To analyze the prevalence, control, and management of hypertension, hypercholesterolemia, and diabetes mellitus type 2 (DM2).
DesignCross-sectional analysis of all individuals attended in the Catalan primary care centers between 2006 and 2009.
LocationHistory of cardiovascular diseases, diagnosis and treatment of hypertension, hypercholesterolemia, DM2, lipid profile, glycemia and blood pressure data were extracted from electronic medical records. Age-standardized prevalence and levels of management and control were estimated.
ParticipantsIndividuals aged 35–74 years using primary care databases.
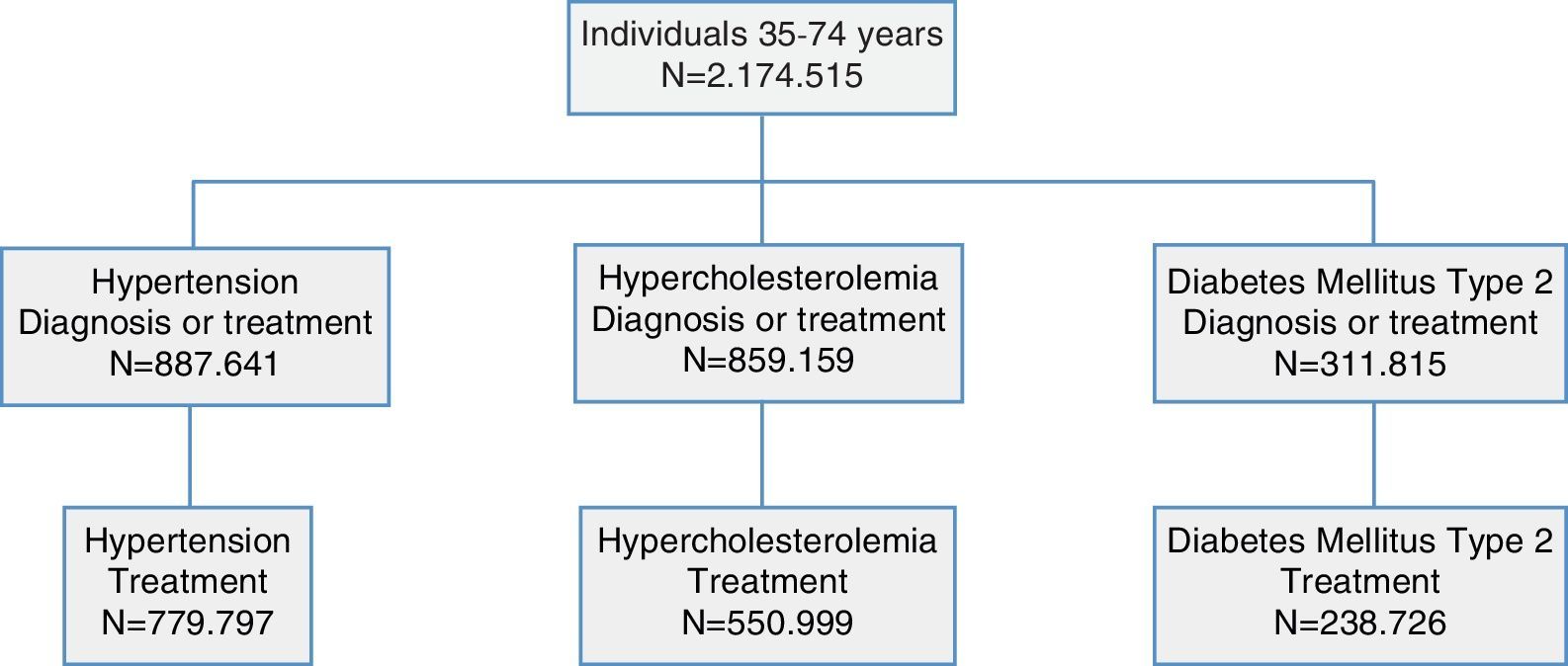
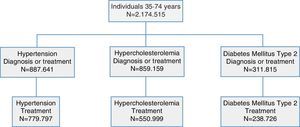
Main measuresA total of 2,174,515 individuals were included (mean age 52 years [SD 11], 47% men).
