To evaluate the effectiveness of two types of intervention in reducing antibiotic prescribing in respiratory tract infections (RTI).
DesignBefore–after audit-based study.
SettingPrimary Care centres in Spain.
ParticipantsGeneral practitioners (GPs) registered all patients with RTIs for 15 days in winter 2008 (pre-intervention), and again in winter 2009 (post-intervention).
InterventionsIntervention activities included meetings, with the presentation and discussion of the results, and several training meetings on RTI guidelines, information brochures for patients, workshops on point-of-care tests – rapid antigen detection tests and C-reactive protein rapid test – and provision of these tests in the clinic. All GPs, with the exception of those in Catalonia, made up the full intervention group (FIG); conversely, Catalan doctors underwent the same intervention, except for the workshop on rapid tests (partial intervention group, PIG). Multilevel logistic regression was performed taking the prescription of antibiotics as the dependent variable.
ResultsOut of a total of 309 GPs involved in the first register, 281 completed the intervention and the second register (90.9%), of which 210 were assigned to the FIG, and 71 to the PIG. The odds ratio of antibiotic prescribing after the intervention was 0.99 (95% CI: 0.89–1.10) among GPs assigned to PIG, and 0.50 (95% CI: 0.44–0.57, p<0.001) among those who were allocated to FIG. The reduction in antibiotic prescribing in FIG was more marked in flu infection, common cold, acute pharyngitis, acute tonsillitis, and acute bronchitis.
ConclusionsActive participation of GPs with the performance of point-of-care tests in the clinic is accompanied by a drastic reduction of antibiotic use in RTIs, primarily in infections considered as mainly viral.
Evaluar la efectividad de dos tipos de intervención en la prescripción antibiótica en infecciones del tracto respiratorio (ITR).
DiseñoEstudio antes-después basado en audit.
EmplazamientoCentros de atención primaria de España.
ParticipantesMédicos de familia registraron durante 15 días en invierno 2008 todas las ITR (preintervención), que se repitió en 2009 (postintervención).
IntervencionesSe realizaron reuniones con presentación y discusión de resultados, sesiones de formación en guías de ITR, folletos informativos para pacientes, talleres en uso de pruebas rápidas (Strep A y proteína C reactiva) y su provisión en las consultas. Los médicos participantes a excepción de Cataluña realizaron la intervención completa (IC), mientras que los médicos de Cataluña realizaron lo mismo menos el taller de pruebas rápidas (intervención parcial [IP]). Se efectuó análisis de regresión logística multinivel considerando como variable dependiente la prescripción antibiótica.
ResultadosDe los 309 médicos que realizaron el primer registro, 281 completaron la intervención y el segundo registro (90,9%), de los cuales 210 se asignaron a IC y 71 a IP. La odds ratio de prescripción antibiótica después de la intervención fue de 0.99 (IC95%: 0,89–1,10) entre los médicos asignados a IP, mientras que el observado en la IC fue de 0.50 (IC95%: 0,44–0,57, p<0,001). La mayor reducción de prescripción antibiótica en IC se observó en gripe, catarro común, faringitis aguda, amigdalitis aguda y bronquitis aguda.
ConclusionesLa participación activa de los médicos con uso de pruebas rápidas en la consulta se acompaña de una reducción importante de antibióticos en las ITR, sobre todo en las infecciones mayoritariamente virales.
A third of primary care consultations are due to an infectious disease and more than half are caused by a respiratory tract infection.1 Inappropriate use of antimicrobials for these infections is associated with increased risk of adverse drug events and higher overall health care costs.2,3 Data from 26 European countries demonstrated a correlation between the use of antibiotics and the level of antibiotic resistance.4 The danger of increasing antibiotic resistance has been recognised globally, resulting in extensive campaigns aimed at both prescribers and the public and in the development of treatment guidelines.5
Attempts to reduce unnecessary antibiotic use have had mixed results. A combination of patient and physician education has been shown to help reduce antibiotic overuse for a variety of acute respiratory tract infections,6 but levels of improvement have been limited, on average, to less than 20% absolute reduction across the study populations of physicians.7–10
The Happy Audit project has been a study financed by the European Commission, the main objective of which was to strengthen the surveillance of respiratory tract infections in primary healthcare through the development of intervention programmes targeting general practitioners (GP) and changing people's habits towards prudent use of antimicrobial agents.11 GPs from six countries have participated in this study (Denmark, Sweden, Lithuania, Russia, Spain and Argentina). However, Spain was the only country in which two types of interventions were undertaken. We present in this final paper the overall results of the study in Spain [with the participation of semFYC] aimed at evaluating the effect of two types of interventions on antibiotic prescribing in respiratory tract infections.
