To determine changes in the prevalence of dyslipidemias during the pre-COVID-19 and COVID-19 years in three regions of Ecuador.
DesignCross-sectional study.
SiteQuito, Guayaquil, and El Coca.
ParticipantsAdults with cholesterol, HDL, LDL, and triglyceride levels at primary care centers from January 2017 to December 2022.
InterventionsNot applicable.
Main measurementsData were obtained from five BIODIMED primary care centers. Cholesterol, HDL, LDL, and triglyceride levels were classified according to the ATP III guidelines. Dyslipidemia was considered present when one or more parameters exceeded specific thresholds. Sociodemographic variables and the year of examination were included as independent variables.
ResultsThe study analyzed 110,521 participants’ laboratory results, where 65.3% were males and an average age of 38±12 years. The study spanned the Andean (72.4%), Coast (15.4%), and Amazonic region (12.3%). Pre-pandemic exams constituted 60.9% of the sample. The prevalence of dyslipidemia increased gradually from 43.1% in 2017 to 64.1% in 2022. Cholesterol levels, HDL, and LDL exhibited changes during the pandemic, with an increased risk of hypercholesterolemia, low HDL, and high LDL.
ConclusionsDuring the COVID-19 pandemic, a notable increase in the prevalence of dyslipidemias, including hypercholesterolemia, high triglycerides, and high LDL, was determined across three regions in Ecuador.
Determinar los cambios en la prevalencia de dislipidemias durante los años previos a la COVID-19 y durante la misma en tres regiones de Ecuador.
DiseñoEstudio transversal.
UbicaciónQuito, Guayaquil y El Coca.
ParticipantesAdultos con niveles de colesterol de lipoproteínas de alta densidad (HDL), de lipoproteínas de baja densidad (LDL) y triglicéridos en centros de atención primaria desde enero de 2017 hasta diciembre de 2022.
IntervencionesNo aplica.
Principales medicionesLos datos se obtuvieron de cinco centros de atención primaria BIODIMED. Los niveles de colesterol HDL, LDL y triglicéridos se clasificaron según las directrices del Adult Treatment Panel III (ATP III). Se consideró que existía dislipidemia cuando uno o más parámetros superaban los umbrales específicos. Se incluyeron variables sociodemográficas y el año de examen como variables independientes.
ResultadosEl estudio analizó los resultados de laboratorio de 110.521 participantes, donde el 65,3% eran hombres y la edad promedio era de 38±12 años. El estudio abarcó la región Andina (72,4%), la Costa (15,4%) y la región Amazónica (12,3%). Los exámenes prepandemia constituyeron el 60,9% de la muestra. La prevalencia de dislipidemia aumentó gradualmente del 43,1% en 2017 al 64,1% en 2022. Los niveles de colesterol HDL y LDL mostraron cambios durante la pandemia, con un riesgo aumentado de hipercolesterolemia, HDL bajo y LDL alto.
ConclusionesDurante la pandemia de COVID-19, se determinó un aumento notable en la prevalencia de dislipidemias, incluyendo hipercolesterolemia, triglicéridos altos y LDL alto, en tres regiones de Ecuador.
The acute respiratory infection caused by the coronavirus SARS-CoV-2 was initially identified in Wuhan, China, at the end of 2019, reaching the pandemic in March 2020.1 By December 2022, more than 200 million cases had been diagnosed worldwide.2 The first case was reported in Ecuador on February 29, 2020, with over 1,000,000 confirmed cases by December 2022.1 For this reason, and due to the rapid progression of the disease, governments implemented various preventive strategies primarily aimed at reducing human mobility, including lockdowns and social distancing measures.3
These preventive measures led to significant changes in daily activities, including alterations in dietary habits (increased consumption of non-perishable foods), a decrease in physical activity (closure of gyms, schools, mobility restrictions), and an increase in sedentary behavior (telecommuting, school closures, leisure sites, etc.). Individuals’ psychological states were also affected, increasing stress, boredom, and anxiety.4 Furthermore, public health was impacted by a decrease in the management of chronic conditions in healthcare centers and an increase in economic inequalities. This combination of external and internal factors is related to the prevalence of cardiovascular diseases, leading to an increased cardiovascular risk (hypertension, diabetes mellitus, and hypercholesterolemia) and deaths associated with these conditions (arrhythmias, cardiomyopathies, peripheral arterial disease, heart attacks, etc.).5,6
On the other hand, dyslipidemias, defined as lipid metabolism disorders characterized by one or more of the following parameters: elevated cholesterol and triglycerides, low levels of high-density lipoproteins (HDL), and high levels of low-density lipoproteins (LDL),7 are considered one of the most important and common risk factors for atherosclerotic cardiovascular disease (ASCVD) worldwide.8 This is especially true when they are associated with sedentary lifestyles, smoking, high-calorie diets, diabetes mellitus, and obesity, which were altered during the COVID-19 pandemic.9
According to the National Health Survey of Ecuador, in 2012, the population between 10 and 59 years had a prevalence of hypercholesterolemia, low HDL, high LDL, and hypertriglyceridemia of 24.5%, 53.3%, 19.9%, and 28.7%, respectively.8,10 However, it has not been described whether the COVID-19 pandemic has led to changes in the prevalence of these conditions, mainly due to the increased frequency of anxiety, stress, and sedentary behavior in the population, as well as the inflammatory process generated by acute infection.11–13
This study aimed to determine changes in the prevalence of dyslipidemias in a pre-COVID-19 and COVID-19 context in individuals over 18 years, assessed in primary care centers located in three regions of Ecuador.