ResultsHypertension was the most prevalent cardiovascular risk factor (39% in women, 41% in men) followed by hypercholesterolemia (38% and 40%) and DM2 (12% and 16%), respectively. Diuretics and angiotensin-converting enzyme inhibitors were most often prescribed for hypertension control (<140/90mmHg, achieved in 68% of men and 60% of women treated). Hypercholesterolemia was controlled (low-density lipoprotein cholesterol <130mg/dl) in just 31% of men and 26% of women with no history of cardiovascular disease, despite lipid-lowering treatment, primarily (90%) with statins. The percentage of women and men with DM2 and with glycated hemoglobin <7% was 64.7% and 59.2%, respectively; treatment was predominantly with oral hypoglycemic agents alone (70%), or combined with insulin (15%).
ConclusionsHypertension was the most prevalent cardiovascular risk factor in the Catalan population attended at primary care centers. About two thirds of individuals with hypertension or DM2 were adequately controlled; hypercholesterolemia control was particularly low.
Analizar la prevalencia, control y manejo de la hipertensión arterial, hipercolesterolemia y diabetes mellitus tipo 2.
DiseñoAnálisis transversal de todos los individuos atendidos en centros de atención primaria entre 2006 y 2009.
EmplazamientoSe extrajo de la historia clínica electrónica los antecedentes de enfermedad cardiovascular, el diagnóstico y tratamiento de la hipertensión arterial, hipercolesterolemia, diabetes mellitus tipo 2, el perfil lipídico, la glicemia y la presión arterial. Las prevalencias y las variables de manejo y control se estandarizaron por edad.
ParticipantesIndividuos de 35 a 74 años registrados en las bases de datos de atención primaria.
Mediciones principalesSe analizaron registros de 2.174.515 de individuos (47% hombres, edad media 52 años (DE 11)).
ResultadosLa hipertensión arterial fue el factor de riesgo más prevalente (39% en mujeres y 41% en hombres), seguido de la hipercolesterolemia (38% y 40%) y la diabetes mellitus tipo 2 (12% y 16%), respectivamente. Los diuréticos y los inhibidores de la enzima convertidora de angiotensina fueron los fármacos más frecuentemente recetados para el control de la presión arterial (68% de hombres y 60% de mujeres presentaron valores <140/90mmHg). Sólo el 31% de los hombres y el 26% de las mujeres sin antecedentes de enfermedad cardiovascular presentaron hipercolesterolemia controlada (colesterol de las lipoproteínas de baja densidad <130mg/dl), a pesar del porcentaje de tratamiento con estatinas (90%). EL porcentaje de mujeres y hombres con diabetes mellitus tipo 2 y hemoglobina glicada <7% era de 64.7% y 59.2%, respectivamente; el tratamiento se realizó predominantemente con antidiabéticos orales únicamente (70%) o asociados con insulina (15%).
ConclusionesLa hipertensión arterial fue el factor de riesgo cardiovascular más prevalente en población catalana atendida en centros de atención primaria. Alrededor de dos tercios de los individuos con hipertensión arterial o diabetes mellitus tipo 2 estaban adecuadamente controlados; mientras que el control de la hipercolesterolemia fue especialmente bajo.
Cardiovascular disease (CVD) causes 56million deaths annually all over the world and accounts for 30% of recorded deaths in developed countries.1 In Spain, CVD was responsible for one fourth of all deaths recorded in 2010.2 Atherosclerosis, the common cause of all CVDs, has a long, generally asymptomatic, induction period that often leads to an event such as myocardial infarction or stroke, with more than 35% mortality.3 The control of cardiovascular risk factors leads to a reduction in CVD incidence,4 making primary prevention of CVD a crucial issue in primary care. A better understanding of CVD mechanisms and the role of associated risk factors, particularly hypercholesterolemia, hypertension and diabetes mellitus type 2 (DM2), is essential to the design and implementation of the preventive public health interventions that are needed.5
Data routinely collected in primary care settings and stored in electronic medical records (EMR) databases have recently been validated for estimating the prevalence of cardiovascular risk factors in the general population in Spain.6 The strengths of this type of database are mainly based on the universal coverage of the Spanish National Health System, which guarantees a representative population, and the collection of clinical and treatment data by each individual's general practitioner and primary care nurse, increasing data quality and avoiding the inaccuracies inherent in self-reported data. EMR in the National Health System are stored in a centralized database that can be accessed by all health professionals. Recently, clinical decision support systems, such as the electronic clinical practice guidelines, have been integrated at several points in the EMR software.7 A two-steps project has been designed to analyze the impact of such interactive documents in the clinical management. The first phase of this study aimed to analyze the prevalence and control of three cardiovascular risk factors (hypercholesterolemia, hypertension, and DM2) before implementing the electronic clinical practice guidelines.8 These results can be compared with previous epidemiologic studies conducted in the same area. Indeed, major efforts have been made to estimate the prevalence of cardiovascular risk factors in Spain using general population samples collected for research purposes.9–11 However, the use of routinely collected data to create large databases suitable for research would better optimize the large amount of resources invested in our universal National Health System.