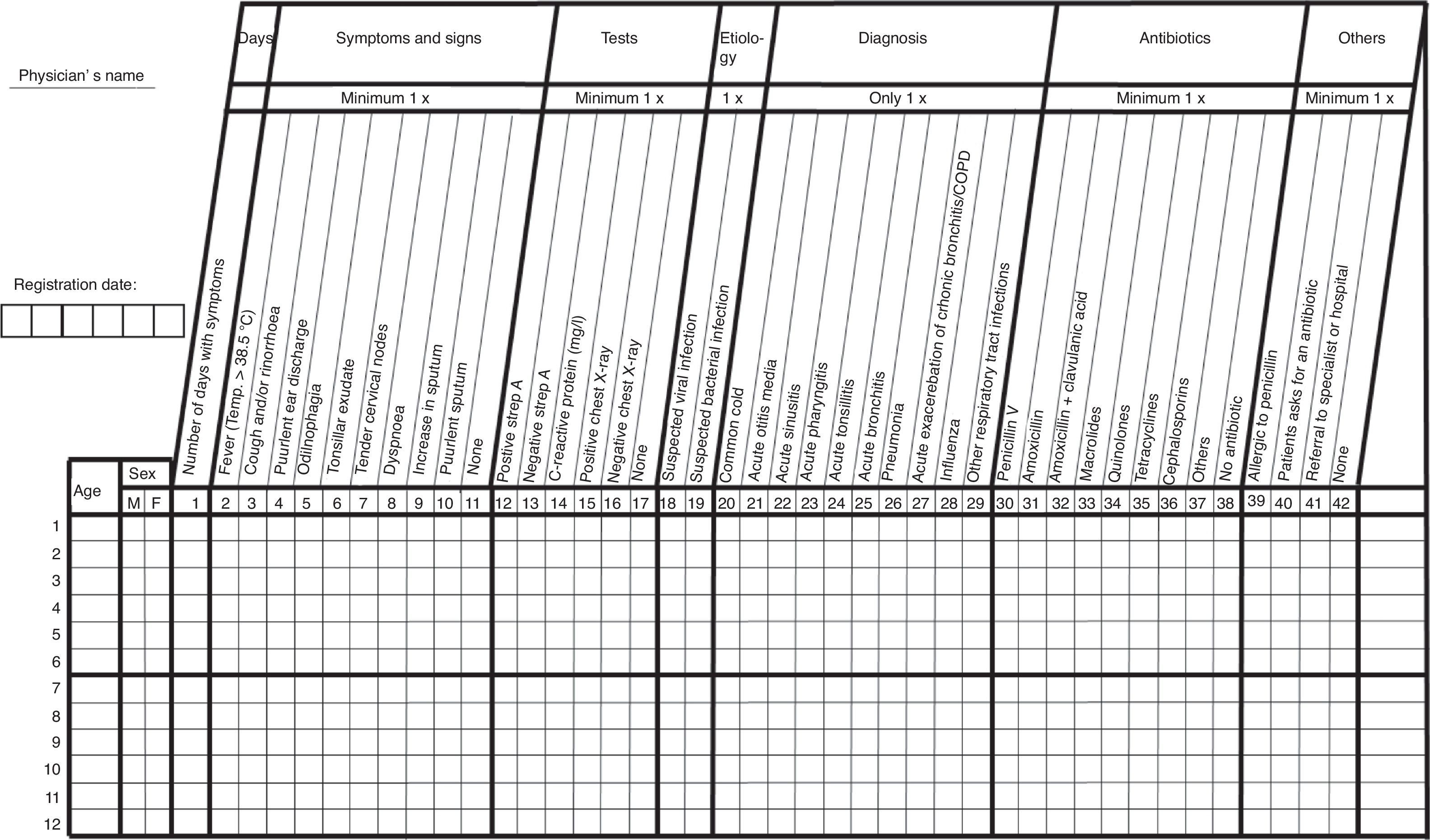
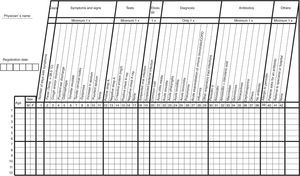
Materials and methodsThis is a before–after quality assurance study carried out in primary care with family physicians in nine Autonomous Communities in Spain. Detailed information about the study method and the intervention were previously published in the study protocol.11 Briefly, the data were registered according to the methodology of the Audit Project Odense described by Munck et al.,12 which follows a prospective self-registration methodology in which a simple reporting sheet was used. Approval was obtained from the Ethical Committee Board Fundació Jordi Gol i Gurina (Barcelona, Spain; registration number: 44154). All participants were instructed to fill out a template with all respiratory tract infections during a 3-week period in the winter months of 2008 (preintervention). On this sheet, the physician attending the patient noted different specific parameters of medical care, including the age and sex of the patient, the number of days of symptoms, presenting signs (fever, coughing, otorrhoea, odynophagia, tonsillar exudates, tender cervical glands, dyspnoea, increase in sputum volume, purulence of sputum), diagnosis (common cold, otitis media, pharyngitis, tonsillitis, influenza, acute bronchitis, acute exacerbation of chronic bronchitis or chronic obstructive pulmonary disease, pneumonia), aetiological suspicion (viral or bacterial), performance of chest radiograph and point-of-care tests – rapid antigen detection tests for detecting group A β-haemolytic streptococcus antigen and C-reactive protein rapid test in capillary blood, antibiotic treatment or not, allergy or not to penicillin, and whether the patient requested an antibiotic and referral to another healthcare setting (Fig. 1).
With the overall and individual results intervention activities were conducted including meetings with presentation and discussion of results and several training meetings on respiratory tract infections guidelines, information brochures for patients, workshops on point-of-care tests and provision of these rapid tests in the consultation. The point-of-care tests were specifically bought for this study and were provided free to the participants. All GPs participating in the study with the exception of Catalonia carried out the full intervention group; conversely, Catalan doctors underwent the same intervention excepted for the workshop on rapid tests and point-of-care tests were not provided (partial intervention group). The same registry was repeated in early 2009 (postintervention).
The data were analysed with the Stata v.11 statistical program. Bivariate analysis was carried out with the use of chi square tests for comparing categorical variables. For the calculation of the odds ratio of antibiotic prescribing after the intervention a multilevel logistic regression analysis was estimated with two levels: patients and GPs. Antibiotic prescription was considered as the dependent variable (yes/no). The model was also adjusted for covariables age, gender, signs and symptoms of patients, referral, demand of antibiotics and age, gender, and burden of GPs. Statistical significance was considered with p<0.05.
