observed. In contrast, the change in LA was greater in the combination therapy. | OK lens treatment had high efficacy in both groups, emphasising that the addition of atropine does not differentiate clinical responses. |
| Tan Q et al.18 (2022) | Interventional randomised longitudinal study. | To determine whether the combination of atropine 0.01% in conjunction with orthokeratology has a greater effect in delaying LA compared to single OK. | 96 children aged 6 to <11 years with a measurement of −1,00 D to −4,00 D. | A longer delay in AL was shown with the AOK group over 2 years. | The presence of minor LA in AOK treatment could be caused by superior pupil dilation and choroidal thickening. |
| Kinoshita N et al.19 (2020) | 2-year randomised trial. | To evaluate the efficacy of OK combined with 0.01% atropine or monotherapy in reducing AL in children with myopia. | 80 children aged 8–12 years with a measurement of -1,00D to -6,00 D | Over 2 years, the AL in both groups slowly, with no significant change by age. | Combination therapy may be effective in slowing AL, especially in children with low baseline myopia. |
| Yu S et al.20 (2022) | Prospective, randomised, double-blind, controlled trial. | To assess the additive effects of OK lenses and atropine 0.01% on slowing AL in myopic children. | 60 children aged 8–12 years with a measurement of −1,00 to −4,00 D. | Both groups showed differences at 12 weeks. | The combination treatment had efficacy in slowing down AL during one year of therapy, with enhancement in the first 12 weeks. |
| Yu Y et al.21 (2022) | Systematic review and meta-analysis | To identify the clinical efficacy of atropine 0.01% combined with OK lenses on ocular AL in myopic children. | 191 children with AOK and 196 with OK. | There was no change in the simple OK, on the contrary, in the AOK a significant efficacy was observed, reducing the AL. | AOK was found to be more effective in slowing AL in myopic children. |
| Tsai H et al.22 (2022) | Systematic Review and Meta-Analysis | To identify the performance of single and combined OK with atropine, we also calculated the surface area under cumulative rating area (SUCRA) to determine the relative ranking of treatments. | 3 435 children under 18. | Using SUCRA analysis, the effectiveness of low-dose atropine was proven: based on the AL in the AOK. | All three therapies demonstrated slowing of myopia progression and slowing of AL. OK proved to be better in combination with low-dose atropine. |
| Wang S et al.23 (2021) | Meta-analysis | Discuss the additive effects of OK and atropine 0.01% for myopic children. | 267 children under 18. | No serious adverse effects occurred in any study. Corneal staining was caused by OK lenses and brief cases of conjunctivitis associated with lens contamination at lens insertion. | AOK was found to have greater efficacy in reducing AL than OK monotherapy alone in children in a short period of time. |
| Hao Q et al.24 (2021) | Prospective, randomised, controlled study. | To find out the changes in the progression of CFShT in myopic children treated with atropine 0.01%, OK or in combination; and to identify the connection between CFShT and AL. | 67 children aged 8–12 with −1.00 D to −6.00 D. | Within the first month, SFChT increased in the OK group and in the AOK, while AL did not increase. After one year, SFChT did not change. | The increase in SFChT was better in the AOK group, within the first month. Therefore, the increase in SFChT influences AL and myopia progression. |
| Yuan Y et al.25 (2021) | Randomised, controlled, double-blind, multicentre, controlled clinical trial. | To recognise the usefulness of AOK and compare with OK lens monotherapy alone in children. | 96 children aged 8–12 years with measurement of −1,00 and −4,00 D. | A change in LA was highlighted, with a significant slowdown in the first 12 months. | The combination of OK lens and 0.01% atropine slows the progression of myopia and AL in children. |
