Introduction
Primary health care centres (PHCC) have to provide care to those patients who want to be seen that same day because they cannot wait for a scheduled appointment with their usual doctor. In Spain, as in other developed countries, there has been spectacular increases in demand for these spontaneous or urgent visits.1-5
This increase in demand has been attributed to different causes.2,6,7 Added to a progressively ageing society accustomed to being dependent on the system, are new generations of an immigrant population that have not been taken into account by managers and politicians. On the other hand, there is the decrease in the number of health professionals, due to bad planning, in both training (university level) and management. However, at the same time a sizeable majority of family medicine and nursing professionals have increased their knowledge and skills to tackle health problems that, until now, were not resolved in primary care. Finally, the subjective perception of the seriousness and patient anxiety, considered by other authors as the most important determining factor of the urgent visit, must be pointed out.2,6,7
Several actions have been proposed to reduce health care pressures caused by the excessive demands of urgent visits.8-12 One of these has been the care of mild illnesses by nursing professionals. There are different studies that have evaluated a series of actions in which these professionals (nurse practitioners) resolve health problems classified as mild or non-urgent, with a high level of patient (user) satisfaction, low levels of drug prescriptions, little need to refer to family doctors and a low percentage of new visits for the same problem in the 3 days after the consultation.13-15 None of these studies were carried out in our country, which limits the extrapolation of their results to Spain.
The aim of our study is to evaluate a solution to the demand of urgent visits for the same day in a PHCC, by applying a nursing practice guide.
Methods
Design
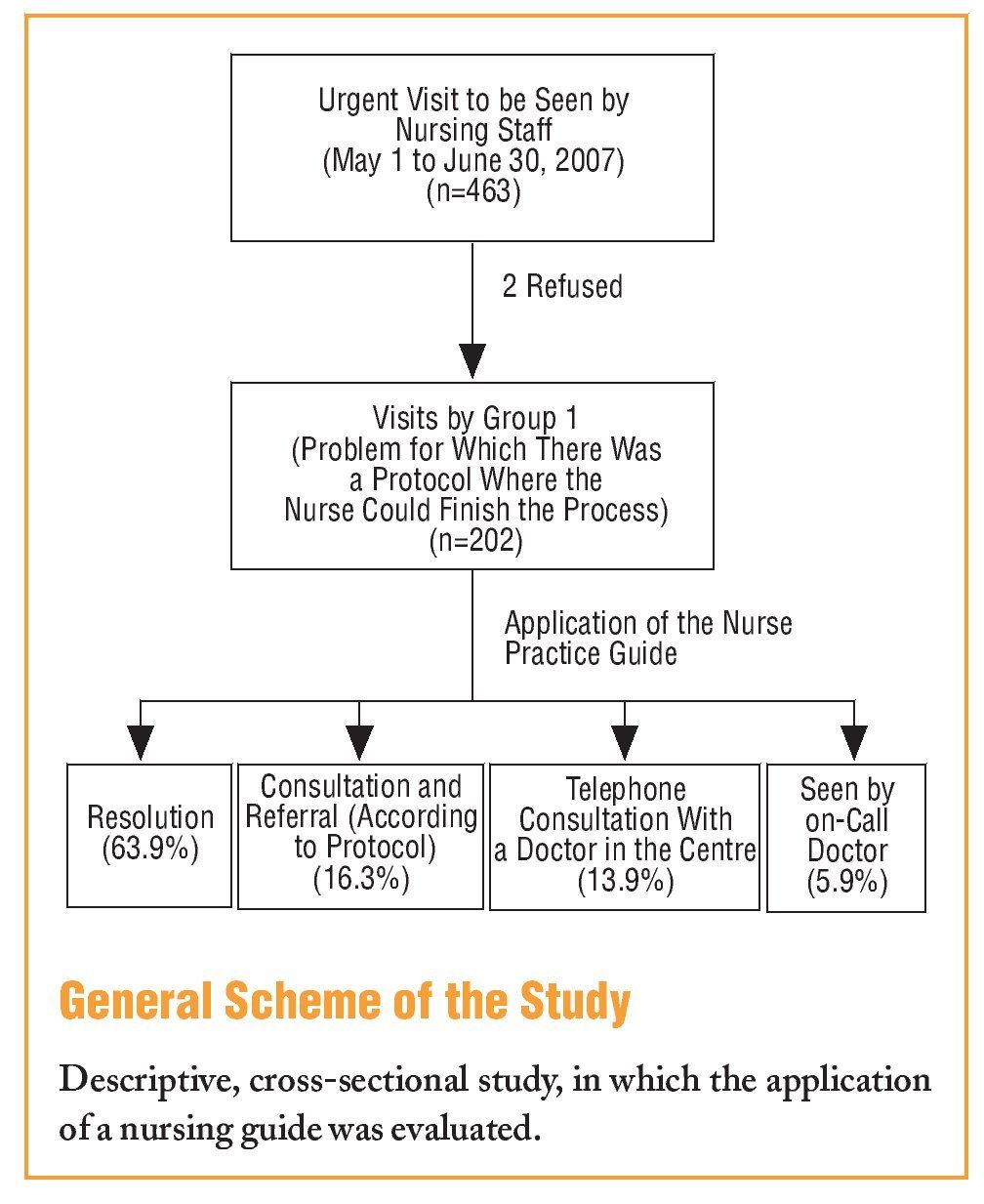
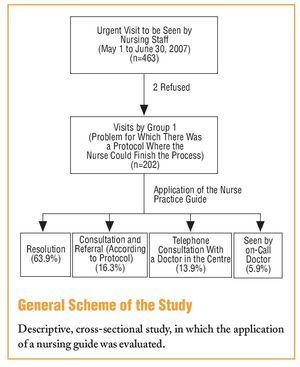
It is a descriptive, cross-sectional study.
Actions
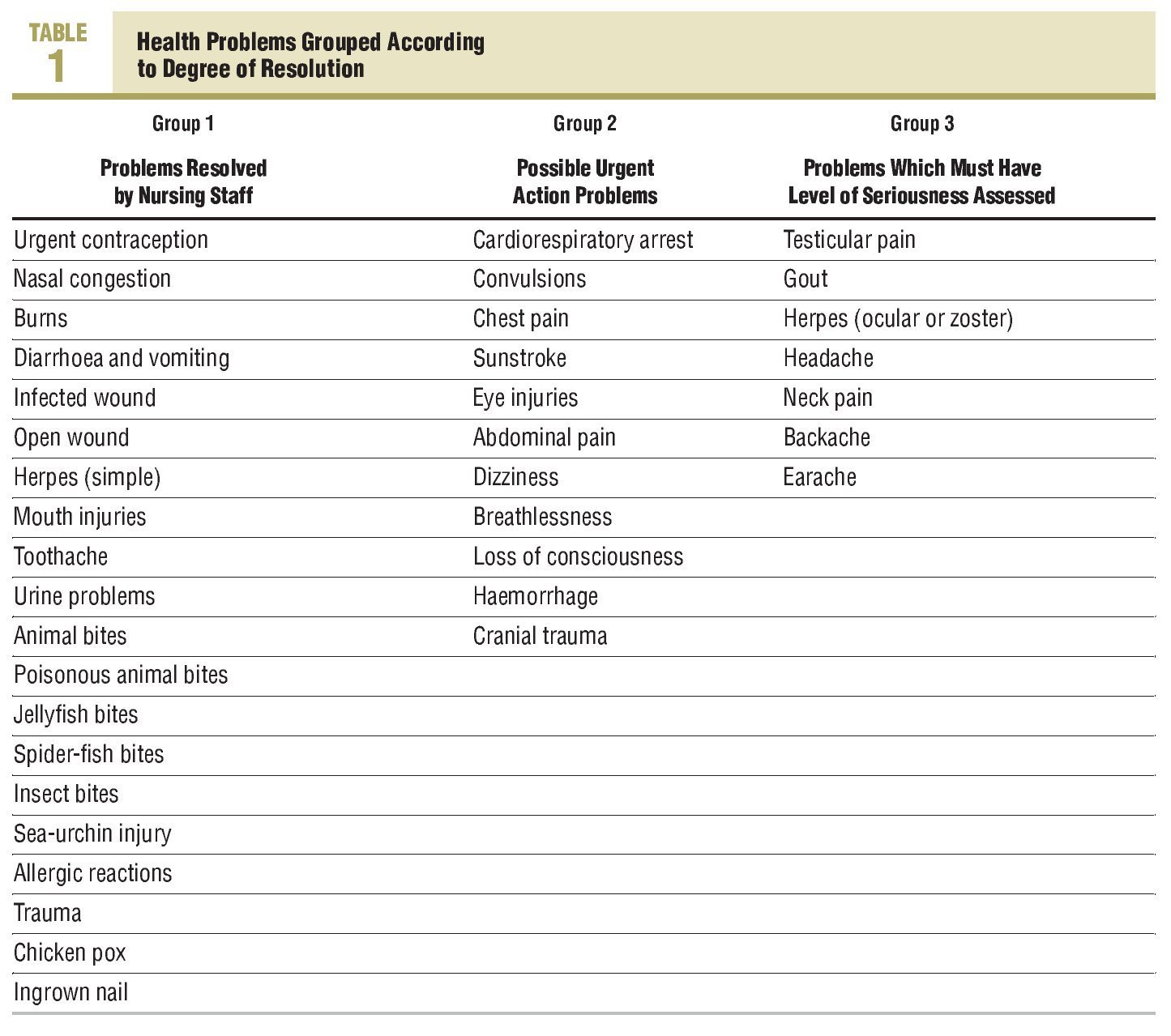
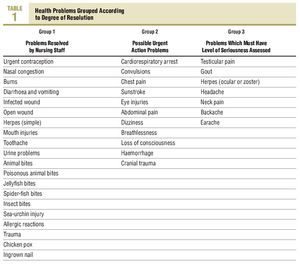
Firstly, a resolvable demand profile was prepared by the nurses. The health problems, using a consensus of the whole health care team, were classified into 3 groups: a) group 1, health problems where there were protocols that allowed the nurses to complete the process, and could be responsible for receiving and resolving them; b) group 2, situations, that are possible emergencies in which the nurse professional acts independently in the first part of the algorithm, that subsequently require action by the doctor, and which gives rise to a shared completion of the process; and c) group 3, health problems that require an assessment of their seriousness, before action is taken by the doctor, and that only take place when their visit list is saturated.
Each health problem is structured into 3 sections: a) short description of the problem; b) an action algorithm which includes, anamnesis, assessment, and action (that may be from resolving the problem to the referral or shared action between nursing and medical staff ); and c) possible NANDA (North American Nursing Diagnosis Association) diagnoses that better describe the problem with the nursing outcomes classification (NOC) from which the nursing interventions classification (NIC) arises.
Specific training was then given to increase the skills of the nursing staff and, at the same time, the administrative staff were trained so that they would understand the nomenclature, identify alarm signs and improve the correct referral of the patients. Monthly sessions were also held to identify what were the weak points in the cycle.
Subjects
The study included all patients who asked to be seen on the same day in the Can Bou PHCC in Castelldefels (Barcelona), and whose health problem belonged to group 1. The study period was from May 1 to June 30, 2007. Patients who did not accept being seen by nursing staff were excluded.
Each family doctor has 6 urgent visits daily. Once their list is full, the patients are seen by the on-call doctor, up to a total of 16 visits. When the continuous healthcare list is full, the patients who request an urgent visit are seen by the nurse responsible for the care on demand clinic. The nursing staff changes each day and shift (morning and afternoon), in this way all the adult care nursing staff have one day a week when they are scheduled to see to the urgent visits of the whole centre.
