To describe baseline socio-demographic and clinical characteristics and drugs prescribed for secondary prevention after a first episode of ACS and to assess differences between men and women.
SettingPHC in Catalonia. Data source: SIDIAP (Information System for Research in Primary Care).
ParticipantsPatients who suffered an ACS during 2009–2016 and followed-up in PHC centres of the Catalan Health Institute in Catalonia.
InterventionsNot applicable.
Main measuresSocio-demographic and clinical characteristics at baseline: sex, age, socioeconomic index, toxic habits, comorbidities, study drugs (prescribed for cardiovascular secondary prevention: antiplatelets, betablockers, statins, drugs acting on the renin–angiotensin system) and comedications.
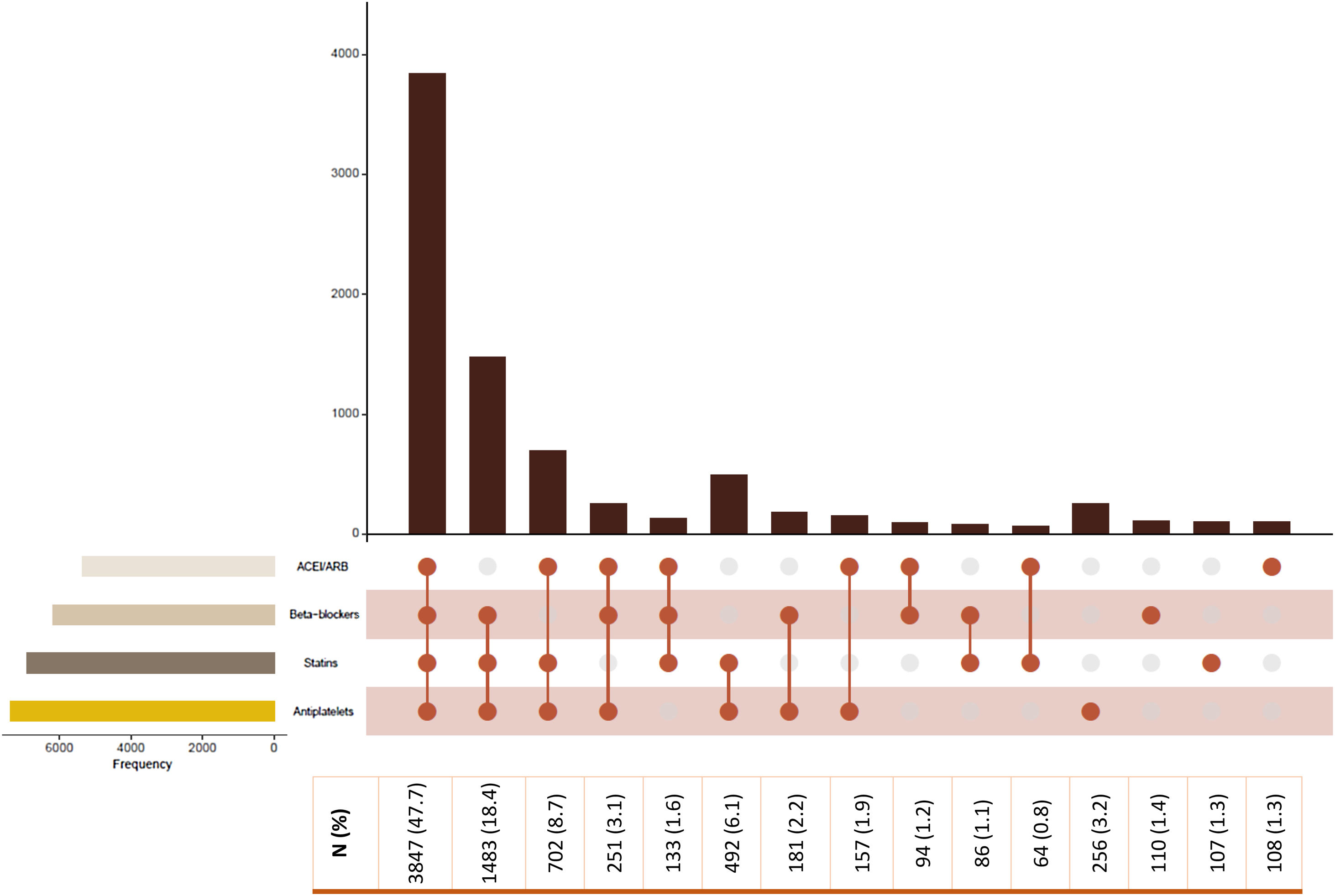
Results8071 patients included, 71.3% of them were men and 80.2% had an acute myocardial infarction. Their mean age was 65.3 and women were older than men. The most frequent comorbidities were hypertension, dyslipidaemia and diabetes and they were more common in women. Antiplatelets (91.3%) and statins (85.7%) were the study drugs most prescribed. The uses of all comedications were significantly higher in women, except for nitrates. The combination of four study groups was initially prescribed in 47.7% of patients and combination of beta-blockers, statins and antiplatelets was prescribed in 18.4%. More men than women received all recommended pharmacological groups.
