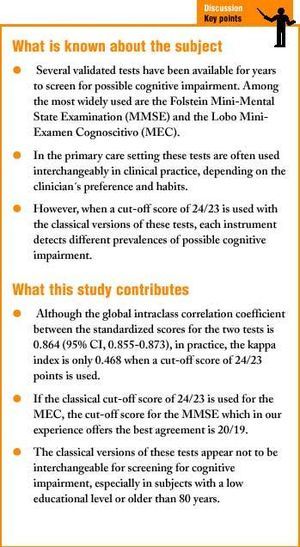
Introduction
Most clinical guidelines and consensus documents do not recommend systematic screening for dementia in the general population.1-3 However, when caregivers or physicians suspect cognitive impairment, the patient should be examined and followed.4 Several validated instruments have been available for years to detect possible cognitive impairment.5 The Folstein Mini-Mental State Examination (MMSE),6 which dates from 1975, is one of the most widely used tests world wide, and validated translations have been produced in several languages including Spanish.7,8 Despite the low specificity of the MMSE, different studies have shown good interobserver agreement and short-term test-retest agreement. Accordingly, the NINCDS-ADRDA recommends this test as a screening instrument to detect possible cognitive impairment.9
In 1979 Lobo et al.10 adapted the MMSE for the Spanish-speaking population, naming the instrument the Mini-Examen Cognoscitivo (MEC) and modifying some of the items such that the total score obtainable on the MEC is 35 points rather than 30 points, as in the MMSE. Since then both tests have been used interchangeably in primary care for the early detection of cognitive impairment. However, studies done in recent years have tended to favor the Spanish translation of the MMSE, possibly with the legitimate aim of comparing studies in Spain with other international studies. Such comparisons have been facilitated by the 30-point version of the MEC,11 in which the items involving abstract thinking (2 point) and digits (3 points) have been deleted.
Our hypothesis was that the classic 35-point MEC and the Spanish version of the MMSE could not be used interchangeably to screen for cognitive impairment.12 The aim of the present study was therefore to compare agreement between the MMSE and the MEC in daily clinical practice.
Material and methods
This study was done within the framework of the Cuida´l project, a multicenter, controlled randomized clinical trial in process at the time of writing, which was designed as reported previously13 to determine the effectiveness of a specific intervention aimed at caregivers for patients diagnosed as having dementia. In the first phase of the project a cross-sectional study was done with a random sample of persons older than 64 years who were served by 53 primary care centers in Catalonia (northeastern Spain). One hundred patients were chosen at random from each primary care center, for a total of 5300 patients. At the discretion of each patient´s family physician and licensed nurse, these persons were recruited by telephone and in writing, or when they visited their center for any reason other than to seek medical care. We excluded institutionalized patients, itinerant patients living at a temporary address (and planning to remain at this address for less than 6 months), and patients with a chronic illness and extreme cognitive impairment that prevented them from taking part in the interview. Participation in a home care program was not an exclusion criterion.
After a training period the primary care team responsible for the patient (physician or licensed nurse) administered the MMSE and the MEC simultaneously to all selected patients in the course of a scheduled, 20-30 min visit to the health center. Items common to both tests were presented only once, and the response was considered valid for scoring both instruments. For example, the questions «What day of the week is it?», «What is today´s date?», «What month is it?» and «What year is it?» were presented only once, and the responses were considered valid for both the MMSE and the MEC. In contrast, items that differed in each of the two tests were presented alternately. When the researcher considered it appropriate, the interview took place at the patient´s home. All subjects (n=3167) belonged to a subsample of the participants in the Cuida´l program. Analysis of the data was based on all patients who satisfied the inclusion criteria and for whom complete and correctly recorded results for both the MMSE and MEC were available.
Measures
The Spanish version of the MMSE consists of 30 items, and each correct answer is scored as 1 point. It evaluates six cognitive abilities (Annex 1), and takes 5-10 minutes to administer. Suitably trained health care personnel can administer the test.