| Yang N et al.26 (2021) | Meta-analysis | To evaluate the effect of AOK with OK lenses alone on AL changes in myopic children. | 229 children with AOK treatment and 232 children with single OK. | OK lenses combined with atropine at low concentrations significantly decreased the AL of low and moderate myopia. | OK therapy combined with low-concentration atropine was more effective than the OK lens in treating children with myopia and in reducing AL. |
| Kinoshita N et al.27 (2018) | Prospective randomised clinical trial | Investigate the additive effects of OK and 0.01% atropine for slowing AL in myopic children. | 41 children aged 8–12 years with measurement from −1,00 to −6,00 D. | Over 1 year, the AL increase of the combination therapy group was found to be more effective than the monotherapy group. | The combination of OK and atropine 0.01% was more effective in delaying AL. |
| Zhou H et al.28 (2020) | Prospective study | To identify changes in the use of OK with 0.01% atropine in the control of myopia progression in children. | 22 children aged 8–13 years with measurement of −2,00 D and −5,00 D. | In the AOK group the spherical equivalent refraction increased with little increase in LA. In the atropine group the increase in LA was related to the initial spherical equivalent fraction but not to the initial age. | AOK was most effective in reducing myopia progression through changes in spherical equivalent refraction. |
| Wan L et al.29 (2018) | Retrospective cohort study | To know how safe the combination of atropine 0.01% and OK is for slow myopia progression. | 179 children aged 7–17 years with a measurement of −1.5 to −7 D | Improvement with combination therapy was observed in both the low and high myopia groups. The LA was noticeably shorter in the AOK group. | Both separate therapies provide effective components to prevent myopia progression, however, greater efficacy was obtained for the AOK combination therapy over the course of 12–24 months. |
| Gao C et al.30 (2021) | Meta-analysis | Preliminary evaluation of the efficacy of joint atropine to OK on AL, for future research. | 341 children under 18. | In five studies, the AL was lower in the AOK group than in the OK group. | Atropine combined with OK was found to be safer than plain OK in delaying AL in children with myopia. |
D, Diopters; OK, Orthokeratology; AOK, Orthokeratology combined with atropine; AL, Axial lengthening. SFChT, Subfoveal choroidal thickness.
The results for the effectiveness of the AOK were based on several parameters. One of the most important was the dioptres of the children. For dioptres measured between −1,00 and −6,00 D, AOK was found to be more effective.13–18,22,23,25,26 Also, several studies have demonstrated the effectiveness of AOK in delaying AL.14,15,17–21,23–25,27,28
Among the studies reviewed, the study by Tan Q et al.17 published their pilot study at 4 months after the start of treatment, while Kinoshita N et al.27 both found a negative correlation between LA and photopic pupil enlargement in AOK treatment. Other results were that of Yang N et al.26 where it was shown that atropine at low concentrations combined with OK is more effective than using the OK lens alone, as well as Tsai H et al.22 determined the relative ranking of treatments using SUCRA analysis which concluded that AOK is effective for myopia progression and AL slowing.
The study by Tan Q et al.17 detailed that a lower AL in AOK therapy may be due to superior pupil dilation and choroidal thickening. On the other hand, we have results from Wan L et al.29 who found that AOK and OK have efficacy in reducing myopia over 12–24 months, although AOK had greater efficacy. Hao Q et al.24 demonstrated an increase in SFChT with AOK and mentioned that it may influence AL and thus myopia progression.
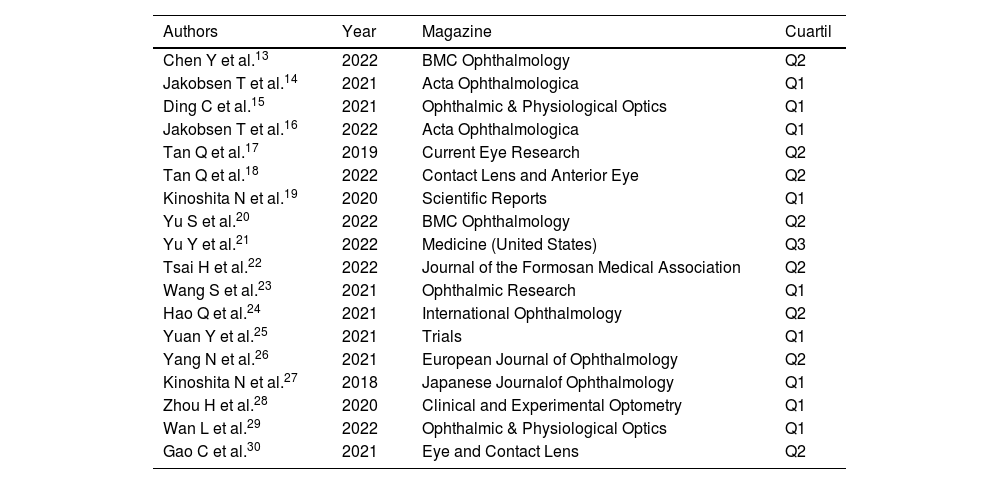
Finally, Table 3 shows the 18 selected articles that were searched in SJR, of which 9 have quartile 1, 8 have quartile 2 and 1 has quartile 3, detailed with the year from 2018 to 2022 and name of the corresponding journal.