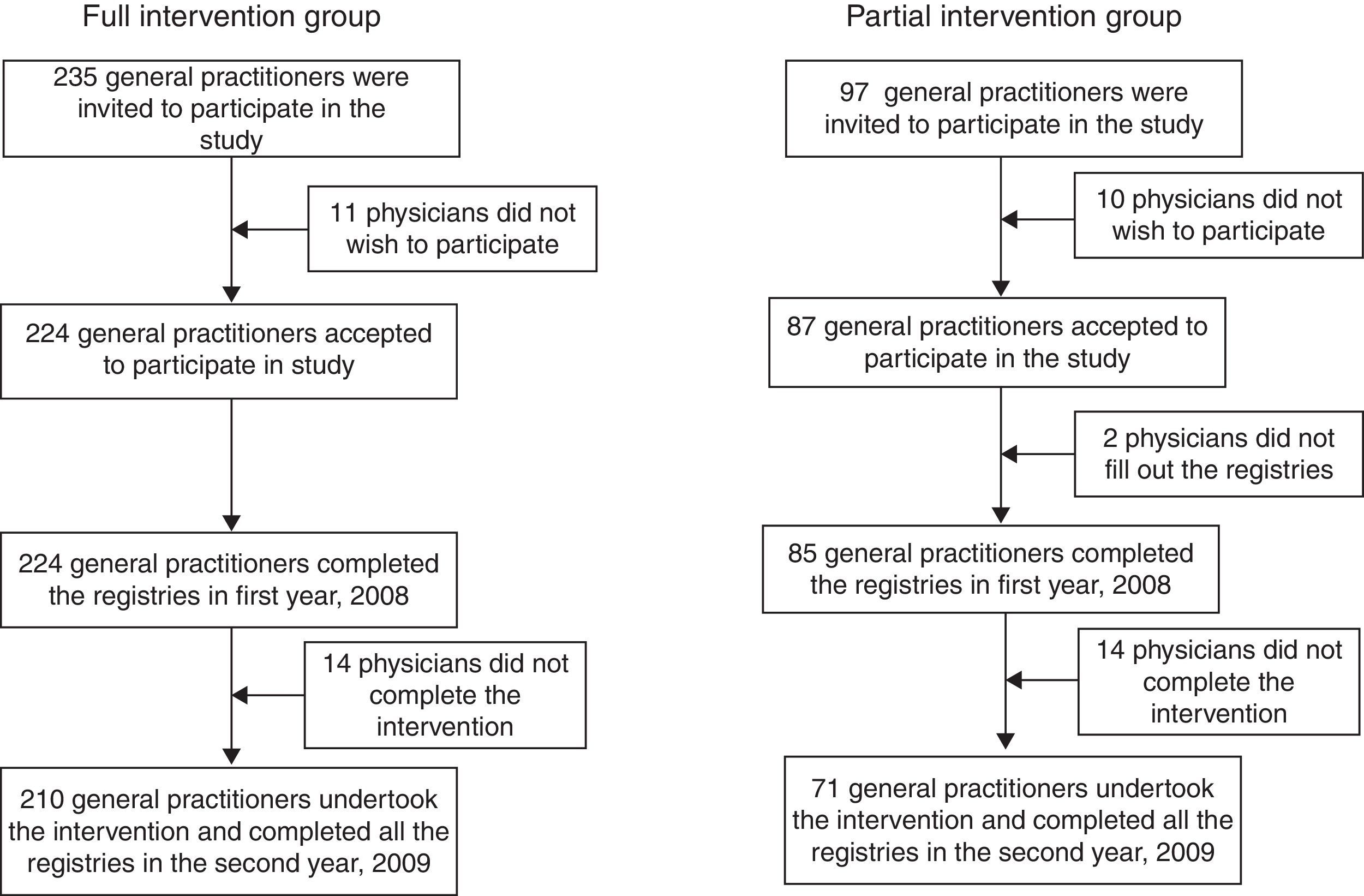
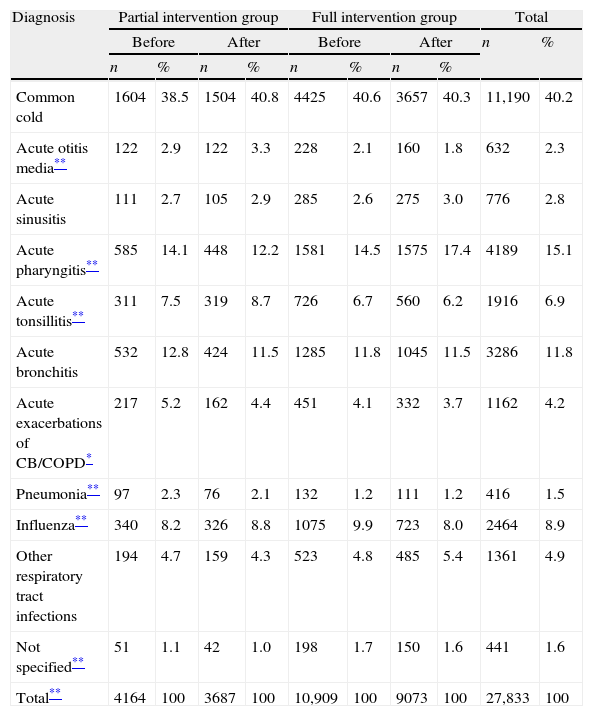
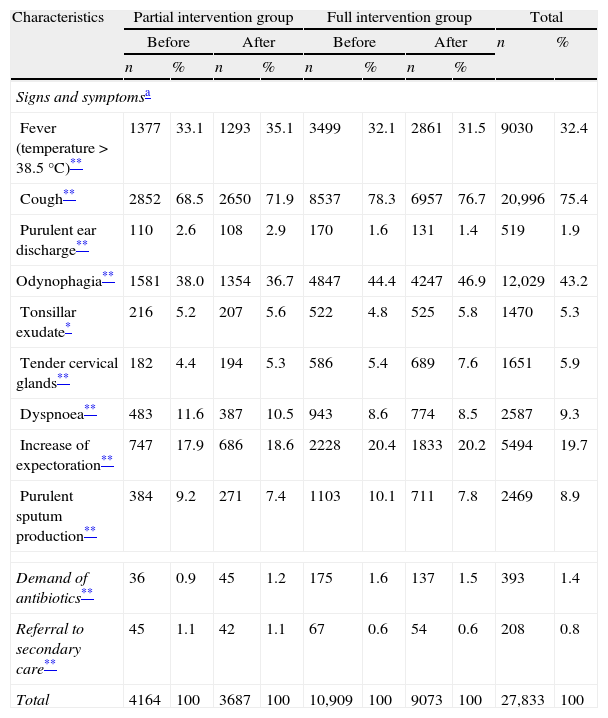
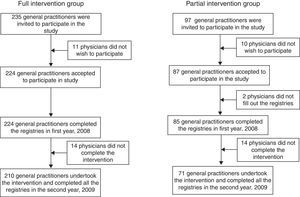
ResultsA total of 332 GPs were invited to participate in this study but 21 declined. Out of a total of 309 primary care physicians who performed the first registry in 2008, 281 completed the intervention and the second registry (90.9%), of which 210 were assigned to the full intervention group (89.4% of the GPs who were invited to take part) and 71 to the partial intervention group (73.2% of the GPs invited). Fig. 2 describes the flow of the GPs throughout the study. A total of 15,073 respiratory tract infections were registered in the first registry while 12,760 were registered after the intervention. The most common infection was common cold, with 11,190 infections (40.2% of all cases), followed by pharyngitis with 4189 cases (15.1%) and acute bronchitis with 3286 infections in total (11.8%) (Table 1). As shown in Table 2 the sign most frequently reported by GPs was cough, present in 20,996 contacts in both years (75.4%), followed by odynophagia (12,029 cases; 43.2%), fever (9030 cases; 32.4%) and increase of expectoration (5494 episodes; 19.7%).