The objective of this study is to analyze the prevalence, control, and management of hypercholesterolemia, hypertension, and DM2 in individuals aged 35–74 years and attended by primary care centers in Catalonia between 2006 and 2009.
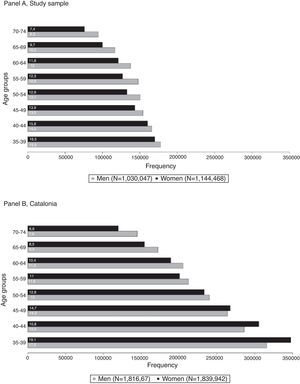
MethodsParticipantsThe cross-sectional design included all individuals aged 35–74 years attended in the primary care centers of the Catalan Institute of Health from January 2006 through December 2009. The study was conducted in Catalonia, a Mediterranean region in northeastern Spain. The protocol of study has been explained elsewhere.8
Briefly, within Spain's National Health System that serves every citizen, the Catalan Institute of Health administers a network of 279 primary care centers that serves approximately 80% of the Catalan population. Each individual is registered with a primary care team (general practitioner and nurse) in one of these publicly funded centers. As the main health provider for Catalonia, this network employs about 3500 primary care physicians and serves 5.8million patients.12
The protocol of the present study was approved by the primary care research arm of the Catalan Institute of Health, the Institut d’Investigació en Atenció Primària Jordi Gol Clinical Research Ethics Committee (authorization number P09/28).
Data managementAll personal identifiers were eliminated before EMR data were pooled and queried for patients seen between 2006 and 2009. The database contained the most recent information for each patient: age, sex, and the International Classification of Diseases (ICD) codes for hypertension, hypercholesterolemia, DM2, coronary heart disease, stroke, and peripheral artery disease. If available, values and dates for measurements of systolic and diastolic blood pressure, total cholesterol, low-density lipoprotein (LDL) cholesterol, high-density lipoprotein (HDL) cholesterol, triglycerides, glycemia, and glycated hemoglobin, along with information regarding smoking cessation, if applicable.
The Framingham risk score validated for Spain by the Girona Heart Registry researchers (Framingham-REGICOR)13 was calculated for records containing complete data (age, sex, DM2, systolic and diastolic blood pressure, total cholesterol, and HDL cholesterol) and no history of CVD. Using Framingham-REGICOR risk charts, a cut-off point of 10% was used as the indicator for hypercholesterolemia drug treatment.14
Variables analyzedHypertension, diabetes, and hypercholesterolemia were identified when diagnosis or treatment for these disorders was recorded between 2006 and 2009. These subsamples of participants were used for estimating the proportion of controlled patients for each disease. Optimal control of hypertension was considered if a record included a systolic blood pressure <140mmHg and diastolic blood pressure <90mmHg after diagnosis or treatment. Optimal control, suboptimal control, and uncontrolled diabetes was considered if an individual already diagnosed or treated presented with glycated hemoglobin <7%, ≥7% and <8% or ≥8%, respectively. Optimal control of hypercholesterolemia was considered when LDL-cholesterol was <100mg/dl in patients with CVD history or <130mg/dl in those with no CVD history and coronary risk ≥10% or cholesterol-lowering drug treatment.
Treatment characterizationThe most common groups of medications were considered: antihypertensive agents (diuretics, angiotensin-converting enzyme (ACE) inhibitors, beta-blockers, calcium channel blockers, angiotensin II receptor antagonists (ARA-II), alpha-blockers, central nervous system sympatholytics, and direct acting vasodilators); hypoglycemic agents (biguanide, sulfonylurea, alpha-glucosidase inhibitor, thiazolidinedione, dipeptidyl peptidase-4 inhibitors, other oral hypoglycemic agents and insulin); and lipid-lowering drugs (statins, fibrates, ion exchange resins, ezetimibes, other lipid-lowering agents). Within each disorder, we also described the percentage of individuals treated with the most common combinations of drugs.