Study Variables
The reason for the visit, age, sex, and results obtained were collected. While applying the guides, 4 possible results were distinguished: a) resolving the health problem without consulting any other professional or making a referral outside that established by the protocols; b) consult with another professional and refer the patient to be seen in another centre and/or carry out a complementary test; c) consult another professional and resolve the problem; and d) refer to the on call doctor of the centre. It was also determined whether visits not indicated by the nursing staff had been made in a period of less than 2 weeks. Cases where a patient was seen again, due to lack of improvement, doubts about the treatment, or for other reasons, were analysed.
Statistics Analysis
The quantitative variables were described using the mean and standard deviation, and the quantitative variables using percentages. The quantitative baseline characteristics were compared using the Student t test. The Pearson c2 test was used for the qualitative variables. In all the calculations, a P value less than .05 was considered significant. The analysis was performed using the SPSS 15.0 statistics package.
Results
Of the 38 health problems that had set protocols, 20 of them were within protocols that allowed the nursing staff to resolve the process (Table 1).
Of the 463 urgent visits for nursing care recorded during the period of the study, 202 belonged to group 1 (health problems with protocols in the guide in which the nurse was the person who finalised the process).
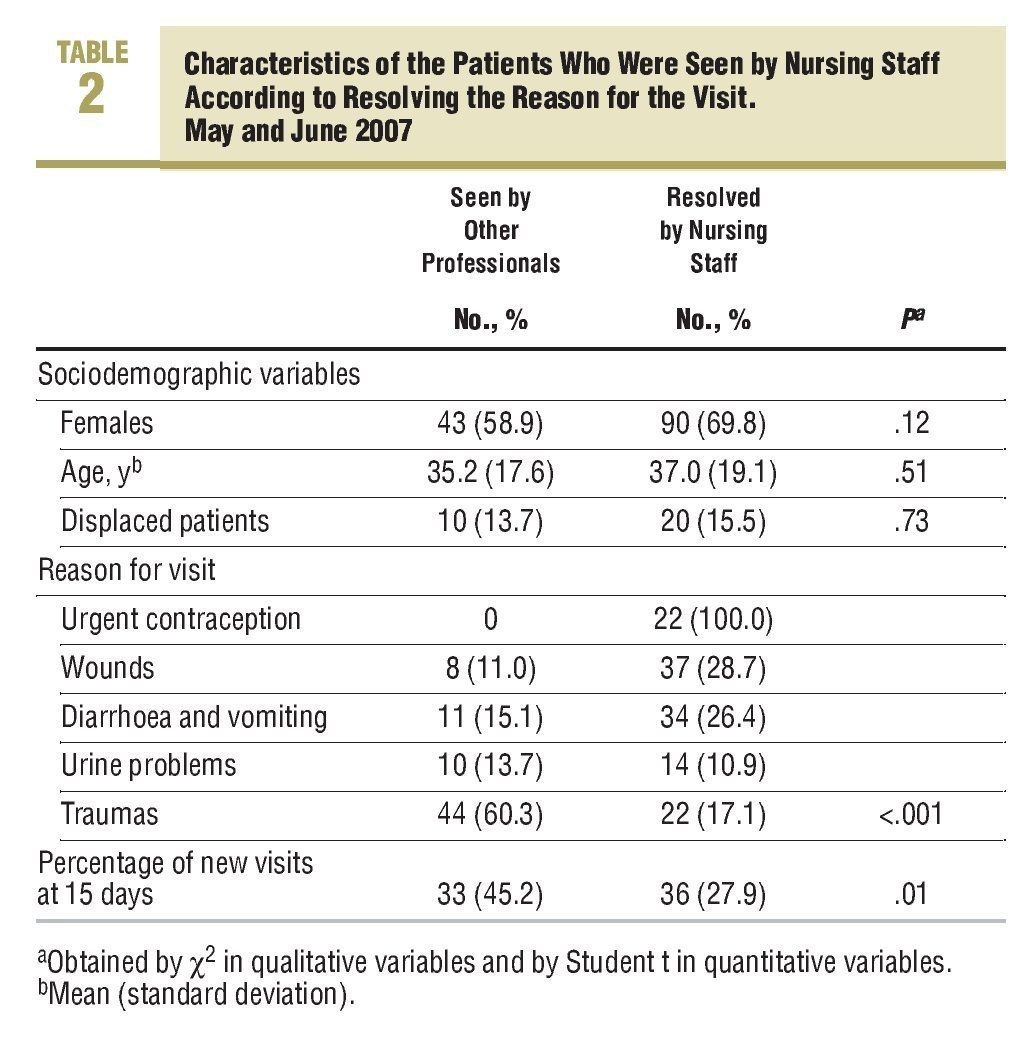
Only 2 patients refused to be seen by nursing staff. The mean age of the patients seen was 36.3 years (SD, 18.6 years) and 65.8% were female. The most common reasons for the visits were, traumas (32.7%), followed by diarrhoea and vomiting (22.3%), skin lesions (22.3%), genitourinary (11.9%), and urgent (10.9%).
