Pharyngitis is one of the most common causes for seeking health care in the primary care clinic. In the majority of cases it is due to a viral aetiological process which is self-limited in less than a week. Only a small percentage is it of bacterial origin (10%-15%) and it is that known as tonsillopharyngitis or acute tonsillitis. Different bacterial agents have been described as causing this infection, but it is, without a doubt, those caused by Streptococcus pyogenes that require appropriate antibiotic treatment, since it has been shown that this reduces the symptoms of the infection, cuts the transmission of the streptococcal infection and decreases the suppurative and nonsuppurative complications. In normal practice the diagnosis is clinical and therefore the treatment is empirical. However, many studies alert on the inappropriate prescribing of antibiotics for this complaint, mainly as regards its over-treatment, subjecting patients to the various problems of excessive antibiotic treatment, such as secondary effects and the spread of resistances in the community.
An article is published in this issue on the validity of a rapid diagnostic test in the diagnosis of streptococcal pharyngitis, to be precise, a rapid antigen technique. It is not the first time that a study with these characteristics has been published in this journal and, as the authors state, similar works have been published, some of them more than 15 years ago. The results of all these studies advise the use of these techniques in primary care clinics. So, we should ask ourselves, why they are not in general use, not even in paediatric clinics where the incidence of streptococcal infection is higher than in the population over 14 years old. Certainly, these techniques are now more sensitive and specific than they were 15 years ago and an example of this are the improved results observed in the recent study by Llor et al.
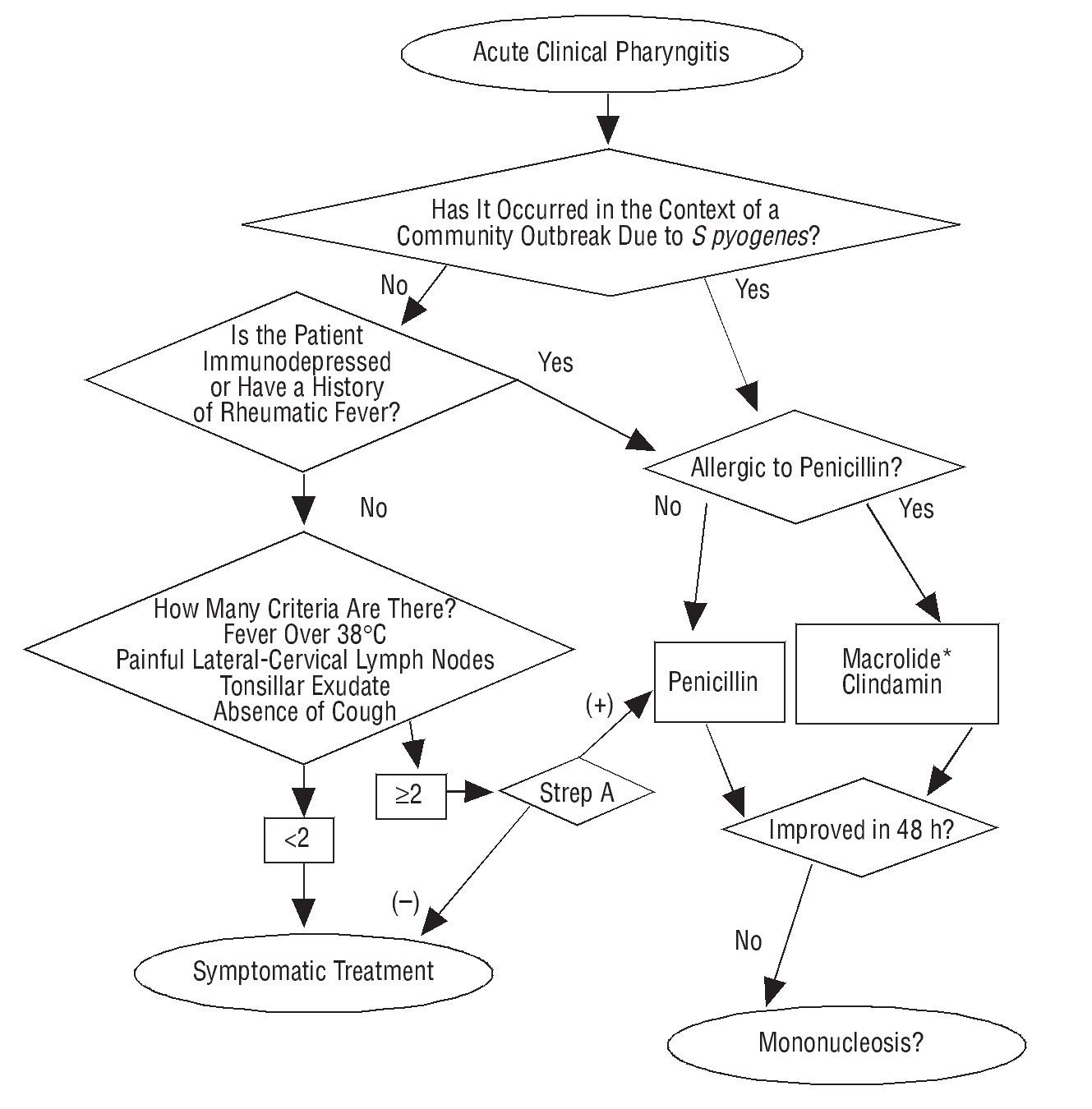
Another positive aspect, and one which the authors point out, is the high negative predictive value found for the diagnosis of streptococcal pharyngitis, an aspect much appreciated by the doctor, since with a negative result infection due to S pyogenes can be almost certainly be ruled out. This is a fundamental aspect, particularly if it is taken into account that in the countries where these techniques are applied, antibiotics are still prescribed with negative results. In 1 study carried out in the United States it was shown that up to 30% of patients with negative results were prescribed antibiotics by their family doctor.1 Another aspect worth mentioning in the study by Llor et al is the limited validity of the clinical data for diagnosing streptococcal pharyngitis. Although it is already well known, it is worth pointing out that these much used criteria, such as the presence of tonsillopharyngeal exudate or fever, are just a few more predictors of the streptococcal aetiology which, in their absence and curiously in this study, no statistically significant differences were seen. These 2 criteria, along with the presence of painful lymph nodes in the neck and absence of cough, make up the 4 criteria for receiving antibiotic treatment, described for the first