Impact of articles used in the systematic review according to the scimago journal rank.
| Authors | Year | Magazine | Cuartil |
|---|---|---|---|
| Chen Y et al.13 | 2022 | BMC Ophthalmology | Q2 |
| Jakobsen T et al.14 | 2021 | Acta Ophthalmologica | Q1 |
| Ding C et al.15 | 2021 | Ophthalmic & Physiological Optics | Q1 |
| Jakobsen T et al.16 | 2022 | Acta Ophthalmologica | Q1 |
| Tan Q et al.17 | 2019 | Current Eye Research | Q2 |
| Tan Q et al.18 | 2022 | Contact Lens and Anterior Eye | Q2 |
| Kinoshita N et al.19 | 2020 | Scientific Reports | Q1 |
| Yu S et al.20 | 2022 | BMC Ophthalmology | Q2 |
| Yu Y et al.21 | 2022 | Medicine (United States) | Q3 |
| Tsai H et al.22 | 2022 | Journal of the Formosan Medical Association | Q2 |
| Wang S et al.23 | 2021 | Ophthalmic Research | Q1 |
| Hao Q et al.24 | 2021 | International Ophthalmology | Q2 |
| Yuan Y et al.25 | 2021 | Trials | Q1 |
| Yang N et al.26 | 2021 | European Journal of Ophthalmology | Q2 |
| Kinoshita N et al.27 | 2018 | Japanese Journalof Ophthalmology | Q1 |
| Zhou H et al.28 | 2020 | Clinical and Experimental Optometry | Q1 |
| Wan L et al.29 | 2022 | Ophthalmic & Physiological Optics | Q1 |
| Gao C et al.30 | 2021 | Eye and Contact Lens | Q2 |
OK is a clinical procedure where rigid contact lenses are used to reshape the cornea and temporarily reduce or eliminate refractive error, although its mechanism of action is not yet well defined.29 However, Wan S et al.23 stated that in the redistribution of the corneal epithelium, the central cornea becomes thinner while the midperipheral cornea thickens, thus contributing to increased peripheral myopic defocus.
In clinical practice, the gold standard for the assessment of myopia progression is the spherical equivalent by cycloplegia.31,32 Even so, most trials consider that axial length measurement is also essential to assess myopia progression, which would allow determining the efficacy of OK lenses.13,16 However, it should be emphasised that the correlation between spherical equivalent and AL is currently not well established.28 in addition to the variability of LA measurement due to the different measurement methods used and factors that may alter its value.18–21,24,26,30
In relation to AL, Chen Y et al.13 established that previous studies determined that OK lenses slow down AL by 32%–55% but various factors such as genetic background, myopia measurement, age, progression rate, race, environment, behavioural habits and duration of follow-up, individually influence the results. The evaluation of a myopic eye with a contralateral emmetropic eye allows to assess the natural growth of AL and therefore to directly measure the efficacy of OK.
In the myopia control mechanism with OK, not only the central refractive error must be corrected but also a peripheral defocus must be created. In myopia magna, this mechanism induces a further decrease of hypermetropic defocus in the peripheral retina, thus exerting a stronger suppressive effect on axial growth.13
In relation to adverse effects Jakobsen T and Moller F14 stated that no complications requiring treatment or affecting vision were observed during the evaluation period. Ding C et al.15 concluded that in the 1-month interrupted OK, baseline HOA and spherical aberration (SA) values were maintained above baseline values, reducing AL by 24% (0.9 mm) and myopia progression by 47% with a refractive error correction of 0.37D.
It has been observed that the combined use of OK and 0.01% atropine has shown an additive effect in decreasing AL in patients tested in the short and long term.17–30 Zhou H et al.28 determined that combined therapy is more effective in controlling AL in children with younger age or lower baseline myopia.