The MEC is analogous to the MMSE and conserves the same structure based on six cognitive abilities, but incorporates 5 additional items, 3 referring to attention and concentration, and 2 dealing with language (Annex 2). The subtraction item is not based on a series of sevens, but asks the subject instead to perform five successive subtractions of 3 units from 30, which is much easier. In contrast to the MMSE, the highest possible score on the MEC is 35 points. In both tests the item that asks «What hospital are we in?» was replaced with the question «Whose doctor´s office are we in?» (The physician´s or nurse's name was taken as the correct answer.) If the tests were given at the patient´s home, this item was replaced with the question «Whose home are we in?». The name of the district was accepted as correct in place of the province or region of Catalonia.5 To facilitate the simultaneous administration of the two tests, the language item «There were five dogs in a field of wheat» (originally «No ifs, ands or buts» in the English version of the MMSE) was repeated.
Statistical analysis
Because this was an analysis of a subsample from the Cuida´l trial, sample size was calculated on the basis of the primary aims of the main study.13 We assumed a prevalence of dementia among persons older than 64 years of 5%, and a nonresponse rate of 10%. This meant that 4750 persons older than 64 years needed to be screened; the final number was 5300. McNemar´s test was used to compare the number of positive findings of cognitive impairment (ie, a score ¾24) obtained with the two tests.
The intraclass correlation coefficient was calculated for fixed effects of the score on the MMSE and MEC. Because the maximum MEC score (35 points) was higher than the maximum score for the MMSE (30 points), these variables were standardized before the analysis.
Different cut-off scores for the two tests were identified as indicating a positive finding of cognitive impairment, and agreement between the two results was calculated as the kappa index. Logistic regression was used for the variables age, sex and educational level as predictors of good agreement (cut-off point ¾24 points).
All analyses were done with version 10.0 of the Statistical Package for Social Sciences (SPSS-Win).
Results
Description of the population
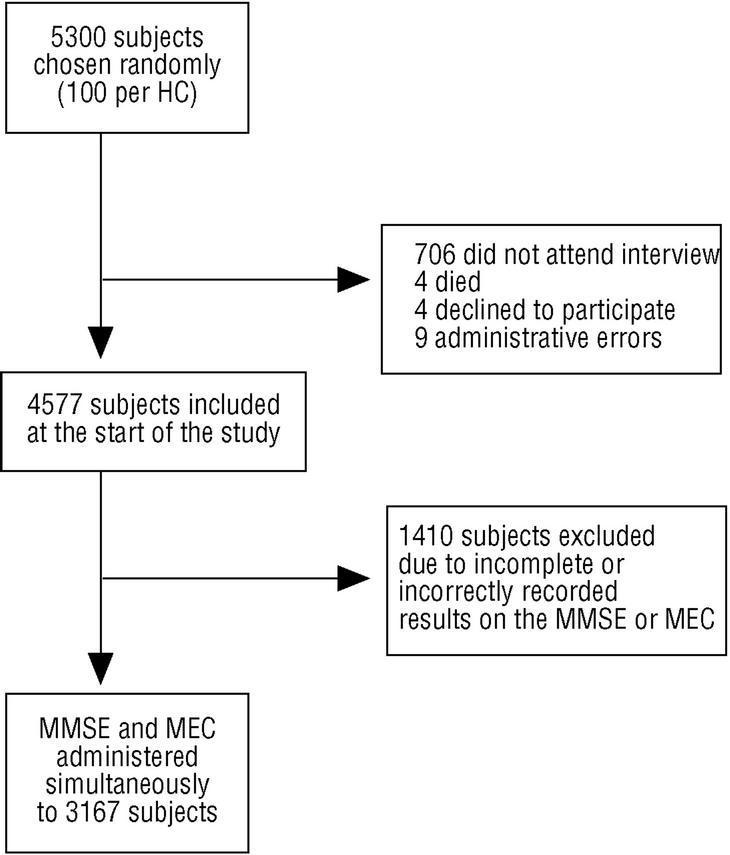
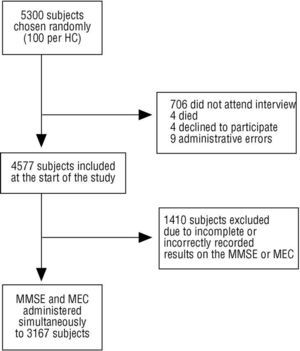