ConclusionWomen were older, had more comorbidities and received more comedications. Most patients were treated with a combination of four or three study drugs for secondary prevention. Men initiated more drug treatments for secondary prevention and dual antiplatelet therapy than women.
EUPAS RegisterEUPAS19017.
Describir las características sociodemográficas y clínicas basales, y los fármacos prescritos para la prevención cardiovascular secundaria tras un síndrome coronario agudo (SCA). Analizar si existen diferencias entre varones y mujeres.
EmplazamientoAtención primaria (AP) en Cataluña. Fuente de datos: Sistema de Información para el Desarrollo de la Investigación en AP (SIDIAP).
ParticipantesPacientes que hayan sufrido un primer SCA durante 2009-2016, seguidos en AP del Instituto Catalán de la Salud en Cataluña.
IntervencionesNo aplica.
Mediciones principalesCaracterísticas sociodemográficas y clínicas al inicio: sexo, edad, índice socioeconómico, hábitos tóxicos, comorbilidades, fármacos de estudio (prescritos para prevención secundaria: antiagregantes, betabloqueantes, estatinas, fármacos del sistema renina-angiotensina) y fármacos concomitantes.
ResultadosSe incluyeron 8.071 pacientes; 71,3% varones y 80,2% habían sufrido infarto. La edad media era de 65,3 años y las mujeres eran mayores que los varones. Las comorbilidades más frecuentes fueron hipertensión, dislipemia y diabetes; más comunes en mujeres. Antiagregantes (91,3%) y estatinas (85,7%) fueron los fármacos más prescritos. El uso de todas las comedicaciones era más frecuente en mujeres, excepto nitratos. La combinación de los 4 grupos farmacológicos de estudio se prescribió al 47,7% de los pacientes incluidos y la combinación de antiagregante, betabloqueante y estatina al 18,4%. Más varones que mujeres recibieron los fármacos recomendados.
ConclusionesLas mujeres incluidas eran mayores, con más comorbilidad y mayor uso de comedicaciones. La mayoría de pacientes eran tratados con la combinación de 3 o 4 fármacos para prevención secundaria. Los varones iniciaban más fármacos para prevención secundaria y más terapia antiagregante doble que las mujeres.
EUPAS RegisterEUPAS19017.
Cardiovascular disease remains the most common cause of death worldwide, 31.5% of all deaths and 45% for non-communicable disease deaths in Europe.1,2 Despite these numbers, the incidence of cardiovascular disease has decreased over the last four decades, due to population-level lifestyle changes and the development of effective interventions to treat individuals and invasive procedures and effective drugs to tackle modifiable risk factors.3
Several randomised clinical trials, meta-analyses and cohort studies have shown that long-term administration of aspirin, statins, beta-blockers, and angiotensin-converting enzyme inhibitors (ACEI) or angiotensin-receptor blockers (ARB) improve survival in high risk patients, particularly those with established cardiovascular disease.4–7 Therefore, the European and American Cardiology guidelines recommend in both genders this long-term pharmacological therapy for an acute coronary syndrome (ACS) secondary prevention.8–12
Several population-based studies have analysed the pharmacological secondary prevention in the real-world practice. In Lafeber et al. study, 67% of patients with cardiovascular disease were treated with a combination of aspirin, statin and at least one blood pressure-lowering agent for secondary prevention.13 Sanfélix-Gimeno et al. showed that after an ACS 92.8% of patients were treated with an antiplatelet, 74.7% with beta-blocker, 87.1% with statins and 77.2% with an ACEI or ARB.5
Some population-based studies have described differences between men and women in clinical characteristics and pharmacological treatment received after ACS. Women have been reported to be older than men and have greater comorbidities, such as hypertension, diabetes and dyslipidaemia.14–17 Some differences between genders in secondary prevention have also been described and found that women were less likely to be treated.14–16
This work is part of IMPACT study and the protocol has been previously published.18 The objective of IMPACT study is to assess the impact of the four recommended drugs adherence on mortality and cardiovascular morbidity. This study aims to describe the baseline socio-demographic and clinical characteristics and the medication prescribed for secondary prevention after a first episode of ACS in a Primary Health Care (PHC) cohort in Catalonia (Spain) and to assess differences in these characteristics between women and men.
MethodsStudy designPopulation-based observational cohort study of patients with a first episode of ACS admitted in hospitals of the Catalan Health Institute during 2009–2016, followed-up in PHC. The data source is Information System for Research in Primary Care (SIDIAP) database, which includes PHC data of more than 5.8 million people from Catalonia (approximately 80% of the Catalan population).18
Data sourceSIDIAP database,19 which contains pseudonymized information coming from different data sources: ECAP (electronic health records in PHC of the Catalan Health Institute, including) socio-demographic characteristics, comorbidities registered as International Classification of Disease (ICD) 10 codes (Table S1, Appendix),20 specialist referrals, clinical parameters, toxic habits (smoking and alcohol intake), sickness leave, date of death, laboratory test data; general practitioners’ prescriptions and their corresponding pharmacy invoice data registered as chemical classification system (ATC) codes21; and the CMBD-HA (minimum basic dataset at hospital discharge),22 which includes diagnoses at hospital discharge registered as ICD9 codes (Table S1, Appendix).23
Study populationAll adults with a first episode of ACS (acute myocardial infarction (AMI) or unstable angina) registered in CMBD-HA from 2009 to 2016 with at least two months of follow-up in SIDIAP after the index date were included. The individuals lost in follow-up during the first two months have no information available in the database to be captured. Exclusion criteria: patients with a recorded diagnosis of a previous ischaemic stroke.