Statistical analysisPrevalence is presented by sex and is standardized to the age distribution of the European population.15 Continuous variables are presented as mean and 95% confidence interval (CI), and categorical variables as proportions and 95%CI.
Missing values for 8 variables (smoking, total, LDL and HDL cholesterol, triglycerides, glucose, and systolic and diastolic blood pressure) were imputed from multivariate linear models of every missing variable as a function of sex, age, and the rest of variables fitted by the multiple imputation method.
Student T test was used to compare means of continuous variables and Chi-squared for proportions.
The R Statistical Package (R Foundation for Statistical Computing, Vienna, Austria; Version 2.15.0) and STATA software, version 12 (Stata Corp., College Station, TX, USA) were used for data analysis.
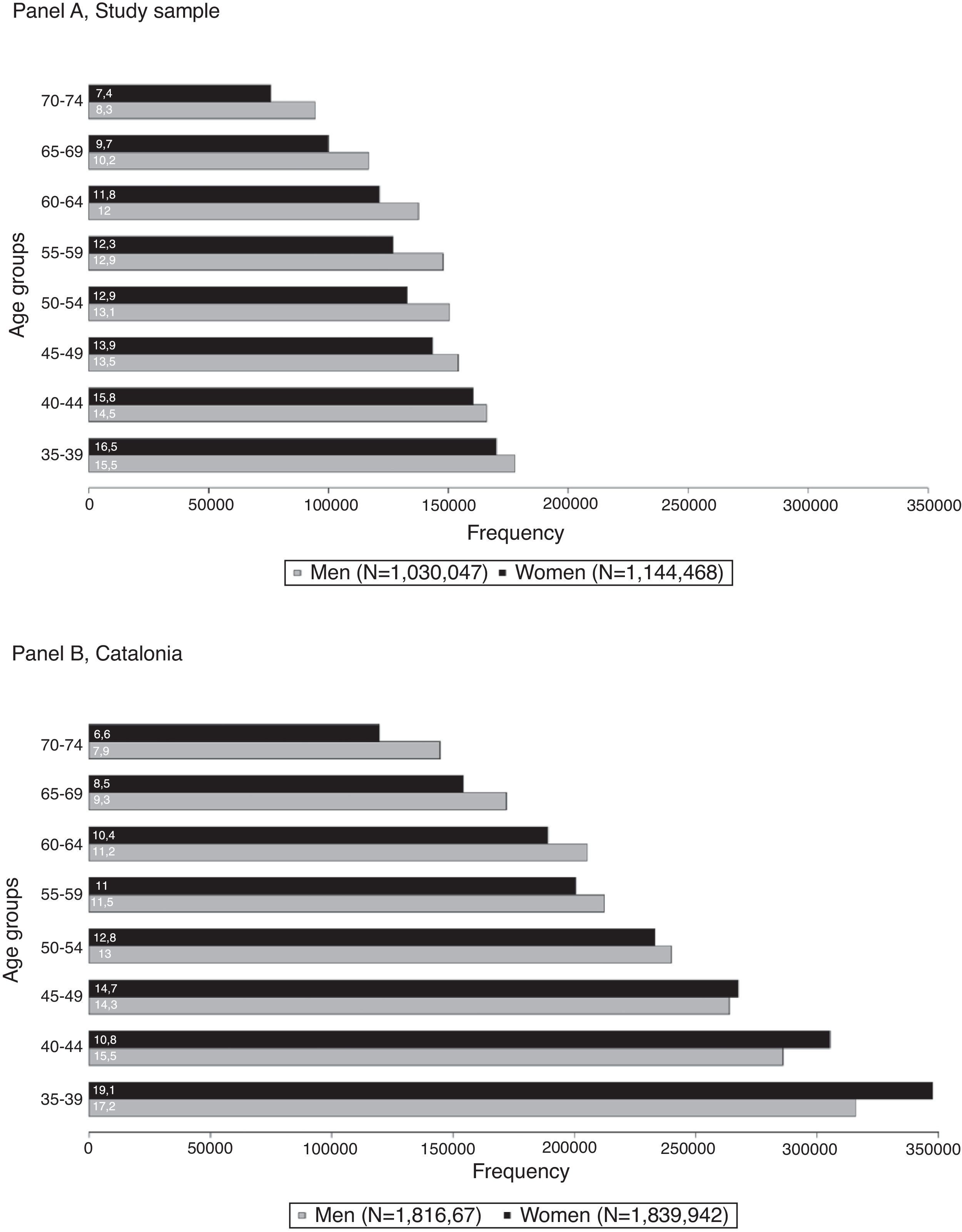
ResultsWe included 2,174,515 individuals, representing 59% of the Catalan population aged 35–74 years (Fig. 1), and 78% of the total number of these individuals assigned to primary care centers of the Catalan Institute of Health. The mean age of the sample was 52 years (SD 11) and 47% were men; in the assigned population, mean age was 51 years (SD 11) and 50% were men.