Materials and methodsThis article was prepared following the STROBE initiative for reporting observational studies.14
Study designCross-sectional study.
Setting and participantsLaboratory records of patients were evaluated from five primary care medical centers in three Ecuadorian cities: three from Quito and one from Guayaquil and El Coca; these three cities represented the Andean, Coast, and Amazon regions, respectively. Results of total cholesterol, HDL, LDL, and triglyceride levels of men and women over 18 years obtained from January 2017 to December 2022 were included. All serum samples were collected by peripheric venipuncture after at least twelve hours of fasting using a vacuum extraction method (Vacutainer™). Pregnant patients were excluded.
Sample sizeSample size calculation was not performed because the entire population that met the eligibility criteria was included. Strict data security protocols were followed to ensure patient confidentiality and anonymity.
Data sourcesAnonymized data were obtained from the BIODIMED company's database, which operates primary care centers in the mentioned cities.
Measurement and equipment considerationsAll samples were processed in the BIODIMED-Tomás de Berlanga central laboratory in Quito. This specialized laboratory meets rigorous external and internal quality control systems in compliance with the international recommendations established for the pre-analytical, analytical, and post-analytical phases. The laboratory complies with ISO 15189:2012; ISO 9001:2015; ISO 14001:2015 standards regarding external quality control. To assure international quality specifications, the Levey y Jennings and the Westgard Programs are implemented during the analysis of the samples, as well as the quality control through the MedlabQC informatic system. Measurements were performed in the Erba Lachema®, Biochemical analyzer XL 1000, with a monthly programmed calibration. The CHOD-PAP/Total cholesterol, Direct/HDL, Direct/LDL, and GPO-Trinder/Triglycerides kit tests were used through photometric measurements previously controlled by internal quality control of the Clinical Laboratory Improvement Amendments (CLIA) specifications of 3 levels (Low-Normal-High) of biological matrix, and external commercial quality control of ISO 17043 standard.
VariablesCholesterol, HDL, LDL, and triglyceride levels were categorized based on the Adult Treatment Panel III (ATP-III) guidelines.15 Similarly, they were classified based on the outcome (Normal/Abnormal), with abnormal values defined as total cholesterol greater than or equal to 200mg/dL, HDL less than 40mg/dL, LDL greater than or equal to 130mg/dL (higher risk of atheroma formation), and triglycerides greater than or equal to 150mg/dL. The dependent variable considered was the dichotomous variable dyslipidemia (Yes/No), defined as an abnormal result in one or more of the requested tests (cholesterol, HDL, LDL, triglycerides).
Sociodemographic data, including sex, age, place of origin, and examination year, were used as independent variables. The examination year variable was subclassified, considering examinations conducted between 2017 and 2019 as pre-pandemic (unexposed) and 2020 to 2022 as pandemic (exposed).
Statistical methodsAn exploratory data analysis was performed, followed by descriptive statistics, including measures of central tendency (median, mean) and measures of dispersion (standard deviation and interquartile range), according to each variable. Frequency tables were generated for qualitative variables.