Of the 5300 subjects initially selected, 706 did not attend the interview or could not be located; 4 had died; 4 declined to participate; and 9 were included because of an administrative error. Of the 4577 eligible participants, 1410 (30.8%) were excluded because one or both tests could not be given correctly or completely (Figure 1). The final sample comprised a total of 3167 patients for whom complete, correct data were obtained. Mean age and standard deviation (SD) was 74 (6.1) years; 17.5% of the participants (n=554) were 80 years old or more. Slightly more than half (n=1611, 50.9%) were women. The number of patients who could not read or write or who were functionally illiterate was 954 (30.1%). Most were married (n=2080, 65.9%), 874 (27.7%) were widows or widowers, and the remaining participants were unmarried, separated or divorced.
Fig. 1 Scatterplot showing the scores on the MMSE and MEC. To facilitate comprehension of the graph, lines along each axis indicate a score of 24.
Estimate of prevalence
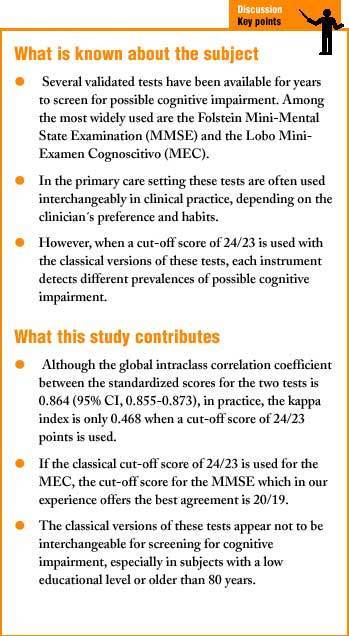
With a cut-off score in both tests of ¾24 as a screen for a positive result, the prevalence of suspected cognitive impairment was 16.52% (n=449) according to the MMSE and 5.49% (n=165) according to the MEC (P<.001).
Estimate of agreement
The overall intraclass correlation coefficient for the two standardized scores was 0.864 (95% CI, 0.855-0.873). By age group, the intraclass correlation index was 0.76 (65-69 years), 0.77 (70-74 years), 0.83 (75-79 years) and 0.91 (older than 79 years). With a cut-off score of ¾24, the MEC results tended to identify fewer subjects as having suspected cognitive impairment (Figure 1). We used the method proposed by Bland et al.14 to calculate the difference between the standardized MEC and MMSE scores, and these differences were in turn standardized. Numbers below 1.96 or above 1.96 were the extreme values (Figure 2): with a MMSE score close to 24 but below 25, a large positive difference was seen (the MEC tended to yield higher scores than the MMSE), whereas beyond this cut-off score the opposite occurred.
Fig. 2 Scores on the MMSE plotted on the horizontal axis, versus the standardized differences between standardized scores on the MEC and MMSE, plotted on the vertical axis. Values lower than 1.96 (MMSE>MEC) and higher than +1.96 (MEC>MMSE) represent extreme values.
Because clinicians do not use these scores on a continuous scale but rather use a cut-off score to categorize a given subject as having a positive or negative screening result, we calculated the kappa index for different cut-off scores on both tests to try to determine where agreement was greatest. As shown in table 1, when a cut-off score on both tests of ¾24 points was used (as is customary in clinical practice), the kappa index was 0.468, whereas with a cut-off score of ¾20 for the MMSE and ¾23 for the MEC, the kappa index increased to 0.788.