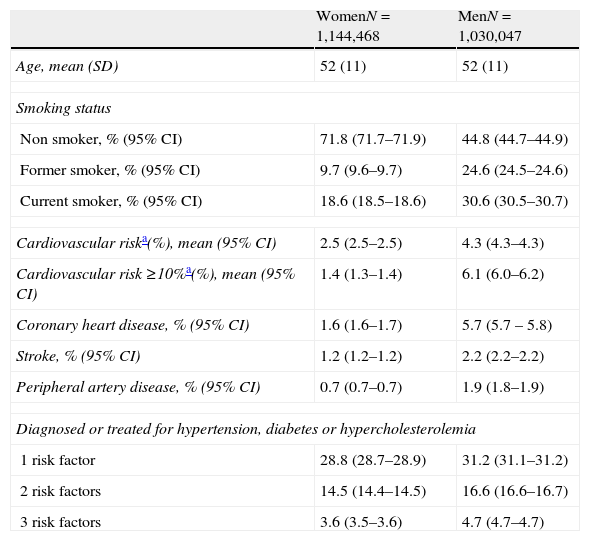
Men were more likely than women to be smokers and to have previous history of myocardial infarction, stroke or peripheral artery disease. The percentage of women and men with all three risk factors (hypertension, hypercholesterolemia and DM2) was 3.6% and 4.7%, respectively (Table 1).
Characteristics of individuals included in primary care electronic medical records, by sex and standardized to the European population.
| WomenN=1,144,468 | MenN=1,030,047 | |
| Age, mean (SD) | 52 (11) | 52 (11) |
| Smoking status | ||
| Non smoker, % (95% CI) | 71.8 (71.7–71.9) | 44.8 (44.7–44.9) |
| Former smoker, % (95% CI) | 9.7 (9.6–9.7) | 24.6 (24.5–24.6) |
| Current smoker, % (95% CI) | 18.6 (18.5–18.6) | 30.6 (30.5–30.7) |
| Cardiovascular riska(%), mean (95% CI) | 2.5 (2.5–2.5) | 4.3 (4.3–4.3) |
| Cardiovascular risk ≥10%a(%), mean (95% CI) | 1.4 (1.3–1.4) | 6.1 (6.0–6.2) |
| Coronary heart disease, % (95% CI) | 1.6 (1.6–1.7) | 5.7 (5.7 – 5.8) |
| Stroke, % (95% CI) | 1.2 (1.2–1.2) | 2.2 (2.2–2.2) |
| Peripheral artery disease, % (95% CI) | 0.7 (0.7–0.7) | 1.9 (1.8–1.9) |
| Diagnosed or treated for hypertension, diabetes or hypercholesterolemia | ||
| 1 risk factor | 28.8 (28.7–28.9) | 31.2 (31.1–31.2) |
| 2 risk factors | 14.5 (14.4–14.5) | 16.6 (16.6–16.7) |
| 3 risk factors | 3.6 (3.5–3.6) | 4.7 (4.7–4.7) |
CI, confidence interval.
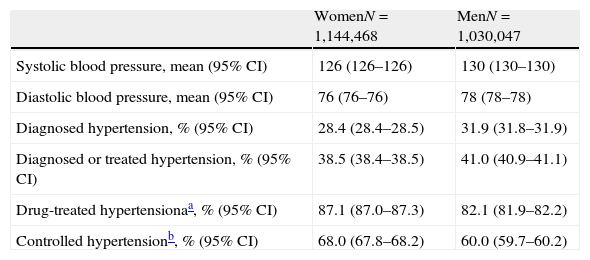
Hypertension was the most prevalent cardiovascular risk factor in both sexes. Although more prevalent in men, a significantly higher percentage of women were treated for hypertension and adequately controlled. About half of the patients treated were taking one drug; 18% of women and 21% of men were treated with three or more drugs. The most common prescriptions were diuretics (most often prescribed in women), ACE inhibitors (most often prescribed in men), or a combination of the two drugs (Table 2). Among those controlled for hypertension, 43.5% use one single drug, 33.8% used two drugs and the rest (22.7%) were treated with three or more drugs.