The prevalence of dyslipidemia and subgroups (total cholesterol, HDL, LDL, triglycerides) was estimated, and pre-pandemic and pandemic prevalence was calculated. Subsequently, bivariate analyses were conducted using parametric tests and the calculation of Odds Ratios (OR) with their respective 95% confidence intervals (95% CI), using the presence of dyslipidemia (yes/no), total cholesterol≥200mg/dL, HDL<40mg/dL (yes/no), LDL≥130mg/dL (yes/no), and triglycerides≥150mg/dL (yes/no) as dependent variables. To determine the mean difference between the quantitative variables cholesterol, HDL, LDL, and triglycerides among the cities analyzed, a one-factor ANOVA was applied, where, based on the statistically significant result and the present heterogeneity, the Games–Howell post hoc statistic was applied. Statistical analysis was performed using SPSS Version 26® software.
BiasGiven the design used, the risk of confounding bias is present; however, it was controlled through variable stratification for statistical analysis.
Ethical principlesEthical guidelines for research as defined by the Declaration of Helsinki16 were considered, and approval was obtained from the Ethics Committee for Human Research of the General Hospital San Francisco, with code number 13, version 1.
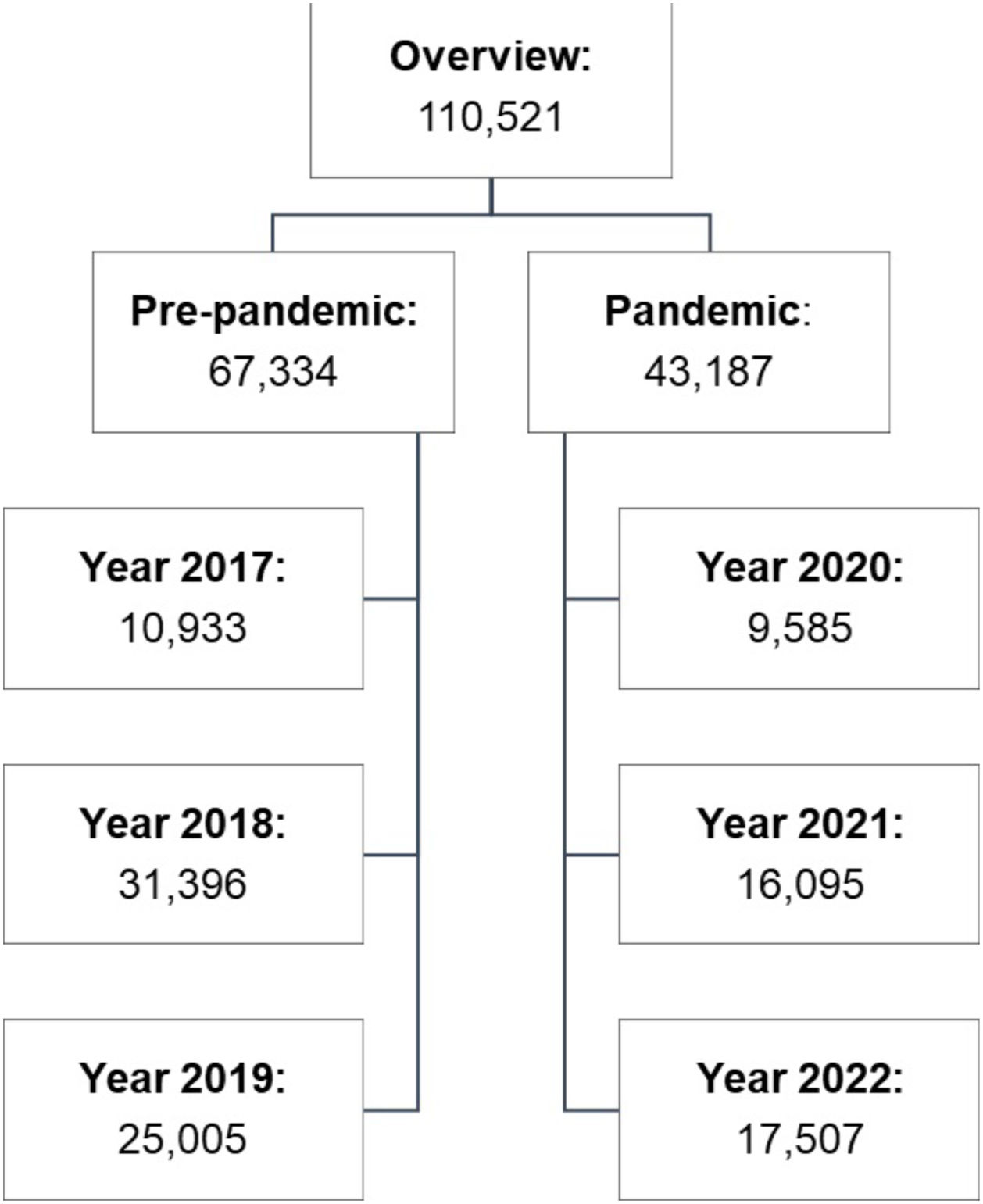
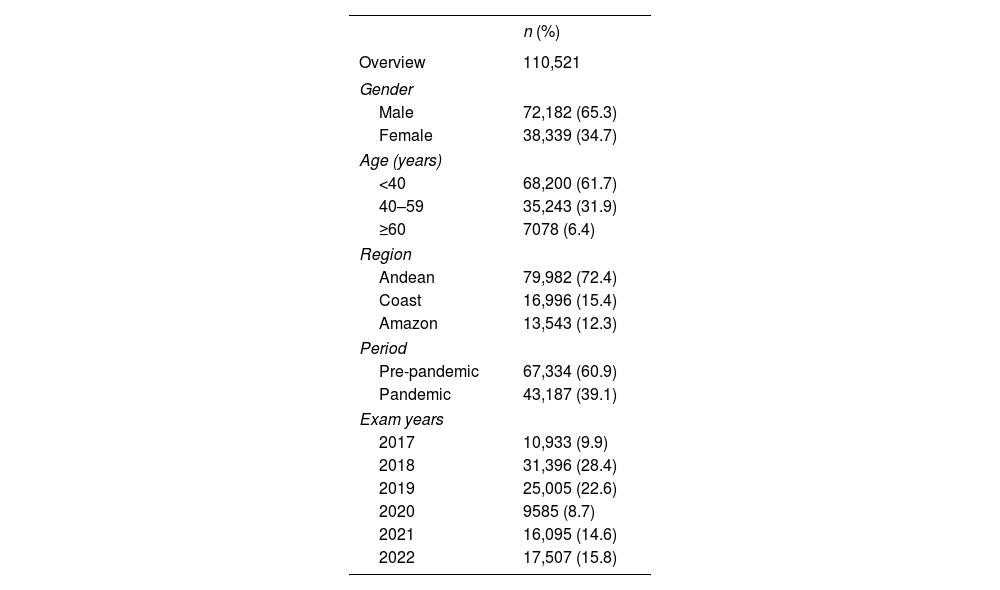
ResultsParticipants and descriptive data110,521 participants’ results were assessed (Fig. 1). The analyzed population comprises 65.3% males, with an average age of 38±12 years. 61.7% of the population is under 40, and 72.4% come from the Ecuadorian Andean region. 60.9% of the exams were conducted in the pre-pandemic period (2017–2019), where it is evident that 2018 and 2019 had the highest representation in the sample, with 28.4% and 22.6%, respectively (Table 1).
Sociodemographic characteristics of participants.