Study variablesAt index date: age, gender, socioeconomic MEDEA Index,24,25 toxic habits (smoking and alcohol), body mass index (BMI), type of ACS event (AMI, unstable angina or other forms of ACS), laboratory data (cholesterol, other lipid parameters and glomerular filtration rate), and comorbidities of interest. MEDEA socioeconomic index is a deprivation index built with the information of five cities in Spain (Barcelona, Bilbao, Madrid, Sevilla, Valencia), using the census section as the unit of analysis and 2001 census data, based on five indicators of socioeconomic position: manual workers, unemployment, temporary workers, overall insufficient education and insufficient education in young people. MEDEA is able to detect small areas with socioeconomic inequalities in large cities, allowing the study of associations between socioeconomic indicators and mortality. MEDEA is categorised in five urban quintiles, with quintile 1 (U1) corresponding to the least deprived population and quintile 5 (U5), the most deprived.24 In order to facilitate the presentation of our results, we grouped categories U1 to U3, and U4 to U5. The rural category (R) includes municipalities with less than 10,000 inhabitants and a population density lower than 150/km2. The use of MEDEA index has not been analysed for rural areas. Socioeconomic deprivation measured with MEDEA was associated with an increase in total mortality in urban areas of Catalonia.25
The study drugs were those recommended for secondary prevention: antiplatelets, beta-blockers, statins and ACEI/ARB. Study drugs prescribed after the ACS event and other concomitant drugs were collected after the index date. The initiation of exposure to the study drugs was defined according to the drugs firstly prescribed during the period spanning from index day to 120 days after the event in order to capture all prescriptions in PHC, due to the length of hospital's prescriptions and the delay in the register of the dispensing in our records.