Number of infections registered by the 281 GPs who completed the two registries, before and after the intervention, depending on the diagnoses.
| Diagnosis | Partial intervention group | Full intervention group | Total | |||||||
| Before | After | Before | After | n | % | |||||
| n | % | n | % | n | % | n | % | |||
| Common cold | 1604 | 38.5 | 1504 | 40.8 | 4425 | 40.6 | 3657 | 40.3 | 11,190 | 40.2 |
| Acute otitis media** | 122 | 2.9 | 122 | 3.3 | 228 | 2.1 | 160 | 1.8 | 632 | 2.3 |
| Acute sinusitis | 111 | 2.7 | 105 | 2.9 | 285 | 2.6 | 275 | 3.0 | 776 | 2.8 |
| Acute pharyngitis** | 585 | 14.1 | 448 | 12.2 | 1581 | 14.5 | 1575 | 17.4 | 4189 | 15.1 |
| Acute tonsillitis** | 311 | 7.5 | 319 | 8.7 | 726 | 6.7 | 560 | 6.2 | 1916 | 6.9 |
| Acute bronchitis | 532 | 12.8 | 424 | 11.5 | 1285 | 11.8 | 1045 | 11.5 | 3286 | 11.8 |
| Acute exacerbations of CB/COPD* | 217 | 5.2 | 162 | 4.4 | 451 | 4.1 | 332 | 3.7 | 1162 | 4.2 |
| Pneumonia** | 97 | 2.3 | 76 | 2.1 | 132 | 1.2 | 111 | 1.2 | 416 | 1.5 |
| Influenza** | 340 | 8.2 | 326 | 8.8 | 1075 | 9.9 | 723 | 8.0 | 2464 | 8.9 |
| Other respiratory tract infections | 194 | 4.7 | 159 | 4.3 | 523 | 4.8 | 485 | 5.4 | 1361 | 4.9 |
| Not specified** | 51 | 1.1 | 42 | 1.0 | 198 | 1.7 | 150 | 1.6 | 441 | 1.6 |
| Total** | 4164 | 100 | 3687 | 100 | 10,909 | 100 | 9073 | 100 | 27,833 | 100 |
CB, chronic bronchitis; COPD, chronic obstructive pulmonary disease.
Items registered by the 281 GPs who completed both registries, before and after the intervention.
| Characteristics | Partial intervention group | Full intervention group | Total | |||||||
| Before | After | Before | After | n | % | |||||
| n | % | n | % | n | % | n | % | |||
| Signs and symptomsa | ||||||||||
| Fever (temperature>38.5°C)** | 1377 | 33.1 | 1293 | 35.1 | 3499 | 32.1 | 2861 | 31.5 | 9030 | 32.4 |
| Cough** | 2852 | 68.5 | 2650 | 71.9 | 8537 | 78.3 | 6957 | 76.7 | 20,996 | 75.4 |
| Purulent ear discharge** | 110 | 2.6 | 108 | 2.9 | 170 | 1.6 | 131 | 1.4 | 519 | 1.9 |
| Odynophagia** | 1581 | 38.0 | 1354 | 36.7 | 4847 | 44.4 | 4247 | 46.9 | 12,029 | 43.2 |
| Tonsillar exudate* | 216 | 5.2 | 207 | 5.6 | 522 | 4.8 | 525 | 5.8 | 1470 | 5.3 |