The mechanism of myopia may be related to AL and subfoveal choroidal thinning (SFChT), so the combination of OK lenses and 0.01% atropine effectively and safely slows AL and increases SFChT by affecting oxygen supply and producing chemicals that cause slower AL.22,24
Kinoshita N et al.27 stated that the mechanisms that delay myopia progression with combination therapy are still unknown, although the most reasonable mechanism of OK is defocusing in the peripheral retina with increased HOA through redistribution of the corneal epithelium. Said author also found that single OK has similar efficacy to the combination with atropine alone in children with high myopia.27
Tan Q et al.18 established that there may be an influence of choroidal thickness on LA in the short and long term. In the studies reviewed, it is established that there is a greater change in choroidal thickness in combination therapy. In the first month of treatment a significant axial shortening of approximately 30% was obtained, although the shortening in axial length at one month of evaluation was not a direct result of choroidal thickening and its influence is questionable.18
The exact mechanism of action of atropine is still unknown, but it has been shown to slow the progression of myopia through its pharmacological and optical mechanisms, due to its antimuscarinic and/or α2-sympathomimetic effects and an enhanced optical effect, thus producing an additive effect with the combination of OK, as it induces an increase in myopic defocusing around the retina, improving the control effect on the ocular axis.19,21,27
Yu S et al.20 indicated that atropine and OK modify the biochemical substances responsible for regulating the homeostasis of the eyeball because, in moderate and low concentrations, atropine slows the progression of myopia by its action on the sclera, which influences scleral remodelling or increases collagen cross-linking (due to increased ultraviolet exposure, secondary to pupillary dilation) limiting scleral growth, whereas OK lenses control myopia progression and slow AL through increased peripheral myopic defocus with increased HOA.
Wan L et al.29 found an improvement in myopia control when combining OK lenses with 0.1% or 0.025% atropine compared to OK lenses alone. He stated that the additive mechanism is that they influence pupillary diameter, because they increase retinal illumination by reducing the growth and maturation of the eyes. However, said author stated that another possible mechanism may cause the increase in HOA in combined therapy. Although all had decreased accommodation, it was more significant in the high myopia groups. On the other hand, he found no significant differences in accommodation amplitude, intraocular pressure, tear film break-up time or corneal endothelial cell density between OK alone or combined.
Most of the studies reviewed showed no adverse effects, however, Yu S et al.20 observed that mild photophobia to bright sunlight occurred without discomfort in normal indoor or daily outdoor light, although this problem improved in some cases within six months, after applying eye drops for 1–4 weeks and wearing sunglasses or hats during outdoor activity.
Tan Q et al.17,18 analysed that patients with atropine had a reduction in AL of 0.18 mm in addition to those with single OK with a significant difference between these two control groups accounting for 50% of the overall additive effect in the first 6 months. Despite this, patients with combined therapy had a pupil dilation of 0.54–0.75 mm under photopic conditions and 0.39–0.55 mm under mesopic conditions which were significant compared to normal pupil size measurements of 0.25–0.28 mm, thus the mild mydriasis that occurs predisposes this group to photophobia.
Many of the studies had various limitations, Kinoshita N et al.19 determined that future research should focus on measuring peripheral refraction, HOA and pupil diameter for more accurate results. In addition, a higher concentration of atropine, such as 0.025% or 0.05%, could be meaningful, especially in patients with moderate baseline myopia, but most of the studies were only performed with low doses of 0.01%.19,20 Jakobsen T and Moller F14 advised periodic checks every 3 months to eliminate agents affecting the health of the corneal surface.
Wan S et al.23 indicated that most of the published studies are conducted in Asia, and it is important to focus these evaluations on large-scale, multi-ethnic, double-blind studies. In addition, it is imperative that subsequent studies monitor the treatment groups and evaluate factors that influence myopia progression and AL such as environmental factors, i.e., the amount of time participants work using near vision or in outdoor activities, and genetic factors.18,19,22,23
ConclusionsThe combination of atropine 0.01% with orthokeratology over 1–2 years of treatment in patients with mild myopia was found to be most effective. Although the exact mechanism of action on the eyeball is still unknown, it is believed to provide an additive effect that influences axial lengthening. The use of atropine at medium doses is still under study, but may be beneficial in patients with moderate to high myopia, although the greater number of adverse effects at higher doses should be taken into consideration.
Most research is directed at the combination of these two therapies, so it would be ideal to conduct more studies directly comparing atropine with AOK. In the future, more multi-ethnic studies should be conducted to evaluate myopia progression by means of spherical equivalent under cycloplegia, the influence of genetic and environmental factors that may contribute to greater myopia progression and possible complications that may occur with this treatment, in order to obtain more precise data to corroborate its efficacy and safety.
Conflict of interestThe authors state that they have no commercial interest and have received no financial support.
FundingThis systematic review has been self-funded, with no specific support from public sector agencies, the commercial sector or non-profit organisations.
The authors would like to thank the Universidad Católica de Cuenca and especially PhD. Fabricio Guerrero for his collaboration and logistical support for this study.