Statistical analysisDemographic and baseline characteristics of the participants were described using counts and proportions for categorical variables and for continuous variables mean with standard deviation (SD) for normally distributed variables and median and interquartile range (IQR) for skewed distributions. Univariate analysis between genders was performed by means of Pearson's Chi-square test and we compared mean or median between groups using Student's T test and Mann–Whitney U test, respectively. The analysis between groups according to the number of study drugs was performed using the ANOVA test (under equal variance assumption) for continuous variables and Pearson's Chi-square test (with continuity correction) for categorical variables.
Regarding to the missing data, we assumed that if data was missing, it meant that the patient did not had that condition.
All analyses were performed using R 3.5.1 (R Core Team, 2020. A language and environment for statistical computing. R Foundation for Statistical Computing, Vienna, Austria. URL https://www.R-project.org/), under a significance level of 0.05.
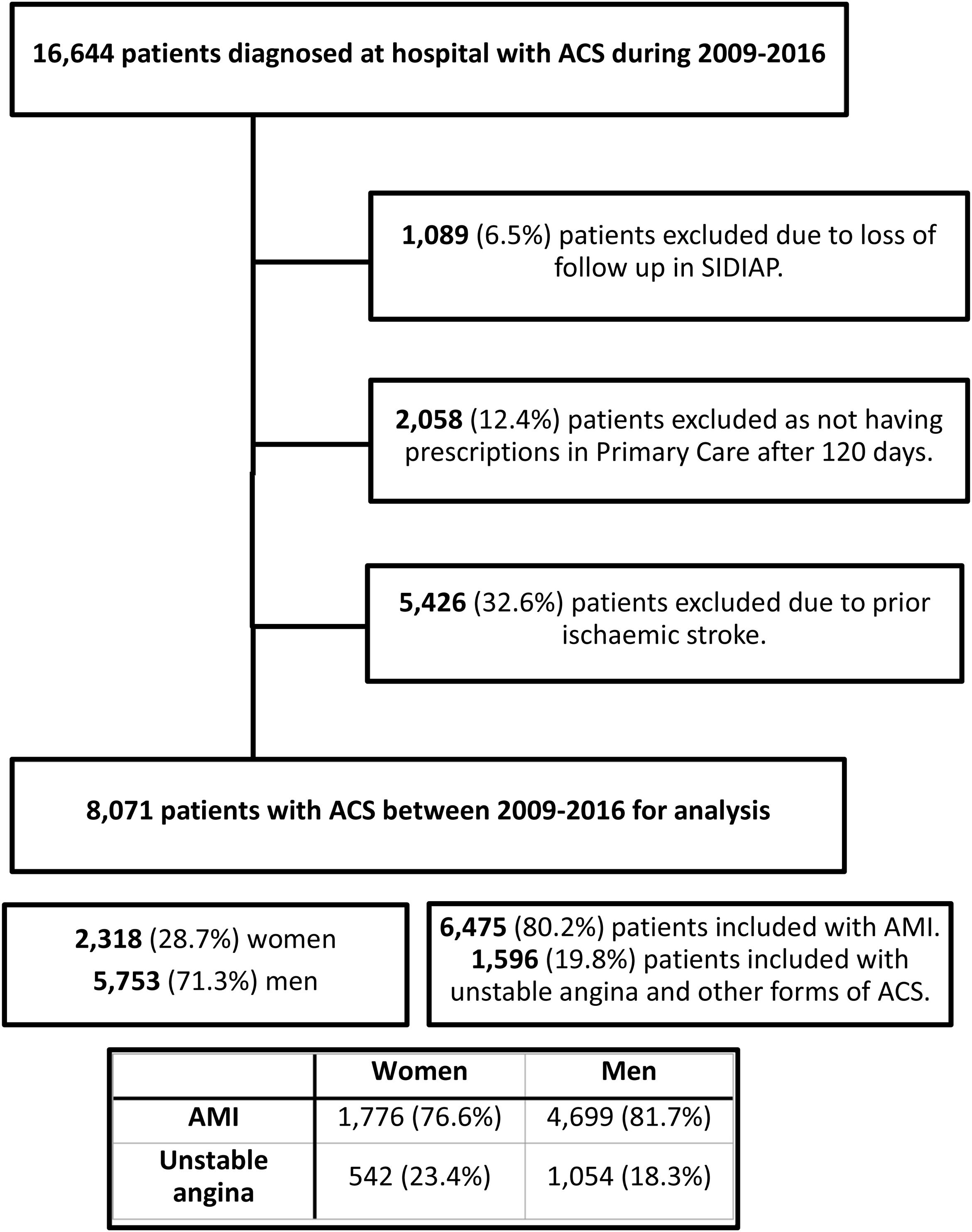
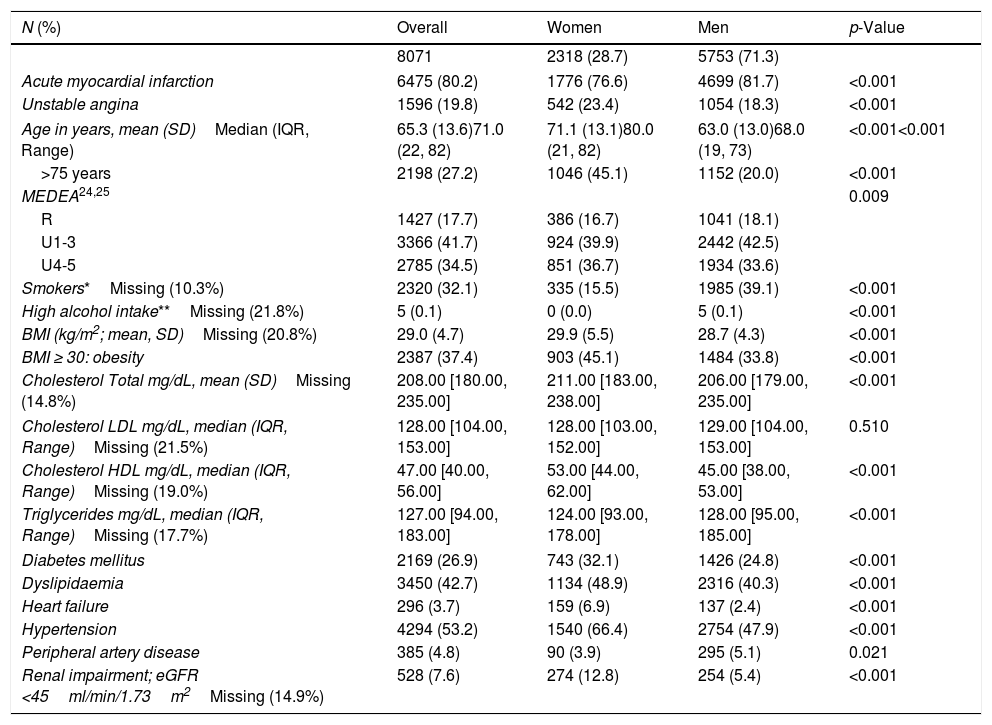
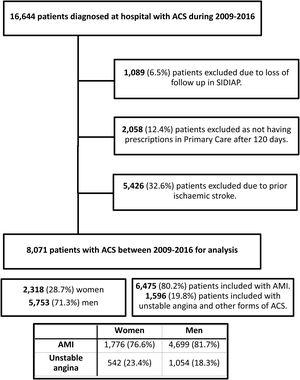
ResultsThere were 16,644 patients admitted to hospital with a first episode of ACS from 2009 to 2016 and 8573 of them were excluded (Scheme 1). 8071 patients were included, 71.3% of them were men and 80.2% had an AMI (men: 81.7%; women: 76.6%). Their mean age was 65.3, women were older than men (71.1 vs 63.0, p<0.001) and 45.1% older than 75. The most frequent comorbidities were hypertension, dyslipidaemia and diabetes and they were all significantly more common in women. Heart failure and renal impairment were also common in women (Table 1).