The results obtained with the logistic regression model for predicting good agreement between the two tests (cut-off at ¾24) are shown in table 2. The variables educational level and age #>80 years were statistically significant; the former as a predictor of good agreement, the latter as a predictor of poor agreement. Table 3 shows how agreement between the two scores varied across different subgroups.
Discussion
For a cut-off score of 23/24, the sensitivity and specificity for detecting dementia were reportedly 87% and 82%, respectively, for the MMSE,15,16 and 89.8% and 83.9%, respectively, for the MEC.10 Some authors have reported a higher sensitivity for the MEC (93.5%).17 Although the sensitivity in detecting dementia was similar in both tests, in the present study the prevalence of suspected cognitive impairment, identified with a cut-off score of 24/23, varied significantly between the two under conditions similar to those encountered in every-day clinical practice. Under these conditions, when clinicians use the MMSE they probably need to make a greater number of diagnostic decisions afterwards, such as the indication for complementary tests (laboratory tests, psychiatric examination, imaging tests, etc.). In contrast, if the MEC is used fewer of these complementary tests will be needed. However, the present study was not designed to determine which of the two tests is better at screening for cognitive impairment, hence we cannot say whether either of the two is the more effective or efficient. The results do suggest that they cannot be used interchangeably in the primary care setting as if each were a substitute for the other, at least when a cut-off score of 24/23 is used. Their agreement in practice is only moderate, as clinicians do not interpret the test scores on a continuous scale but rather as a dichotomous result: above or below the cut-off score. Under these conditions it seems prudent to consider these tests as not equivalent or interchangeable, especially for certain population groups. According to our results the discrepancy widens in patients with a low educational level and in those older than 80 years; in these subgroups the two instruments should not be used interchangeably. Our data favor the use different cut-off scores depending on the patient´s educational level, as proposed by Escribano et al.7 for the MMSE.
Comparison with other studies
Lobo et al.10 recently showed a cut-off score of 23/24 on the MEC to be valid for older patients, and proposed a 30-point version of the MEC to facilitate comparisons with other international studies based on the MMSE.
Bermejo et al. compared the diagnostic effectiveness of the MEC with that of two versions of the MMSE: that containing the «serial sevens» subtraction, and that containing the request to spell mundo (world) backwards.18 In this study the diagnostic performance of the Spanish translation of the MMSE that contains the «serial sevens» item was similar to that of the MEC. These authors suggested that the Spanish version of the MMSE could be improved.
Bermejo et al.18 also found that with a cut-off score of 21/22, the sensitivity of the version of the MMSE with the «serial sevens» item was 1.0. If this result is accurate, a cut-off score of 24 or lower would be expected to diminish the specificity of this test without increasing its sensitivity; this would therefore decrease its positive predictive value. In the same study18 the ideal cut-off for the MEC was set at 25/26, which yielded a sensitivity of 1.0 and a specificity of 0.84. Thus the overall effects of the MEC are the opposite of those of the MMSE: if the cut-off score is 24 or lower, sensitivity is reduced somewhat and specificity is increased. This affects the agreement between tests: with the cut-off score suggested by Bermejo et al., agreement between the tests according to table 1 would increase significantly to 0.675.
Limitations of the study
One of the limitations of our study is that we gave the two tests simultaneously. This lengthens the time needed to administer them, and some patients may have become tired, especially when asked questions that required more concentration. However, this has been a relatively common practice in a number of studies, and the fact that most items overlapped exactly in the two tests and were thus presented only once reduced the total time needed, and hence minimized the effects of this factor. Another source of bias may have been the large number of researchers and interobserver variability, although we tried to minimize this by training all participating researchers in the administration of the MMSE and the MEC. In addition, we excluded from the study all test results that were complete or incorrectly recorded.
On the other hand, we consider the fact that the patient´s regular physician or nurse administered the tests personally an additional advantage which may have contributed toward a favorable interview climate. In addition, this provided information on the effectiveness of these screening instruments under conditions that approximated those of actual clinical practice. The present study can therefore be considered an analysis of agreement applied to the actual primary care setting.