| Tender cervical glands** | 182 | 4.4 | 194 | 5.3 | 586 | 5.4 | 689 | 7.6 | 1651 | 5.9 |
| Dyspnoea** | 483 | 11.6 | 387 | 10.5 | 943 | 8.6 | 774 | 8.5 | 2587 | 9.3 |
| Increase of expectoration** | 747 | 17.9 | 686 | 18.6 | 2228 | 20.4 | 1833 | 20.2 | 5494 | 19.7 |
| Purulent sputum production** | 384 | 9.2 | 271 | 7.4 | 1103 | 10.1 | 711 | 7.8 | 2469 | 8.9 |
| Demand of antibiotics** | 36 | 0.9 | 45 | 1.2 | 175 | 1.6 | 137 | 1.5 | 393 | 1.4 |
| Referral to secondary care** | 45 | 1.1 | 42 | 1.1 | 67 | 0.6 | 54 | 0.6 | 208 | 0.8 |
| Total | 4164 | 100 | 3687 | 100 | 10,909 | 100 | 9073 | 100 | 27,833 | 100 |
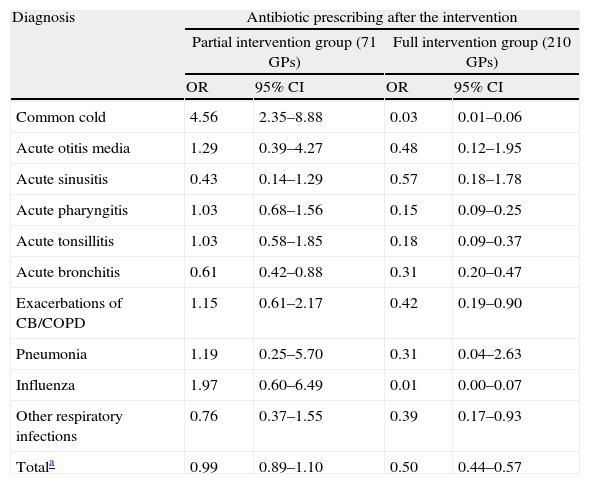
Antibiotics were prescribed in 4178 patients with respiratory tract infections in the first year (27.7%; 95% CI: 27–28.4%). The diagnoses in which antibiotics were most likely to be prescribed by the 281 GPs of the first registry were pneumonia (89.5% of antibiotic prescribing), acute otitis media (88.6%), acute tonsillitis (88.4%), acute sinusitis (87.4%), and exacerbations of chronic bronchitis or chronic obstructive pulmonary disease (81.9%). The percentages observed for acute bronchitis, other respiratory tract infections, acute pharyngitis, influenza and common cold were 58.1%, 20.6%, 18.5%, 2.9%, and 2.5%, respectively. The odds ratio of antibiotic prescribing after the intervention was 0.99 (95% CI: 0.89–1.10) among physicians who undertook the partial intervention, without statistical differences being observed. However, the odds ratio was significantly lower only in acute bronchitis (0.61; 95% CI: 0.42–0.88). The odds ratio of antibiotic prescribing after the intervention was statistically lower among GPs assigned to the full intervention, with an odds ratio of 0.50 (0.44–0.57; p<0.001). This reduction was more marked in flu infection (0.01; 95% CI: 0–0.07), common cold (0.03; 95% CI: 0.01–0.06), acute pharyngitis (0.15; 95% CI: 0.09–0.25), acute tonsillitis (0.18; 95% CI: 0.09–0.37), and acute bronchitis (0.31; 95% CI: 0.20–0.47) (Table 3).
Antibiotics prescribed before the intervention and odds ratio of antibiotic prescribing after the intervention depending on the group assigned.
| Diagnosis | Antibiotic prescribing after the intervention | |||