Gender differences in socio-demographic characteristics, laboratory data and comorbidities.
| N (%) | Overall | Women | Men | p-Value |
|---|---|---|---|---|
| 8071 | 2318 (28.7) | 5753 (71.3) | ||
| Acute myocardial infarction | 6475 (80.2) | 1776 (76.6) | 4699 (81.7) | <0.001 |
| Unstable angina | 1596 (19.8) | 542 (23.4) | 1054 (18.3) | <0.001 |
| Age in years, mean (SD)Median (IQR, Range) | 65.3 (13.6)71.0 (22, 82) | 71.1 (13.1)80.0 (21, 82) | 63.0 (13.0)68.0 (19, 73) | <0.001<0.001 |
| >75 years | 2198 (27.2) | 1046 (45.1) | 1152 (20.0) | <0.001 |
| MEDEA24,25 | 0.009 | |||
| R | 1427 (17.7) | 386 (16.7) | 1041 (18.1) | |
| U1-3 | 3366 (41.7) | 924 (39.9) | 2442 (42.5) | |
| U4-5 | 2785 (34.5) | 851 (36.7) | 1934 (33.6) | |
| Smokers*Missing (10.3%) | 2320 (32.1) | 335 (15.5) | 1985 (39.1) | <0.001 |
| High alcohol intake**Missing (21.8%) | 5 (0.1) | 0 (0.0) | 5 (0.1) | <0.001 |
| BMI (kg/m2; mean, SD)Missing (20.8%) | 29.0 (4.7) | 29.9 (5.5) | 28.7 (4.3) | <0.001 |
| BMI ≥ 30: obesity | 2387 (37.4) | 903 (45.1) | 1484 (33.8) | <0.001 |
| Cholesterol Total mg/dL, mean (SD)Missing (14.8%) | 208.00 [180.00, 235.00] | 211.00 [183.00, 238.00] | 206.00 [179.00, 235.00] | <0.001 |
| Cholesterol LDL mg/dL, median (IQR, Range)Missing (21.5%) | 128.00 [104.00, 153.00] | 128.00 [103.00, 152.00] | 129.00 [104.00, 153.00] | 0.510 |
| Cholesterol HDL mg/dL, median (IQR, Range)Missing (19.0%) | 47.00 [40.00, 56.00] | 53.00 [44.00, 62.00] | 45.00 [38.00, 53.00] | <0.001 |
| Triglycerides mg/dL, median (IQR, Range)Missing (17.7%) | 127.00 [94.00, 183.00] | 124.00 [93.00, 178.00] | 128.00 [95.00, 185.00] | <0.001 |
| Diabetes mellitus | 2169 (26.9) | 743 (32.1) | 1426 (24.8) | <0.001 |
| Dyslipidaemia | 3450 (42.7) | 1134 (48.9) | 2316 (40.3) | <0.001 |
| Heart failure | 296 (3.7) | 159 (6.9) | 137 (2.4) | <0.001 |
| Hypertension | 4294 (53.2) | 1540 (66.4) | 2754 (47.9) | <0.001 |
| Peripheral artery disease | 385 (4.8) | 90 (3.9) | 295 (5.1) | 0.021 |
| Renal impairment; eGFR <45ml/min/1.73m2Missing (14.9%) | 528 (7.6) | 274 (12.8) | 254 (5.4) | <0.001 |
p-Value from Pearson's Chi-square test (categoric variables) and t-test or Mann–Whitney U test (numeric variables) comparing women versus men. BMI, body mass index; LDL-C, low density lipoprotein-cholesterol; HLD-C, high density lipoprotein- cholesterol; eGFR, estimated glomerular filtration rate; R (Rural); U (Urban).
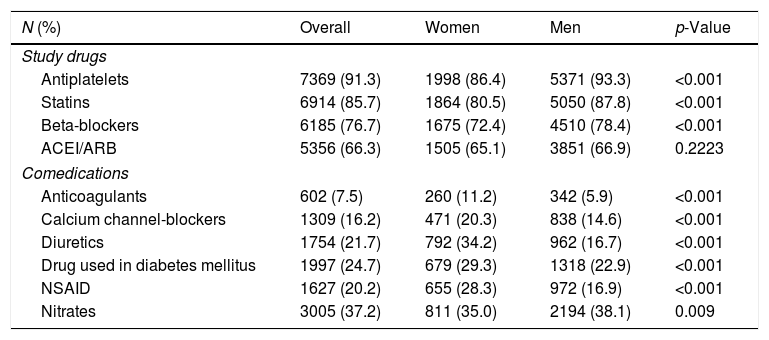
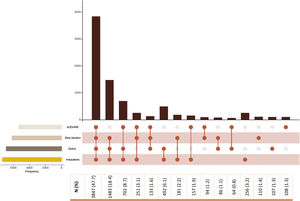
Antiplatelet agents (91.3%) were the most prescribed drugs, followed by statins (85.7%), beta-blockers (76.7%), and lastly, ACEI/ARBs (66.3%). More men than women received all study drugs. Nitrates were the comedication most prescribed overall after the event. The use of all comedications was significantly higher in women, except for nitrates (Table 2). The combination of four study drugs was initially prescribed in 47.7% of patients and 31.8% of total prescriptions were with three study drugs. Beta-blockers, statins and antiplatelets was the more frequent combination of three components (18.4%) (Fig. 1). More men were treated with the combination of four (2879 [50.0%] vs 968 [41.8%], p<0.001) and with the most frequent combination of three drugs: antiplatelets, statins and beta-blockers (1115 [19.4%] vs 368 [15.9%]; p<0.001); and antiplatelets, statins and ACEI/ARB (492 [8.6] vs 210 [9.1], p=0.491).