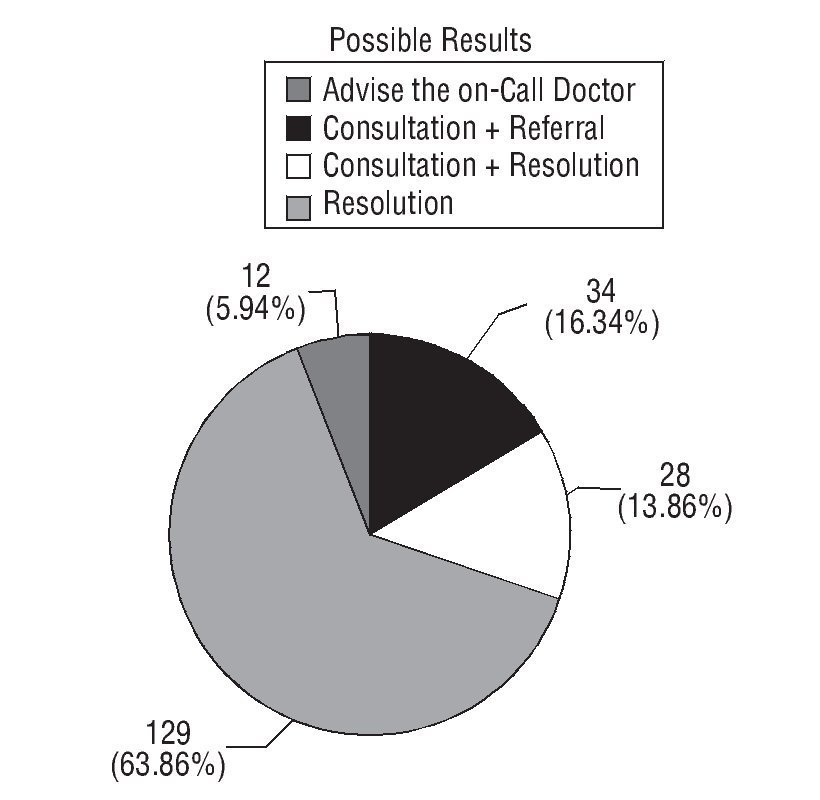
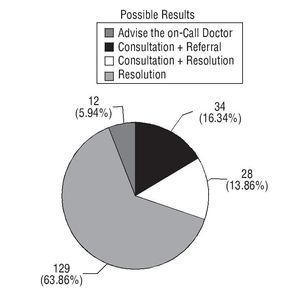
The health problem that led to the visit was resolved in 63.9% of cases by nursing staff applying the action protocol. A referral was made to another service, following that indicated in the guide, in 16.3% of the cases seen. A telephone consultation with a doctor in the centre was required in 13.9% of the cases. Only in 5.9% of cases did the patient end up being seen by the on-call doctor (Figure 1).
FIGURE 1 Percentage of possible results after applying the guides.
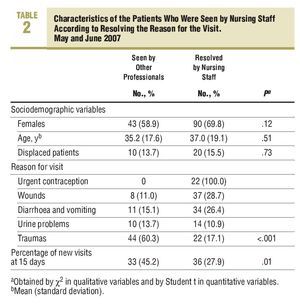
It was observed that the health problems most often resolved by the nursing staff were urgent contraception in 100% of cases and wounds (28.7%). The most common health problem seen was trauma (Table 2).