| n (%) | |
|---|---|
| Overview | 110,521 |
| Gender | |
| Male | 72,182 (65.3) |
| Female | 38,339 (34.7) |
| Age (years) | |
| <40 | 68,200 (61.7) |
| 40–59 | 35,243 (31.9) |
| ≥60 | 7078 (6.4) |
| Region | |
| Andean | 79,982 (72.4) |
| Coast | 16,996 (15.4) |
| Amazon | 13,543 (12.3) |
| Period | |
| Pre-pandemic | 67,334 (60.9) |
| Pandemic | 43,187 (39.1) |
| Exam years | |
| 2017 | 10,933 (9.9) |
| 2018 | 31,396 (28.4) |
| 2019 | 25,005 (22.6) |
| 2020 | 9585 (8.7) |
| 2021 | 16,095 (14.6) |
| 2022 | 17,507 (15.8) |
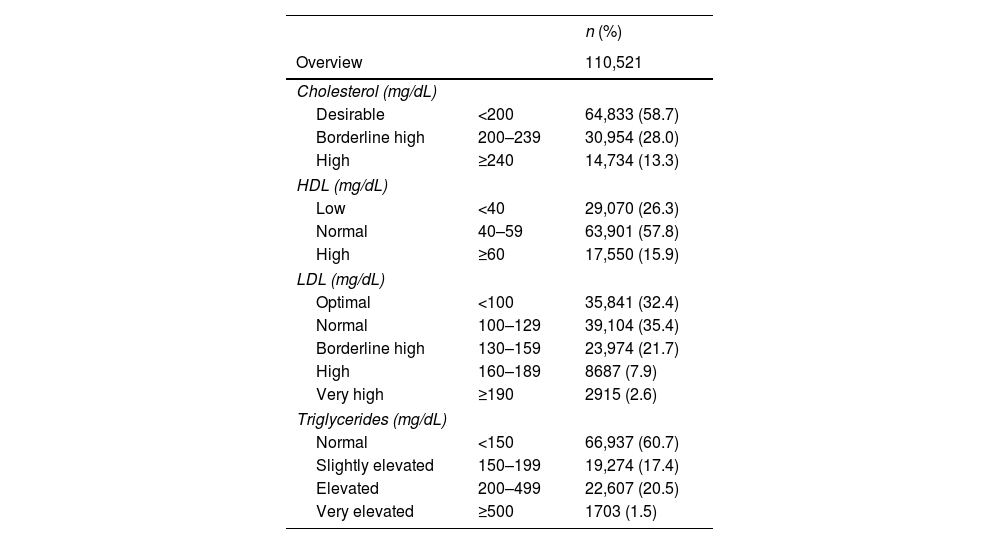
Table 2 describes the frequency of dyslipidemia according to the ATP-III classification. Mean lipid levels and mean differences among the three cities are shown in Supplementary Appendix.
Classification of total cholesterol, HDL, LDL, and triglyceride values according to the adult treatment panel III guidelines.
| n (%) | ||
|---|---|---|
| Overview | 110,521 | |
| Cholesterol (mg/dL) | ||
| Desirable | <200 | 64,833 (58.7) |