Gender differences in population that initiate treatment for secondary prevention: study drugs and comedications after the event.
| N (%) | Overall | Women | Men | p-Value |
|---|---|---|---|---|
| Study drugs | ||||
| Antiplatelets | 7369 (91.3) | 1998 (86.4) | 5371 (93.3) | <0.001 |
| Statins | 6914 (85.7) | 1864 (80.5) | 5050 (87.8) | <0.001 |
| Beta-blockers | 6185 (76.7) | 1675 (72.4) | 4510 (78.4) | <0.001 |
| ACEI/ARB | 5356 (66.3) | 1505 (65.1) | 3851 (66.9) | 0.2223 |
| Comedications | ||||
| Anticoagulants | 602 (7.5) | 260 (11.2) | 342 (5.9) | <0.001 |
| Calcium channel-blockers | 1309 (16.2) | 471 (20.3) | 838 (14.6) | <0.001 |
| Diuretics | 1754 (21.7) | 792 (34.2) | 962 (16.7) | <0.001 |
| Drug used in diabetes mellitus | 1997 (24.7) | 679 (29.3) | 1318 (22.9) | <0.001 |
| NSAID | 1627 (20.2) | 655 (28.3) | 972 (16.9) | <0.001 |
| Nitrates | 3005 (37.2) | 811 (35.0) | 2194 (38.1) | 0.009 |
p-Value from Pearson's Chi-square test comparing women versus men. ACEI, angiotensin-converting enzyme inhibitors; ARB, angiotensin-receptor blockers; NSAID, non-steroidal anti-inflammatory drugs.
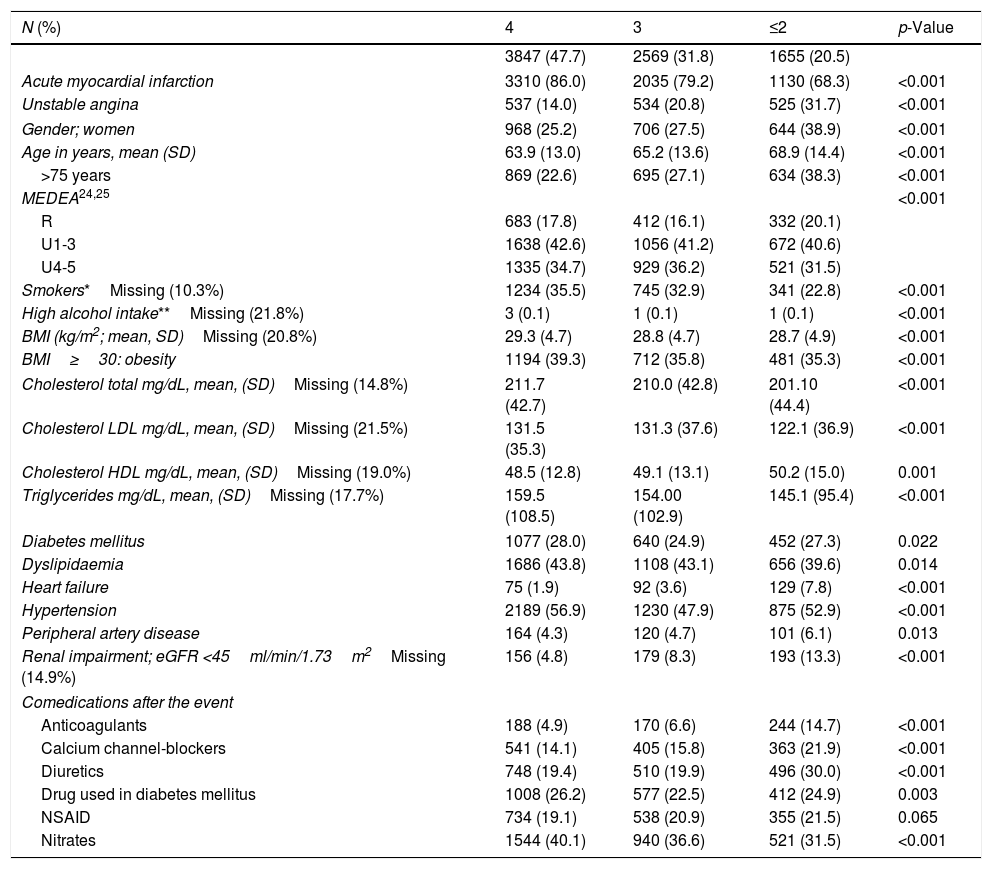
Table 3 compares the baseline characteristics difference of patients by study drug number prescribed. Patients with AMI significantly received four study drugs more frequently (86%) than other combination of three (79.2%) or ≤ two study drugs (68.3%, p<0.001). More women initiated≤two study drugs (38.9%) than three (27.5%) or four (25.2%). Patients receiving≤two study drugs were older (68.9 years). There were more patients treated with other comedications after the event in the group of≤two study drugs than the other combinations (Table 3).