Practical applicability
Although age and educational level are known to influence the results of both tests,19-21 the MMSE appeared to be more sensitive to the influence of these variables in the present study. However, as noted above, this study did not set out to evaluate the diagnostic efficacy of the instruments, but only to discover to what extent their results were in agreement.
We conclude that in a large sample of patients served by primary care centers in Catalonia, and under conditions of actual clinical practice, the MMSE and the MEC detected very different prevalences of suspected cognitive impairment when a cut-off score of 24/23 was used. The classical versions of these tests therefore do not appear to be interchangeable for screening for cognitive impairment, especially in subjects with a low educational level or those older than 80 years. Scores higher than 24 points are unlikely to rule out the absence of cognitive impairment reliably.
Changing the cut-off scores for both tests can improve their agreement. In the light of these findings, and because of the good intraclass correlation coefficient between the MMSE and the MEC, a change in the cut-off score for both tests seems necessary to improve their agreement in practice. When the classical cut-off of 24/23 points is used for the MEC, the best agreement with the MMSE is obtained with a cut-off score for this test of 20/19.
Correspondence: Ernest Vinyoles. Centro de Atención Primaria La Mina. C/ Mar, s/n. 08930 Sant Adrià de Besòs, Barcelona, Spain. E-mail: 23561evb@comb.es
This study was financed in part by the Fundació Marató de TV3 (Project 1019/07).
A shortened version of this paper was awarded the Spanish Society of Family and Community Medicine Prize at the Twentieth Congress of the Spanish Society of Family and Community Medicine in Gijón, November 2000.
Researchers participating in the Cuida´l Project
ABS Badalona 4 (J. Forcada, A. Llibre, E. Borlan, M. Llorens y A. Martínez); ABS Badalona 5 (I. Oliva, M.M. Domingo, S. Mas, M.L. García, C. Palazuelo, C. Piñol, M. Puche, J. Llussá y S. Zamora); ABS Badalona 6 (C. Seco, A. Díaz, J. Fariña, V. Roger, N. Puig, P. Escobedo, A. Robles, A. Girona, M.J. Toribio, P. Laporta, C. Batlle, T. Rama, F. García-Faria, M. Brugada, I. López, R. Cabello, E. Galindo, C. Toran, M.J. Ulldemolins, C. Albaladejo, E. Gejo, A. Martín, M. Castaño, P. Beato, S. Mateu y G. Pizarro); ABS Badalona 7 La Salut (J. Milozzi, M. Ruiz, J. Teruel, M. Giné, I. Barrio, J. Comín, M. Murt, M. Sánchez, A. Muñoz, A. Utgés y S. Gutiérrez); ABS Badia del Vallès (C. Yuste, P. Torres, M. Montasell, R. Azagra, M. Fuentes, J.F. Doz, Q. Figueras, L. Mengual, C. Lluma, G. Gasulla, L. Mayordomo, P. Roura, E. Gutiérrez, M. Iglesias, M. Ruiz, J.M. Bonet, D. García, F. Sole, F. Tarrago, J. Llonch