Prevalence of hypertension and characteristics of the population diagnosed with hypertension, by sex and standardized to the European population.
| WomenN=1,144,468 | MenN=1,030,047 | |
| Systolic blood pressure, mean (95% CI) | 126 (126–126) | 130 (130–130) |
| Diastolic blood pressure, mean (95% CI) | 76 (76–76) | 78 (78–78) |
| Diagnosed hypertension, % (95% CI) | 28.4 (28.4–28.5) | 31.9 (31.8–31.9) |
| Diagnosed or treated hypertension, % (95% CI) | 38.5 (38.4–38.5) | 41.0 (40.9–41.1) |
| Drug-treated hypertensionaa, % (95% CI) | 87.1 (87.0–87.3) | 82.1 (81.9–82.2) |
| Controlled hypertensionb, % (95% CI) | 68.0 (67.8–68.2) | 60.0 (59.7–60.2) |
| Treatments | WomenN=413,930 | MenN=365,867 |
| Diuretics, % (95% CI) | 53.6 (53.4–53.8) | 42.9 (42.7–43.1) |
| ACE inhibitors, % (95% CI) | 42.6 (42.4–42.8) | 53.0 (52.8–53.2) |
| Angiotensin II receptor antagonists, % (95% CI) | 22.8 (22.6–22.9) | 25.3 (25.1–25.5) |
| Beta-blockers, % (95% CI) | 31.3 (31.1–31.5) | 32.7 (32.5–32.9) |
| Calcium channel blockers, % (95% CI) | 19.7 (19.6–19.9) | 24.0 (23.8–24.2) |
| Alpha-blockers, % (95% CI) | 3.3 (3.2–3.3) | 6.1 (6.0–6.2) |
| Central nervous system sympatholytics, % (95% CI) | 0.5 (0.4–0.5) | 0.2 (0.2–0.2) |
| Direct acting vasodilators, % (95% CI) | 0.4 (0.3–0.4) | 0.4 (0.4–0.4) |
| Treated with 1 drug, % (95% CI) | 51.4 (51.2–51.6) | 46.8 (46.6–47.0) |
| Diuretic, % (95% CI) | 16.1 (15.9–16.2) | 7.7 (7.6–7.8) |
| ACE inhibitor, % (95% CI) | 13.4 (13.2–13.5) | 18.7 (18.6–18.9) |
| Angiotensin II receptor antagonist, % (95% CI) | 4.6 (4.5–4.7) | 5.5 (5.4–5.6) |
| Beta-blocker, % (95% CI) | 12.4 (12.2–12.5) | 9.8 (9.7–9.9) |
| Calcium channel blocker, % (95% CI) | 4.4 (4.3–4.5) | 4.2 (4.1–4.3) |
| Treated with 2 drugs, % (95% CI) | 30.8 (30.6–30.9) | 32.0 (31.8–32.1) |
| Diuretic+ACE inhibitor, % (95% CI) | 10.5 (10.4–10.6) | 9.3 (9.2–9.4) |
| Diuretic+angiotensin II receptor antagonist, % (95% CI) | 5.3 (5.2–5.4) | 4.5 (4.4–4.6) |
| Diuretic+beta-blocker, % (95% CI) | 4.3 (4.2–4.4) | 2.9 (2.9–3.0) |
| Diuretic+calcium channel blocker, % (95% CI) | 1.6 (1.6–1.7) | 1.2 (1.2–1.2) |
| ACE inhibitor+beta-blocker, % (95% CI) | 2.4 (2.3–2.4) | 4.4 (4.3–4.4) |
| ACE inhibitor+calcium channel blocker, % (95% CI) | 1.7 (1.7–1.7) | 2.7 (2.7–2.8) |
| Treated with ≥3 drugs, % (95% CI) | 17.9 (17.7–18.0) | 21.3 (21.1–21.4) |
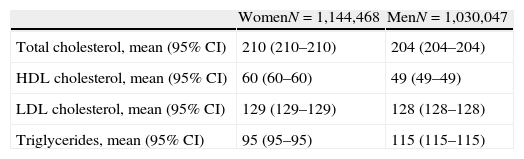
Regarding lipid profile, the non-standardized median triglyceride level was 100 and 121mg/dl in women and men, respectively (data not shown); standardized mean values were 95 and 115mg/dl. We would also note the high mean HDL cholesterol values observed for women (60mg/dl). Hypercholesterolemia was the most frequent cardiovascular risk factor and, after diagnosis, 54% of women and 59% of men were treated for this disorder. Despite high treatment adequacy (i.e., the percentage of women and men with cardiovascular risk ≥10% who received treatment was 79% and 74%, respectively), just 26% of women and 31% of men had well controlled (<130mg/dl) LDL-cholesterol. Furthermore, the percentage of controlled individuals with CVD history (LDL-cholesterol <100mg/dl) was 31% and 43% in women and men, respectively. Statins was by far the most frequently used lipid-lowering agent (Table 3).