Socio-demographic characteristics, laboratory data, comorbidities and comedications stratified by study drugs number.
| N (%) | 4 | 3 | ≤2 | p-Value |
|---|---|---|---|---|
| 3847 (47.7) | 2569 (31.8) | 1655 (20.5) | ||
| Acute myocardial infarction | 3310 (86.0) | 2035 (79.2) | 1130 (68.3) | <0.001 |
| Unstable angina | 537 (14.0) | 534 (20.8) | 525 (31.7) | <0.001 |
| Gender; women | 968 (25.2) | 706 (27.5) | 644 (38.9) | <0.001 |
| Age in years, mean (SD) | 63.9 (13.0) | 65.2 (13.6) | 68.9 (14.4) | <0.001 |
| >75 years | 869 (22.6) | 695 (27.1) | 634 (38.3) | <0.001 |
| MEDEA24,25 | <0.001 | |||
| R | 683 (17.8) | 412 (16.1) | 332 (20.1) | |
| U1-3 | 1638 (42.6) | 1056 (41.2) | 672 (40.6) | |
| U4-5 | 1335 (34.7) | 929 (36.2) | 521 (31.5) | |
| Smokers*Missing (10.3%) | 1234 (35.5) | 745 (32.9) | 341 (22.8) | <0.001 |
| High alcohol intake**Missing (21.8%) | 3 (0.1) | 1 (0.1) | 1 (0.1) | <0.001 |
| BMI (kg/m2; mean, SD)Missing (20.8%) | 29.3 (4.7) | 28.8 (4.7) | 28.7 (4.9) | <0.001 |
| BMI≥30: obesity | 1194 (39.3) | 712 (35.8) | 481 (35.3) | <0.001 |
| Cholesterol total mg/dL, mean, (SD)Missing (14.8%) | 211.7 (42.7) | 210.0 (42.8) | 201.10 (44.4) | <0.001 |
| Cholesterol LDL mg/dL, mean, (SD)Missing (21.5%) | 131.5 (35.3) | 131.3 (37.6) | 122.1 (36.9) | <0.001 |
| Cholesterol HDL mg/dL, mean, (SD)Missing (19.0%) | 48.5 (12.8) | 49.1 (13.1) | 50.2 (15.0) | 0.001 |
| Triglycerides mg/dL, mean, (SD)Missing (17.7%) | 159.5 (108.5) | 154.00 (102.9) | 145.1 (95.4) | <0.001 |
| Diabetes mellitus | 1077 (28.0) | 640 (24.9) | 452 (27.3) | 0.022 |
| Dyslipidaemia | 1686 (43.8) | 1108 (43.1) | 656 (39.6) | 0.014 |
| Heart failure | 75 (1.9) | 92 (3.6) | 129 (7.8) | <0.001 |
| Hypertension | 2189 (56.9) | 1230 (47.9) | 875 (52.9) | <0.001 |
| Peripheral artery disease | 164 (4.3) | 120 (4.7) | 101 (6.1) | 0.013 |
| Renal impairment; eGFR <45ml/min/1.73m2Missing (14.9%) | 156 (4.8) | 179 (8.3) | 193 (13.3) | <0.001 |
| Comedications after the event | ||||
| Anticoagulants | 188 (4.9) | 170 (6.6) | 244 (14.7) | <0.001 |
| Calcium channel-blockers | 541 (14.1) | 405 (15.8) | 363 (21.9) | <0.001 |
| Diuretics | 748 (19.4) | 510 (19.9) | 496 (30.0) | <0.001 |
| Drug used in diabetes mellitus | 1008 (26.2) | 577 (22.5) | 412 (24.9) | 0.003 |
| NSAID | 734 (19.1) | 538 (20.9) | 355 (21.5) | 0.065 |
| Nitrates | 1544 (40.1) | 940 (36.6) | 521 (31.5) | <0.001 |
p-Value from ANOVA test comparing samples with 4, 3 or 2–1 drugs of interest. ACH, acute coronary heart disease; BMI, body mass index; LDL-C, low density lipoprotein-cholesterol; HLD-C, high density lipoprotein-cholesterol; eGFR, estimated glomerular filtration rate; NSAID, non-steroidal anti-inflammatory drugs; R, Rural; U, Urban.
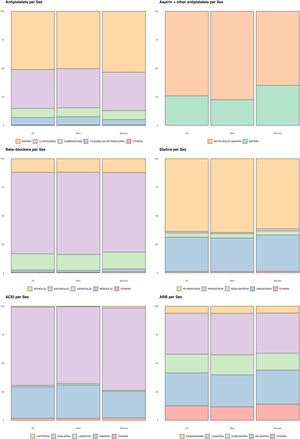
Fig. 2 represents the different drugs prescribed overall, in men and women. Men received dual antiplatelet therapy more frequently than women; the most used antiplatelets were aspirin and clopidogrel. The most prescribed beta-blocker was bisoprolol both in men and women. Atorvastatin was the most prescribed statin for all patients. Enalapril and ramipril were the most used ACEI, being ramipril more frequent in men. Losartan is the most prescribed ARB, followed by valsartan and olmesartan (Fig. 2).