| Partial intervention group (71 GPs) | Full intervention group (210 GPs) | |||
| OR | 95% CI | OR | 95% CI | |
| Common cold | 4.56 | 2.35–8.88 | 0.03 | 0.01–0.06 |
| Acute otitis media | 1.29 | 0.39–4.27 | 0.48 | 0.12–1.95 |
| Acute sinusitis | 0.43 | 0.14–1.29 | 0.57 | 0.18–1.78 |
| Acute pharyngitis | 1.03 | 0.68–1.56 | 0.15 | 0.09–0.25 |
| Acute tonsillitis | 1.03 | 0.58–1.85 | 0.18 | 0.09–0.37 |
| Acute bronchitis | 0.61 | 0.42–0.88 | 0.31 | 0.20–0.47 |
| Exacerbations of CB/COPD | 1.15 | 0.61–2.17 | 0.42 | 0.19–0.90 |
| Pneumonia | 1.19 | 0.25–5.70 | 0.31 | 0.04–2.63 |
| Influenza | 1.97 | 0.60–6.49 | 0.01 | 0.00–0.07 |
| Other respiratory infections | 0.76 | 0.37–1.55 | 0.39 | 0.17–0.93 |
| Totala | 0.99 | 0.89–1.10 | 0.50 | 0.44–0.57 |
OR, odds ratio; CI, confidence interval; GP, general practitioner; CB, chronic bronchitis; COPD, chronic obstructive pulmonary disease.
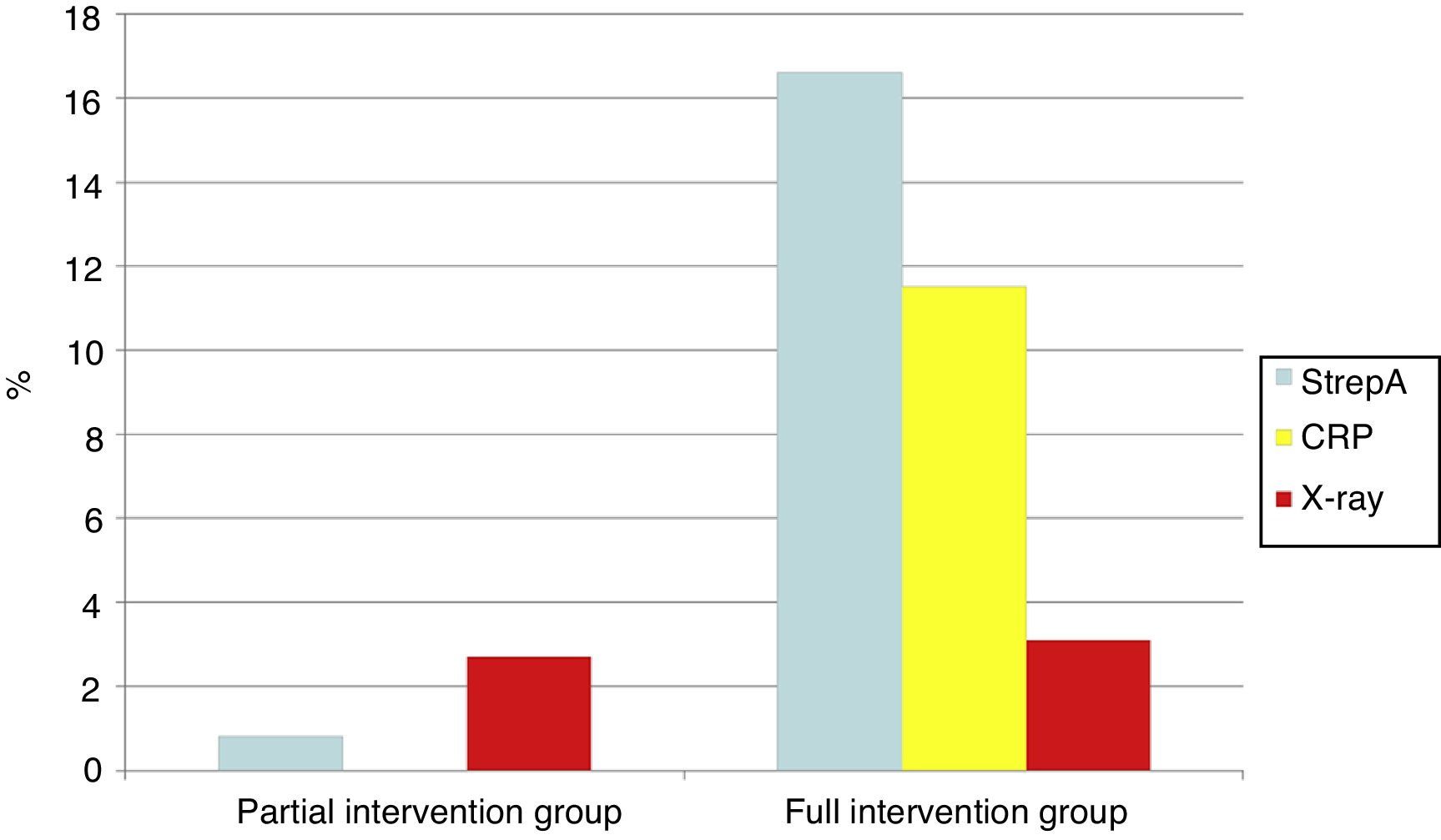
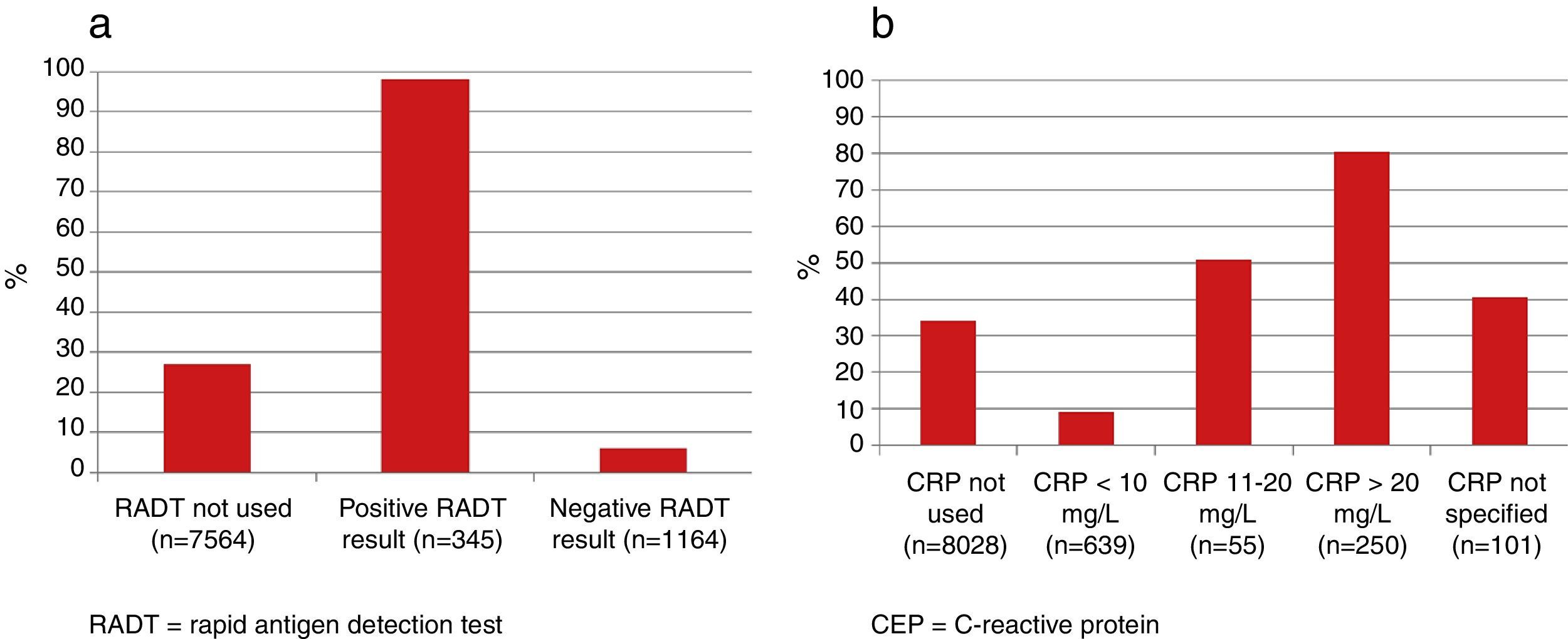
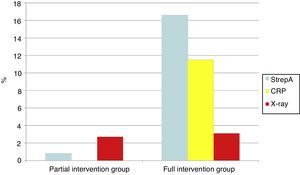
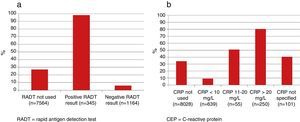
The use of diagnostic tests after the intervention was higher among GPs assigned to the full intervention group, except for the request of an X-ray test. Before the intervention rapid antigen detection tests were performed in 76 cases and C-reactive protein testing only in 4 other cases. On the other hand, rapid antigen detection testing was carried out in 1509 cases (16.6% of all the patients) and CRP was performed in 1045 patients (11.5%) in the second registry (Fig. 3). As shown in Fig. 4, GPs assigned to the full intervention using both rapid antigen detection tests and C-reactive protein were less likely to prescribe antibiotics than their counterparts who did not use them. Antigen detection testing was used in 1499 patients with a result being positive in 345 cases (22.6%). Antibiotics were prescribed in 338 cases of positive test results (98%) but only in 69 individuals out of the 1164 negative test results (5.9%). Similarly, antibiotics were mainly withheld when the CRP value was lower than 10mg/L; however, they were prescribed in more than half of the cases with CRP values over 10mg/L.