| Borderline high | 200–239 | 30,954 (28.0) |
| High | ≥240 | 14,734 (13.3) |
| HDL (mg/dL) | ||
| Low | <40 | 29,070 (26.3) |
| Normal | 40–59 | 63,901 (57.8) |
| High | ≥60 | 17,550 (15.9) |
| LDL (mg/dL) | ||
| Optimal | <100 | 35,841 (32.4) |
| Normal | 100–129 | 39,104 (35.4) |
| Borderline high | 130–159 | 23,974 (21.7) |
| High | 160–189 | 8687 (7.9) |
| Very high | ≥190 | 2915 (2.6) |
| Triglycerides (mg/dL) | ||
| Normal | <150 | 66,937 (60.7) |
| Slightly elevated | 150–199 | 19,274 (17.4) |
| Elevated | 200–499 | 22,607 (20.5) |
| Very elevated | ≥500 | 1703 (1.5) |
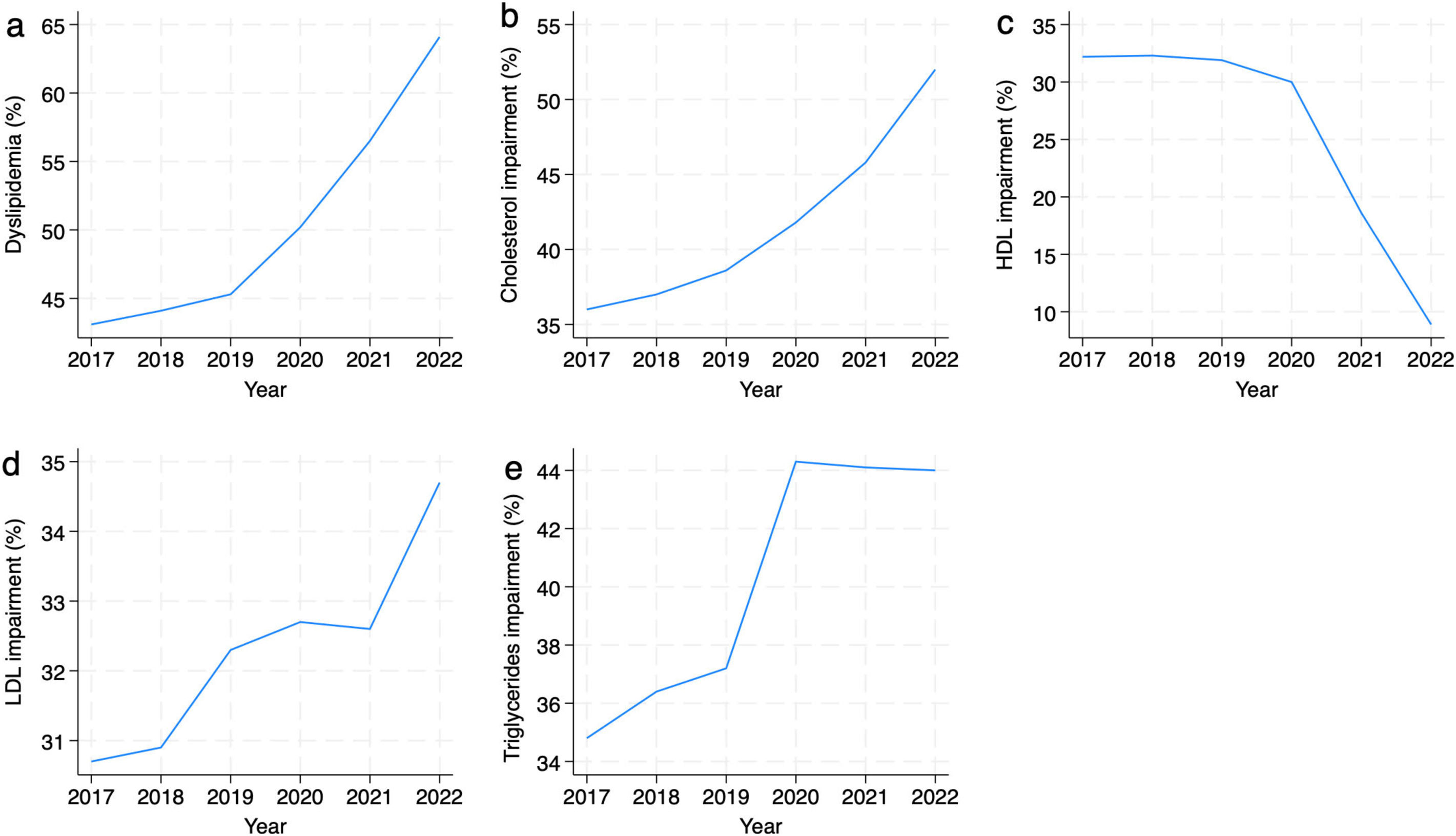
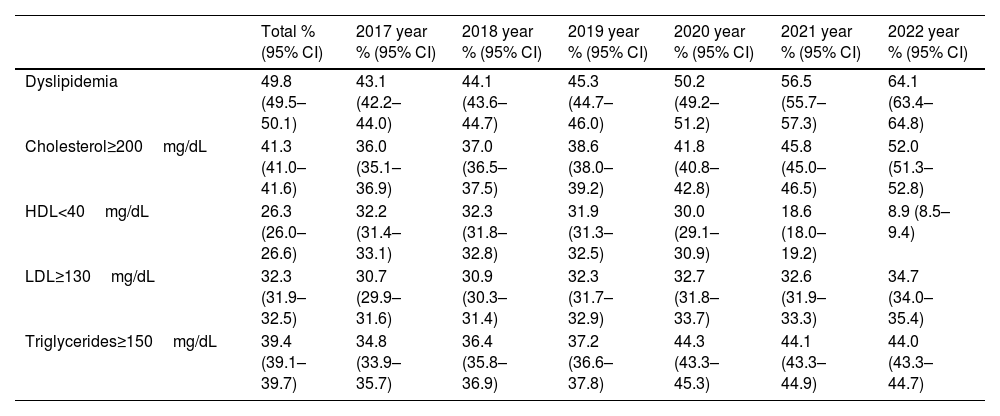
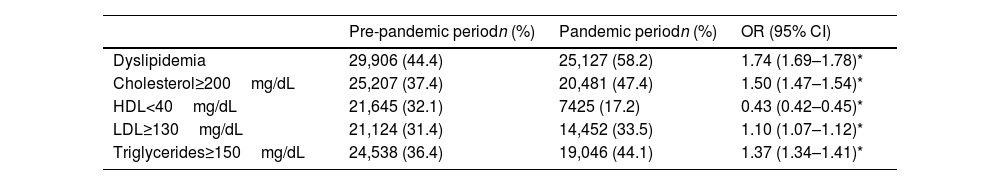
The overall prevalence of dyslipidemia in the population was 49.8% (95% CI: 49.5–50.1) (Table 3). There is a gradual increase in the prevalence (Fig. 2a), identifying a higher probability of presenting this condition during the pandemic. These differences were statistically significant (Table 4).