time by Centor et al in 19812 (since then these criteria are also known by the name of this author). Many clinical practice guides, among which include that of the North-American Society of Infectious Diseases, recommend taking these criteria into account and in those who have 2 or more, make sure of the streptococcal aetiology by using rapid antigen techniques,3 since even in those patients who have all the Centor criteria, less than half of them have streptococcal pharyngitis. Only in positive cases should antibiotic treatment be given, which, in patients not allergic to penicillin, should be penicillin V, at a dose of 1 200 000 U which can be taken every 12 hours. It is a pity, that in view of the absence of S pyogenes resistances towards this antibiotic, it is replaced with other wider spectrum antibiotics and, therefore, with a higher tendency to produce resistance.
On the other hand, it has been published that there is a 30% resistance to macrolides, by an induced resistance mechanism, in such a way that in a high percentage of cases resistance is produced against 14 and 15 atom macrolides but not against those with 16 atoms. For this reason, it is not recommended to administer the latter or lincosamides as a treatment of choice in patients with a possible allergy to betalactams in Spain (Figure 1).4 The use of these rapid antigen techniques is no more complicated than using urine reagent strips and do not take an excessive time. Even in positive cases, the diagnosis can be achieved in no more than 2 minutes from the start of the determination. They are in general use in the majority of European countries, as well as in the USA and Canada.5 The publication of this study should represent an inflection point and, along with other current projects, like the Happy Audit, that looks to introduce rapid diagnostics into the clinic, it should represent a raising of awareness and a change of habits by family doctors and paediatricians. Of course, these results should be accepted by the administration, which should provide our health centres with these diagnostic tests. One determination costs approximately 3 euros, somewhat less than a pack of penicillin. This factor, along with taking into consideration that the population will be exposed to antibiotics when these are not indicated, solves a public health problem, for the patient who will not have to take an unnecessary antibiotic, thus avoiding possible secondary effects, and for the community, by controlling the increase in resistances. Therefore, what are we waiting for?
FIGURA 1 Approach to diagnosis and treatment of acute pharyngitis. *16-atom macrolides, such as josamycin or midecamycin are preferred. If it is recurrent pharyngotonsillitis the amoxicillin-clavulanic acid combination must be used.
Key Points
• Streptococcus pyogenes is the most common bacteria in bacterial tonsillitis, with 0% resistance to penicillin.
• Clinical criteria have a sensitivity of 50%, even with 4 Centor criteria.
• Treatment based only on clinical symptoms causes over-use of antibiotics.
• Rapid diagnostic techniques to detect S pyogenes are reliable and useful, they have a negative predictive value of 98.5% and very easy to use in the primary care clinic.