y M. Pons); ABS Raval Sud (D. García, M.V. Pitarch, P. Escobar, L. Ibáñez, M. Ferrán, J. Casas, B. Casabella, R. Ruiz, J. Pertíñez, A. Hervas, M. Sánchez y M. Canet); ABS Trinitat Nova (N. Castells, C. Munar, M. Estruch, J. Ametlla, A. Roig, X. Flor, C. González, M. Mas, L. Sánchez, J. Guerrero, A. Buendía, M. Delgado, M.J. Pujol, J. Garbayo, D. Pérez, R. Melió, M.M. Fraga y N. Castells); ABS Barcelona 9-D (M. Godall, J.M. Carpio, A. Moretó, A. Díez, A. Rosas, E. González y M.C. Mateu); ABS Barcelona 9-E (L. Llosà, D. Granés, R. Espona, M.C. del Olmo, A. Cano, A. López, A. Alario, F. López, F. Mateos, M.C. García, J.J. Rodríguez, M. Mayorga, S. Martínez y N. Matilla); ABS Barcelona 9-F (J. Juvanteny, I. Angulo, I. Feijoo, I. Giner, A. Broto, J. Galindo, G. Planas, M. Barrachina, A. Aymar, N. Aramendia y M.A. Fuertes); ABS Barcelona 9-G (M. Roura, C. Font, T. Cervelló, C. Ramon, X. Corpas, V. Miralles, E. Olivé y J.L. Losada); ABS Besalú (C. Pou, I. Fernández, C. Pérez, R. Guixà, P. Zacarias y E. Bayona); ABS Capellades (A. Brugués, P. de Millan, P. Salat, J. Martí, I. Colomer, A. Garriga, X. Solé y M. Garriga); ABS Castelldefels (M. González, C. Moliner, J.C. Contel, P. Reig, J. Gené, A. Baulies y J. Gil); ABS Cornellà-La Gavarra (J. Martorell, C. Padin, F. Borrell, R. López, S. Espluga, E. Florensa, O. Moreno, C. Bayona, C. Martí y A.M. Aceituno); ABS Cornellà 2 (E. Sánchez, M. Lacoste, I. Montaner, O. Ortiz, A. Jurado, M.E. Galán, J. Pacet, M.I. Martín y C. Busquier); ABS Cornellà 4 (J. Toll, M. Rodríguez, M. Server, H. Pi, P. Barreto, M. Porta, V. López, L. Ribas, L. Pérez y C. Muñoz); ABS El Prat 3 (C. Batalla, T. Graell, A. Ezpeleta, F. González, E. Comín, M. Miñano, E. López, A. Alfonso, A. Cuenca, O. Maceres y J. Riba); ABS Esplugues 1 (T. Julia, I. Porta, C. Mateo, C. Romero, M. Varona, I. Monte, T. Cabases, F. Alguacil, P. Monge, J. Rodríguez, P. Forgas, M.J. Cerain y M. Cardona); ABS Esplugues 2 (A. Serra, C. Torró, A. Morales, M. Llagostera, P. Wemberg, M. Arriola, D. Marginet, P. Pérez, D. Tornos, J. Ventura, C. Truque y E. Bleda); ABS Garraf-Rural (A. Pérez, J.M. Benet, J.C. Caballero, P. Sabaté, J. Hernández, E. Cuesta, P. Torrecilla, B. Federio, J.R. Garcia, P. Foz, M. Duran, R. Saez, R. Cañizares y X. Castro); ABS Gavà 2 (C. Almirall, A.M. Oliveira, E. Caramés, C. Galera, I. García, T. Vintró, A. Espín, L. Gonzalo, M. Soler, D. Benítez y E. Linares); ABS Girona-1 (C. Bou, M. Clot, C. Serra, M.A. Agüero, C. Sais, M. Salvans, A. Massaguer, M.C. Asensio, S. García, J.M. García, P. López, F. Carulla, P. Rigall, M. Collantes, E. Calvet, N. de Puig, M.A. Agüero, J. Portas, R. Sánchez, M.R. Carbó, M.A. Hereu