Prevalence of dyslipidemia, hypercholesterolemia, low HDL, high LDL, and hypertriglyceridemia.
| Total % (95% CI) | 2017 year % (95% CI) | 2018 year % (95% CI) | 2019 year % (95% CI) | 2020 year % (95% CI) | 2021 year % (95% CI) | 2022 year % (95% CI) | |
|---|---|---|---|---|---|---|---|
| Dyslipidemia | 49.8 (49.5–50.1) | 43.1 (42.2–44.0) | 44.1 (43.6–44.7) | 45.3 (44.7–46.0) | 50.2 (49.2–51.2) | 56.5 (55.7–57.3) | 64.1 (63.4–64.8) |
| Cholesterol≥200mg/dL | 41.3 (41.0–41.6) | 36.0 (35.1–36.9) | 37.0 (36.5–37.5) | 38.6 (38.0–39.2) | 41.8 (40.8–42.8) | 45.8 (45.0–46.5) | 52.0 (51.3–52.8) |
| HDL<40mg/dL | 26.3 (26.0–26.6) | 32.2 (31.4–33.1) | 32.3 (31.8–32.8) | 31.9 (31.3–32.5) | 30.0 (29.1–30.9) | 18.6 (18.0–19.2) | 8.9 (8.5–9.4) |
| LDL≥130mg/dL | 32.3 (31.9–32.5) | 30.7 (29.9–31.6) | 30.9 (30.3–31.4) | 32.3 (31.7–32.9) | 32.7 (31.8–33.7) | 32.6 (31.9–33.3) | 34.7 (34.0–35.4) |
| Triglycerides≥150mg/dL | 39.4 (39.1–39.7) | 34.8 (33.9–35.7) | 36.4 (35.8–36.9) | 37.2 (36.6–37.8) | 44.3 (43.3–45.3) | 44.1 (43.3–44.9) | 44.0 (43.3–44.7) |
Prevalence and risk of dyslipidemia, hypercholesterolemia, low HDL, high LDL, and hypertriglyceridemia during the pandemic.
| Pre-pandemic periodn (%) | Pandemic periodn (%) | OR (95% CI) | |
|---|---|---|---|
| Dyslipidemia | 29,906 (44.4) | 25,127 (58.2) | 1.74 (1.69–1.78)* |
| Cholesterol≥200mg/dL | 25,207 (37.4) | 20,481 (47.4) | 1.50 (1.47–1.54)* |
| HDL<40mg/dL | 21,645 (32.1) | 7425 (17.2) | 0.43 (0.42–0.45)* |
| LDL≥130mg/dL | 21,124 (31.4) | 14,452 (33.5) | 1.10 (1.07–1.12)* |
| Triglycerides≥150mg/dL | 24,538 (36.4) | 19,046 (44.1) | 1.37 (1.34–1.41)* |
The mean cholesterol level in the population was 195.2±40.5mg/dL, with an overall prevalence of hypercholesterolemia of 41.3% (95% CI: 41.0–41.6) (Table 3). It is evident that during the COVID-19 pandemic, the probability of hypercholesterolemia increased compared to the pre-pandemic period (OR: 1.50; 1.47–1.54) (Table 4).
HDLThe mean HDL level was 48.2±12.9mg/dL in the analyzed population. There was an overall prevalence of HDL below 40mg/dL of 26.3% (95% CI: 26.0–26.6) (Table 3). The frequency of this condition gradually decreased from 32.2% in 2017 to 30.0% in 2020. Interestingly, the decrease becomes more noticeable, reaching a prevalence as low as 8.9% in 2022 (Fig. 2c).
LDLThe mean LDL in the studied population was 116.8±34.4mg/dL, with a prevalence of LDL equal to or greater than 130mg/dL of 32.3% (95% CI: 31.9–32.5) (Table 3). Similarly, during the COVID-19 pandemic, the risk increased by 1.10 (95% CI: 1.07–1.12) compared to the pre-pandemic period (Table 4).