A growing literature on strategies to reduce the overuse of antibiotics demonstrates that multifaceted interventions tend to be the most successful.10,13 The results of our study suggest that efforts to reduce antibiotic prescribing may be more effective if GPs intervene actively in the clinical encounter by means of carrying out the point-of-care provided.
This study has some limitations. This study was not a clinical trial and neither the groups were assigned randomly, which may be considered the main limitation of the study. Clinical outcomes of the patients recruited were not taken into account and thus, it is not known whether the percentage of clinical failure or incidence of complications differed between the groups. Nonetheless, the registry sheet included the referral of patients to secondary care. In addition, several papers have not observed any differences in clinical outcomes between patients with respiratory tract infections who were treated with antibiotics and those who were not.14–16 Another limitation that should be regarded in this type of study is that the mere fact of performing an audit may influence prescribing habits. However, the reliability of the Audit Project Odense methodology demonstrated in various projects carried out in other European countries is very high and is very well correlated with actual prescribing in medical offices.17 Nevertheless, the greatest strength of this study is the large number of physicians included, with the inclusion of 27,833 respiratory tract infections. The low drop-out rate observed in this study can be considered as another strength, since less than 10% of the professionals who carried out the first registry left the study. Another strength of this project is inherent in the reality of our country in which point-of-care tests were not incorporated into primary care by the time this study was carried out and, therefore, the effect of their use could be better established.
Many studies have been performed to determine the effectiveness of different types of intervention in reducing the prescription of antibiotics. Not all interventions have achieved positive results particularly when used alone. According to the last review of the Cochrane Library, published in 2005, only interventions taking combinations including result feedback, interactive educational sessions and strategies aimed at patients, achieve a reduction in the prescription of antibiotics in supposedly viral respiratory infections.10 These most successful have focused on combined communication skills training with point-of-care testing and the use of interactive booklets during consultations with patients.18–21 The results of the Happy Audit study confirm these results, since only GPs assigned to the full intervention group significantly reduced the prescription of antibiotics. Van den Velden et al. also observed that those that achieved more reductions of antibiotic overuse were the use of C-reactive protein and the enhancement of communication skills.13 In our study, GPs using rapid tests were more likely to prescribe fewer antibiotics. As far as C-reactive protein is concerned, the physicians felt more confident not to prescribe antibiotics where the results were less than 10mg/L. A recent meta-analysis confirms these results.22 Similarly, negative rapid antigen detections tests were associated with only a 6% of antibiotic prescribing. Interventions that did not include the former are associated with contradictory results or achieve only modest outcomes.23 A meta-ethnographic assessment of different interventions concluded that it is important to allow GPs to reflect on their own prescribing, and to educate GPs about appropriate prescribing and the benefit of implementing it in practice, in order to enhance the acceptability of the interventions.24
In conclusion, this study demonstrates that an intervention consisting of the presentation and discussion of overall and individual results, meetings on guidelines on respiratory tract and information brochures for patients achieved modest reductions on the antibiotic prescribing for respiratory tract infections. When all these interventions were combined with physician's active participation in workshops on point-of-care tests and these tests were provided in the consultation, the reduction was more marked.
- •
Antibiotics are often overprescribed for respiratory tract infections.
- •
Multifaceted interventions have been shown to reduce antibiotic overuse for a variety of respiratory tract infections but levels of improvement are limited.
- •
We carried out this study aimed at knowing the effectiveness of two types of intervention on the antibiotic prescription in respiratory tract infections. The interventions only differed in the training and access to the use of a rapid antigen detection and C-reactive protein testing. Only the intervention that involved near-patient testing sorted the largest intervention effect.
This project is a Specific Targeted Research Project (STREP) funded by The European Commission: DG SANCO under the Frame Program 6 (SP5A-CT-2007-044154). Contract number 044154.
Conflicts of interestCL reports having a grant from the Fundació Jordi Gol i Gurina for a research stage at the University of Cardiff. He also reports receiving research grants from the European Commission (Sixth and Seventh Programme Frameworks), Catalan Society of Family Medicine, and Instituto de Salud Carlos III (Spanish Ministry of Health). The other authors have nothing to declare.