y M. Martínez); ABS Igualada-Urbà (M. Ortínez, C. Espinós, D. Basas, C. Riera, M. Vilarrubias, T. Higuera, J. Zambudio, N. Solà, P. Fusté, C. Castelló, R. Chinarro y M. Canals); ABS L'Hospitalet-Centre (A. Ribas, R. Carrasco, M. Boada, J. Solé, R. Canal, D. Pérez, C. Morató, F.J. Millet, A. Traite, M.J. Megido, S. Milian, S. Coppeti, V. Sahonero, E. Juncadella, N. Maymó, J.M. Fandos, M. García, N. Fernández, M. Martos, E. Rodero, C. Mateos, E. Serra, M. Murcia y T. Rubio); ABS L'Hospitalet-Gornal (M. Hernández, A. Siurana, X. Alba, C. Santiago, G. Fanlo, C. Cortina, J. Mercader, C. Blanco y F. Benavente); ABS L'Hospitalet-Sant Josep (C. Lafuente, A.M. Lafuente, S. Alia, J. Vilaseca, P. Garcés, M.A. Méndez, L. Sandé, A. Fuentesauco, A.M. Gil, V. Cabré, M. Bielsa, A. Gaitano, J. Mena, A.M. de las Mestas y M. Rico); ABS L'Hospitalet-Santa Eulàlia (N. Borrell, C. Añaños, I. Sánchez, T. Meix, A. Evangelio, F. Torralba, S. Berlanga, A. Sanz, X. Mas, M.M. Forés, R. Viñas, J.A. Hernández, I. Zamora, D. Riera y M.L. Tarrida); ABS L'Hospitalet-Pubilla Cases (A. Planas, J.M. Veciana, E. Gavilán, F. Rodríguez, I. Vega, R. Tosquella, M. López, A. López, G. Sánchez, L. Velázquez, F. Segril y M. Martín); ABS La Jonquera (P. Pujol, C. Ruiz, Y. Massó, L. Boix, A. López, D. Pérez, J. Domènech, M. Bonet, M. Forès, X. Lecumberri, J. Isard, M. Pous y J.L. Yecora); ABS Lleida 4 (R. Sánchez, X. Alcalde, P. Navarro, E. Domínguez, L. Marco, M. Martínez, P. Santafe, T. Oliver y D. Ferrer); ABS Manlleu (E. Castell, A. Costa, J. Fontarnau, J. Sierra, J. Deniel, E. Casellas, M. Vilamú, A. García, S. Suriñach, A. Llagostera, V. Canal, D. Casadesús y C. Olmedo); ABS Martorell (L. Esteve, F. López, F. García, T. Badia, F. de Cabo, J. Peligro, C. Herráez, T. Alonso, C. Baiget, A. Oliete, L. Pérez, M. Fuentes, I. Verges, E. Pérez, M. Moreno, L. Oliveras, M. Canals, C. Rovira y C. Luna); ABS Penedès-Rural (A. Cererols, J. Llach, J. Flórez, M. Elias, P. Piñeiro, M. Costa y R. Manuel); ABS Piera (J. Solanellas, R. Torremorell, H. Cortés, J.D. Guevara, S. Caballero, R. Ribas, S. Marcelo, N. Carré y A. Lloses); ABS Roses (F. García, T. Bosch, P. Morcillo y P. Viedma); ABS Sant Adrià 1 (C. Ferré, C. Valladares, A. Plaza, C. Roser, M. Portes, E. Dura, M.J. Lorente, M. Lladó, R. Caro, M.A. Rocabayera y L. Vilalta); ABS Sils-Vidreres-Maçanet (A. Teixidor, M.C. Fondon, C. Pons, A. Sanchís y M. Boldú); ABS La Mina (R. Ciurana, L. Alejandro, C. Espel, M. Vilà, M. Mata, I. Bobé, J. Davins, A. Sáez, M. de la Figuera, A. Salvadó, C. Pareja, F. Soriano, E. Vinyoles, C. Royo, J.M. Mendive, E. Zabaleta, C. de Juan, M. Castillo, R. Centelles, J. Rengel, S. Calvet, J. Agudo, A. Ramos y M. Canals); ABS Sant. Boi De Llobregat 2 (M. Muñoz, A. Rourera, C. Alvarado, A. Fernández, C. Espelt, M.J. Gracia, M. Via, M. Dordal, E. Steiner, R. Rodrigo, J. Alegre y E. Conesa); ABS Sant Boi De Llobregat 3 (C. Tamayo, S. González, A. Espinola, T. Arnau, A.R. Hernández, R.M. Marcos, A. Val, R. Giner, C. Barrio, C. Rubio, F. de la Torre, C. Gorrindo, I. Vázquez y M.R. García); ABS Sant Feliu De Guíxols (R. Herrero, T. Planas, P. Carreras, J. Rovira, L. Cinos, M. Muñoz, D. Torres, C. Xargay, C. Comas, M.A. Oliveras, J. Lafont y M. Félez); ABS Sant Just Desvern (J. Muniesa, N. Aresté, X. Serra, R. Rabaneda, L. Morató, D. Ruenz, A. Wilke, L. Crespo, F. Ridao, S. Granollers y C. Marcos); ABS Santa Coloma de Gramanet 1 (T. Morató, A. Muñoz, M.M. Ansaldo, M. Tramuns, I. López, M. Fuentes, J. Vidal, A. Vidal, M. Roset, E. Sabaté, M.J. Polo, A. Vilanova, A. Sancho, E. Corral, A. Taboada, T. Sala, P. Rodríguez, D. Molina y E. Martínez); ABS Santa Coloma de Gramanet 4 (R. de León, C. García, R. Forés, A. Gallart, C. Vela, R. Escolar, M. Alzamora, A. Fuentes, B. López, M. Puente, R. González, R. Ferrero, M. Sorribes, F. Margarit y M. Monsó); ABS Santa Coloma de Gramanet 6 (M.J. Martínez, J. Hernández, M. Pozo, O. Martínez, C. Lisicic, C. Aguilera, X. Dauder, M.M. Isnard y D. Olmos); ABS Santa Eugènia De Berga (A. Ribas, J. Verdera, A. Planes, J. Oliva, C. Blay, M. Molas, R.M. Salla, D. Rovira, A. Puente, H. Algilaga, T. Iruela, L. Vila, J. Espinàs, E. Caballé y E. García); ABS Tarragona-1 (N. Sarrà, M. Fortín, M. Pollcarpo, M. Henrich, P. Camós, M. Romera, J.M. Roca, J. Monteverde, R. Tigell y M. Juncosa); ABS Tarragona-2 (N. Saun, C.M. Fuentes, B. Rull, E. Satué, R. Canals, M. Barrera, E. Valdivieso y A. Veiga); ABS Terrassa C-Can Parellada (A. Sánchez, R. Camps, A. Casasayas, A. Navarro, O. Grima y M. Nozal); ABS Tortosa Est (J.I. Viloria, J. Clua, M.J. Arasa, J.F. Monclús, J.M. Basart, F. Vallespí, G. García, E. Ciurana, A. Casanova, T. Rupérez, E. Ibáñez, C. Mangrané, E. Gómez, R. Arasa, S. Ponce, N. Beguer y X. Bautista); ABS Vallirana (J. Creixell, E. Castro, C. Càmara, P. Miret, A. Izquierdo, J. Merin, J.M. Olmo, M. Sabaté, R. Llaurador, C. Pujol, A. Balibrea, C. Pérez, N. Casamada, S. González, J. Mata, S. San y V. Bardají); ABS Viladecans 2 (D. del Pino, P. Simonet, A. Padilla, A. Viniegra, E. Rillo, R. Villafafila, C. Lecumberri, C. Verduras, M.A. Fernández, C. Bentue, M.V. Vico, D. Ruiz, P. Figuera, A. García y D. Mora); ABS Vilafranca Urbana (M.L. Gardeñes, M. Ballester, D. Ferrer, P. Utrilla, R. Manuel, B. Coscollar, R. Rodrigo, R. Marchan, M. Giralt, M. Carrascosa, A. Robledo, J.A. Domínguez y B.M. Dinares); ABS Vilanova 1 (I. Garro, C. Casamayor, M. Navarro, O. Fuster, M. Briva, C. Batet, G. Mendoza, L. Gimeno, P. García y M.A. March).