Drugs prescribed per gender. Fig. 2 depicts the different drugs prescribed overall, in men and women. Distribution between genders was compared using the Chi-Square test with all p-values<0.001. ACEI, angiotensin-converting enzyme inhibitors; ARB, angiotensin-receptor blockers.
We report baseline socio-demographic and clinical characteristics of 8701 patients from a Primary Health Care cohort who had a first ACS. Patients’ characteristics have been analysed overall, divided into genders and number of study drugs prescribed. We found that women were older, had greater comorbidity at baseline and received more comedications after the study event than men, probably because they were older when had the first ACS, as described in a similar cohort by Ribas et al.26 In agreement with similar studies, we found a higher prevalence of comorbidities in women,15,27,28 while men had a higher prevalence of peripheral artery disease,29 possibly related with the higher frequency of smoking habit.
With regard to socio-demographic characteristics, the proportion of men and women in our study is not balanced (28.7% of women) and it is similar to previous studies.15,16,26,30
Most patients in our study (91.3%) initiated treatment for secondary prevention with antiplatelets after the first ACS, mainly with dual antiplatelet therapy, as recommended by guidelines.8–10 Statins were the second drug more prescribed (85.7% of patients) and beta-blockers and ACEI/ARB were less prescribed. All patients with established cardiovascular disease should be treated during hospital admission and after discharge with statins, regardless of their cholesterol values.31 ACEI/ARB might be less prescribed as they are not always recommended for all patients, they should be considered in all ST-Elevation Myocardial Infarction patients.8–10 All study drugs were more commonly prescribed in men than women, except for ACEI/ARB, that difference between women and men was slight and not significant, probably related to higher frequency of hypertension in women in our study population, because women were older than men. These results were similar to Lafeber et al.,32 and Sanfélix-Gimeno et al. studies.5 Regarding comedications, anticoagulants and diuretics were the most prescribed in women, possibly related with their higher frequency of atrial fibrillation and heart failure than in men.Women initiated secondary prevention less frequently than men.14–16,33–35 Nevertheless, the majority of our population (79.5%) initiated treatment with three or four drugs combined, and almost half (47.7%) with four study drugs, although we found more women treated with≤two study drugs than with three or four. This may perhaps occur because physicians prescribed fewer drugs to older patients who were multimorbid and polymedicated.36 Probably, the same assumption could be extended to our finding found for women and the number of drugs prescribed, because men usually suffer ACS at an earlier age.37–39
Zeymer et al.40 conducted an observational prospective study including 9998 patients with ACS from June 2000 until December 2002. They reported that patients receiving four drugs were younger and patient's characteristics according to the number of drugs prescribed were similar to our population. They found higher percentage (92.5%) with combination of four or three components and 62.6% with combination of four. The combination of beta-blockers, statins and antiplatelets was also high (39.5%). Also, they suggested that age>75 years old is a potent predictor for not receiving therapy with four components.35,40,41
Other author already mentioned, Lafeber et al.32 conducted an observational prospective cohort study of 2706 recently diagnosed patients clinically manifest coronary artery disease between January 1996 and February 2010. They found fewer patients (67.0%) treated with the combination of aspirin, a statin and ≥one blood-pressure lowering agent(s).32
Aspirin and clopidogrel were the most frequently antiplatelets prescribed. Dual antiplatelet therapy was less frequently prescribed to women as described by previous studies,41–43 probably because women were older.44 Bisoprolol, enalapril, and losartan were the most prescribed beta-blockers with slight differences between genders. The statins most commonly prescribed overall were atorvastatin and simvastatin, probably because they are the statins with more experience of use.
We found a strong relation in the medication prescribed between being women and older in our population, probably because women had the first ACS in older age than men. Consequently, women had lower probability to be treated with study drugs and higher probability to be treated with other comedications.
This study has some limitations inherent to electronic database studies, such as data incompleteness, loss of follow-up of patients suffering an ACS, potential confounders, non-randomised data and possible selection biases. Other limitation is that prescriptions are not linked with diagnoses in SIDIAP database. Our database has PHC's data, therefore some hospital's data is not available.On the other hand, the strengths of our study are the large number of patients included, representativeness for the general population, complete socio-demographic and health records, long follow-up periods and real-world data. Our data is supported by previous studies and the presence of cardiovascular risk factors and outcomes has been previously validated in SIDIAP.45–47
This is the first work conducted with SIDIAP database which analyses the drugs prescribed for secondary prevention of cardiovascular disease providing high value knowledge about the cardiovascular disease in Catalonia (North-East Spain), which represents more than 5.8 million inhabitants in south Europe. The results can be extrapolated to all population in Catalonia and the rest of Spain, as the health systems and population characteristics are similar.
Ethical requirementsIn accordance with European and Spanish legislation on confidentiality and data protection ([EU] 2016/679), the data contained in SIDIAP are always pseudonymised. For the cross-over with the CMBD database, SIDIAP uses a third party to ensure confidentiality.
This study follows all national and international regulations: Declaration of Helsinki and Principles of Good Research Practice.
The study was approved by the IDIAPJGol Research Ethics Committee on May 3, 2017.
FinancingThis study is funded by the IDIAPJGol, in the “6th call for SIDIAP grants” in March 2017.
Conflict of interestsThe authors declare that they have no conflict of interest in conducting this study.