The authors want to acknowledge the advice given by Beatriz González López-Valcárcel for the multilevel logistic regression analysis. The physicians who participated in the Happy Audit study were: Andalusia: Juan de Dios Alcántara, Carolina Álvarez, Francisco Atienza, Manuel Baeza, Juan Bellón, Inmaculada Carrillo, César J. Costa, Pedro Crespo, Carmen Dastis, Salvador Domínguez, M. Magdalena Gálvez, M. Isabel González, Aurora Guerrero, Carmen Gutiérrez, Rosa del Pilar Herrera, Guillermo Largaespada, Beatriz López, Inés M. López, María Luisa Manzanares, Leonor Marín, Francisco Marmesat, M. Mercedes Martínez, Rocío Martínez, M. Inmaculada Mesa, Yolanda de Mesa, Guillermo M. Moreno, M. Luisa Moya, José Oropesa, Carolina Pérez, Manuel Pérez-Cerezal, Juan J. Quero, M. Pilar Rojo, Miguel Sagristá, Consuelo Sampedro, Jesús Carlos Sánchez, José Cristobal Sendín, Miguel Silva, José Miguel Solís, Laura Suárez, Irene Victoria de Tena, Salvador Torres. Asturias: Carmen Alonso, Fernando Álvarez, M. Etelvina Castañón, Beatriz Fernández, Guillermo García, M. Pilar Jimeno, Ramón Macía, Carmen Martín, Ernesto Martínez, Covadonga Monte, M. Amor Paredes, Javier Pérez, M. Mar Pizarro, Felipe J. Rodríguez, Celia Teresa Tamargo, Salvador Tranche, M. Raimunda Vázquez. Balearic Islands: Ester Adelantado, Antonio Ballester, Arnest Bordoy, Bernardino Bou, José Antonio Chumillas, Francisca Comas, Teresa Corredor, Consuelo Corrionero, Esther Domínguez, Alberto Eek, Teresa Estrades, Sebastián Fluxa, Maria E. Garau, Josefa García, Yolanda Garzón, M. José González-Bals, Rosa Grimalt, Antoni J. Jover, Catalina Llabrés, Magdalena Llinas, Marian Llorente, Montse Llort, Ana M. Macho, David Medina, Susana Munuera, Joana M. Oliver, Rosa Ortuño, Juana Pérez, Lourdes Quintana, María Martín-Rabadán, José Alfonso Ramón, Jaime Ripoll, José Ramón Roca, Raquel Ruano, M. Carmen Santos, Isabel M. Socias, M. Mar Sureda, Carolina Tomás. Canary Islands: Margarita Aguado, Pilar Aguilar, M. Carmen Artiles, Jonás de la Cruz Cabrera, M. Isabel Cardenes, Encarna Duque, José Luis Eguren, Javier Francés, Alicia González, Gloria Guerra, M. de las Huertas Llamas, Alicia Monzón, Aurelia Perdomo, Carlos Prieto, José Luis Rodríguez, M. Rafaela Sánchez, M. Teresa Simó, Lucía Tejera, José M. Toscano. Catalonia: Maite Aizpin, Francesc Arasa, Josep Ausensi, Teresa Aviñó, Àngel Ayala, Montse Balagué, Jaume Banqué, Jaume Baradad, Marta Beltrán, Josep Lluis Berdonces, Noemí Bermúdez, Armando Biendicho, Javier Blasco, Miriam Boira, Enric Buera, Joan Cabratosa, Sonia Castro, Mireia Cid, Maria de Ciurana, M. Rosa Dalmau, Carmen Delgado, Teresa Escartín, Rosario Espinosa, Gemma Estrada, Eugeni Fau, M. Emma Fava, Ester Fernández, María Ferré, Pilar Franco, Joaquim Franquesa, Elena Esther Fuentes, Carme García, Manuel García, Montse García, Sergi Giró, Mònica Gómez, Yosbel Guerra, Silvia Hernández, Francisco Ibáñez, Roland Juan, Josep Lluis Llor, Ana Luque, Anna Manzanares, Emili Marco, Judith Marin, Emma Marqués, Ignacio Martínez, Maribel Martínez, Rosa Martínez, Ariadna Mas, Cinta Monclús, Pau Montoya, M. Luisa Morató, Jesús V. Muniesa, Esther Mur, M. Assumpció Nadal, Elena Navarro, Miquel Navarro, Carme Pascual, Marina Payà, Almudena Pérez, Pilar Pérez, Cristina Pozo, Luis Quinzaños, Anna Ràfols, Mercè Ribot, Maria Riera, Pilar Rivera, Carolina Robado, Purificación Robles, M. José Roig, M. Carmen Ros, José Miguel Royo, M. Victoria Rubio, Anna Serra, M. Ángeles Sieira, Yaiza Sierra, Hiam Tarabishi, Silvia Torrent, Leticia Troyano, María Úbeda, Antonio Ubieto, Susana Vargas, Jordi Vilano, Assumpció Wilke. Galicia: Eduardo Alonso, Margarita Bayón, Alejandro Cardalda, Francisco Castrillo, Ángeles Charle, Marina Cid, Pilar Cobas, Peregrina Eiroa, Ana Fernández, Elena García, Ricardo Manuel Héctor, Susana Hernáiz, Jesús De Juan, Pilar Mendos, Elisa Mosquera, Concepción Nogueiras, Ana M. Ogando, Elías Puga, Adolfo Rodríguez, José Benito Rodríguez, Coro Sánchez, Joaquín San José, Santiago Santidrián, Luis Seoane, M. Concepción Soutelo, Jesús Sueiro. Madrid: Ana Aliaga, Raquel Baños, José M. Casanova, Santiago Castellanos, José Corral, Angélica Fajardo, Antonia García, M. Begoña García, Alfredo Gómez de Cádiz, Manuel Gómez, Paloma González, M. Teresa Hernández, Paloma Hernández, M. del Canto de Hoyos, M. Carmen López, Rosa Martín, Isabel Miguel, José M. Molero, Joaquín Morera, Alicia Muñoz, Francisco Muñoz, Javier Muñoz, M. Soledad Núñez, Lourdes Pulido, Ana Rodríguez, Carmen Rodríguez, Ana Ruiz, Ernestina Ruiz, Javier de la Torre, Amalia Velázquez, Lourdes Visedo, Antonio Yagüe. Rioja: Carmen Babace, M. Mar Díez, Francisco García, Tomas García, Jesús Ortega, Olga Revilla, Rosa Ruiz de Austri, José Luis Torres, Antonio Trueba, Santiago Vera. Valencia: Dolores Alfonso, Manuel Batalla, Lourdes Bermejo, Nuria Bosch, Cristina Calvo, Beatriz Camaro, M. Pilar Carceller, Manuela Domingo, Manuel Galindo, Carmen Gandía, Concepción García, Andrés Vicente Genovés, M. Carmen González, M. Ángeles Goterris, Amparo Haya, Eva M. Izquierdo, Carmen Lloret, Engracia López, Pilar Marín, M. José Martín, Susana Martínez, Amparo Melchor, José Antonio Minaya, M. José Monedero, José Monleón, Isabel Monreal, M. Paz Ortega, Nieves Peiró, Vicenta Pineda, Gloria Rabanaque, Remei Raga, Jazmín Ripoll, Cecilia Ruiz, Miguel Antón Sánchez, Beatriz Sánchez-Peral, María Jesús Sancho, M. Ángeles Soriano, Dantes Tórtola, Vicente Vergara.