Of the total, 65.8% of the patients seen did not return to the centre within the 2 weeks following the visit, and 22.3% made a review visit indicated by the nursing professional who attended to the patient.
Discussion
The approach to acute illnesses using a nursing operational guide in a PHCC is an effective intervention and resolves the health problems of the patient users who arrive spontaneously to be seen by a doctor. A total of 63.9% of the health problems attended to by nursing professionals was resolve without consulting or referring the patient to another centre. Also, 65.8% of the patients did not make another visit to the PHCC for the same health problem within the 15 days after receiving care. However, the consensus established on the degree of resolution, although being evidence and literature based, must be adapted to the reality of the team, entails a certain increase in workload in the process of achieving it,16 and involves having continuous work sessions to establish confidence between the different players. We emphasise that, the preparation of the guide has been indispensable in constructing a homogenous resolution profile for the whole nursing team of the centre, has improved the knowledge and skills in critical interpretation of these professionals, as well as in medicine and evidence based nursing. The gradual application of the guide helped to identify points for improvement. Among those, the exact training needs to achieve the desired resolution level and those that are detected in interviews with the professionals and in staff meetings. Using this strategy, workshops on dressings and immobilisation, cardiopulmonary auscultation, otoscopy, pharmacology, cardiopulmonary resuscitation, assessment of a normal electrocardiogram, rotation into Hospital Emergency Departments to improve technical skills (catheters, placing of intravenous lines), suturing workshops, and assessment and approach to urgent illnesses.
Attending to mild health problems by nursing professionals is normal practice in the United Kingdom and North American countries.14,15 In 3 systematic reviews of the results obtained in these countries,13-15 similar results to those obtained in our study were observed: nurses and doctors achieved similar health results in the patients. These studies also mentioned a high level of patient satisfaction when the nursing professional attended to them during the first contact when they required care on the same day.13-15
The assessment of our results need to be expanded and, although there is good acceptance by the users, we also have to prepare a satisfaction survey on this service.
As regards the cost of care by nursing staff compared to care by the doctor, results obtained in previous studies are contradictory. In 1 study it was observed that training the nursing professionals cost 30.35 pounds, but the average cost of being seen by a nurse was 9.46 pounds, and that of the doctor was 9.30 pounds.17 However, another study states that the cost of being seen by the doctor was 60% higher than those provided by nurses.18 Studies on cost effectiveness need to be carried out in our country.
One possible limitation of our study is that information on new visits was obtained from the computerised clinical history in the centre, therefore it could not be identified whether a patient had gone to another centre. However, the large majority of patients seen (85.1%) are users of the PHCC, which means they usually receive their care in our centre, and only 14.9% normally receive their care in another. On the other hand, the cross-sectional nature of the study means that the long-term effects of the care cannot be determined, therefore more studies need to be carried out on the effectiveness and cost-effectiveness of replacing doctors with nursing professionals.
In conclusion, the preparation of the guide enabled a resolution profile to be constructed with excellent homogeneity for the whole nursing team, and means that nursing professionals are a normal entry door to the Primary Health Care System. For this reason, we consider the project is very positive and we believe that it could be a reference for other organisations.
What Is Known About the Subject
•The demand for urgent visits in Primary Care Health centres has increased in all developed countries
•Care of mild health problems by nursing staff is normal practice in the United Kingdom, the United States, and Canada
What This Study Contributes
•The approach to acute illnesses using nursing practice guides resolves the health problems of the users with mild disorders
•Nursing staff can become a standardised entrance into the primary health care system
Source of Finance: GlaxoSmithKline, SA
Spanish version available www.doyma.es/222.577
Correspondence: A. Brugués i Brugués.
Centro de Salud Can Bou. CASAP. Avda. Ciutat de Màlaga, 18-20. 08860 Castelldefels. Barcelona. España.
E-mail: abrugues@casap.cat
Received September 13, 2007.
Accepted for publication February 18, 2008.