TriglyceridesThe mean triglyceride level in the analyzed population was 156.1±117.8, and the prevalence of triglycerides equal to or greater than 150mg/dL was 39.4% (95% CI: 39.1–39.7) (Table 3). This population's risk of hypertriglyceridemia increased during the COVID-19 pandemic (OR: 1.37; 1.34–1.41) compared to the previous period (Table 4).
DiscussionTo our knowledge, this article is the first to assess the impact of the COVID-19 pandemic on the prevalence of dyslipidemia in Latin American countries, specifically in Ecuador, filling this knowledge gap with a representative population.
Different authors have linked acute COVID-19 infection to the subsequent development of dyslipidemias. This association could be explained by the pathophysiological effects of the disease on the body, such as damage to the organs responsible for lipid metabolism or the increase in lipids due to their role in the immune system and the viral cycle.17
A systematic review of dyslipidemias on a global scale identified changes in cholesterol levels over the past 20 years (up to 2019) on different continents.18 In Asia and Latin America, the annual increase in cholesterol values persists, possibly related to the region's economic development, influencing lifestyle habits, especially dietary habits.18,19 Our data resemble the reported trend in the Asian continent and Latin American region because there has been a constant annual increase in cholesterol values between 2017 and 2022, indicating a change in prevalence compared to the years before the total cholesterol pandemic, which varied by a maximum of 2%. However, the changes have been more than 3% since the pandemic started compared to the previous year. Similarly, during the pandemic, the changes implemented by local governments worldwide, interfering with daily activities, have led to changes in mental state and lifestyle among the population.11 This is confirmed by a study conducted in Italy in 2021, which showed an increase of more than 6% in the prevalence of total cholesterol and up to 15% in low LDL values.20 Like what was identified in our results, this trend of increase also occurred with triglyceride values, which was more noticeable during the pandemic period with an annual increase in prevalence. This aligns with what was observed in Slovenia, where a cohort study described that lockdown was associated with an increase in total cholesterol, LDL, and triglyceride values, mainly related to changes in dietary habits, stress, and anxiety.4,21
Regarding the accepted HDL values, surprisingly, there is a change in the prevalence of HDL less than 40mg/dL, with a tendency to decrease by up to 10% compared to pre-pandemic data. These results contrast with what is found in the literature, where HDL levels significantly reduce different populations during lockdown.18
The use of retrospective data and not considering other clinical factors such as the body mass index, chronic disease history, glucose metabolism, and dietary habits are limitations of this study. Additionally, there is no direct evidence of a relationship between the infectious process and laboratory results. Likewise, the decrease in the number of samples related to the pandemic period compared to the previous period is a limitation related to the reduction in preventive consultations and follow-up of chronic diseases. However, it is interesting to note that the overall prevalence of dyslipidemia increases despite the smaller population size.
ConclusionDuring the COVID-19 pandemic, the prevalence of dyslipidemias, including hypercholesterolemia, hypertriglyceridemia, and low LDL, increased in three cities in Ecuador. These results underscore the profound impact of lifestyle changes during the pandemic on lipids-related cardiovascular risk factors, highlighting the need for preventive measures.
- •
During the pandemic it was evident an increase in dyslipidemias, with a particular emphasis on the American and Asian continents.
- •
This increase was attributed to changes in diet and physical activity as key contributing factors, as assessed primarily in European studies.
- •
The COVID-19 pandemic and related lockdown measures have impacted the prevalence of dyslipidemias in Ecuador, in a population of over 100,000 individuals.
- •
This is one of the first studies to assess the impact of COVID-19 on the prevalence of dyslipidemias in the region, providing relevant information on how changes in lifestyle habits during the pandemic influenced the cardiovascular health of the Ecuadorian population.
- •
Detecting and controlling cardiovascular risk factors, such as dyslipidemias, as a fundamental part of preventive healthcare and managing chronic diseases in the Ecuadorian population and possibly in other Latin American regions, gaining even more importance post-pandemic.
The study was approved by the Ethics Committee for Human Research of the General Hospital San Francisco, with code number 13, version 1. All participants approved and signed the informed consent.
FundingThis project funding for ANID+subvención a instalación en la academia convocatoria año 2022+85220114; and J.R. received an ANID-Subdirección de Capital Humano/Doctorado Nacional/2024-21242396 scholarship.
Conflict of interestsNo conflicts of interest are reported.
ANID – MILENIO – NCS2021_013.
BIODIMED S.A.