Prevalence of hypercholesterolemia and characteristics of the population diagnosed with hypercholesterolemia, by sex and standardized to the European population.
| WomenN=1,144,468 | MenN=1,030,047 | |
| Total cholesterol, mean (95% CI) | 210 (210–210) | 204 (204–204) |
| HDL cholesterol, mean (95% CI) | 60 (60–60) | 49 (49–49) |
| LDL cholesterol, mean (95% CI) | 129 (129–129) | 128 (128–128) |
| Triglycerides, mean (95% CI) | 95 (95–95) | 115 (115–115) |
| Prevalence of diagnosed and controlled hypercholesterolemia | WomenN=1,144,468 | MenN=1,030,047 |
| Diagnosed hypercholesterolemia, % (95% CI) | 31.3 (31.2–31.4) | 32.8 (32.7–32.9) |
| Hypercholesterolemia or treatment, % (95% CI) | 37.5 (37.4–37.5) | 40.3 (40.3–40.4) |
| Drug-treated hypercholesterolemia, % (95% CI) | 54.3 (54.1–54.4) | 59.3 (59.2–59.5) |
| Drug-treated hypercholesterolemia in individuals with cardiovascular risk ≥10%, % (95% CI) | 79.1 (71.4–86.9) | 74.0 (72.3–75.7) |
| LDL cholesterol <130mg/dl,a % (95% CI) | 25.6 (25.5–25.8) | 31.4 (31.2–31.6) |
| LDL <100mg/dl in individuals with CVD, % (95% CI) | 30.6 (29.4–31.9) | 43.0 (42.4–43.7) |
| Characterization of hypercholesterolemia treatment | WomenN=281,210 | MenN=269,789 |
| Statin, % (95% CI) | 90.9 (90.7–91.1) | 87.2 (87.1–87.4) |
| Fibrate, % (95% CI) | 12.0 (11.8–12.2) | 20.4 (20.2–20.6) |
| Ezetimibe, % (95% CI) | 4.4 (4.2–4.5) | 4.9 (4.8–5.0) |
| Ion exchange resin, % (95% CI) | 1.6 (1.5–1.7) | 0.9 (0.8–0.9) |
| Other lipid-lowering agents, % (95% CI) | 2.4 (2.3–2.5) | 3.4 (3.3–3.4) |
| Treated with 1 drug, % (95% CI) | 89.9 (89.7–90.0) | 85.4 (85.2–85.6) |
| Statin, % (95% CI) | 81.2 (80.9–81.4) | 73.3 (73.0–73.5) |
| Fibrate, % (95% CI) | 6.1 (5.9–6.2) | 10.7 (10.5–10.9) |
| Ezetimibe, % (95% CI) | 0.9 (0.8–0.9) | 0.5 (0.4–0.5) |
| Ion exchange resin, % (95% CI) | 1.0 (0.9–1.1) | 0.4 (0.4–0.4) |
| Treated with 2 drugs, % (95% CI) | 9.0 (8.9–9.2) | 12.7 (12.5–12.8) |
| Statin+fibrate, % (95% CI) | 4.8 (4.6–4.9) | 7.5 (7.4–7.6) |
| Statin+ezetimibe, % (95% CI) | 2.6 (2.6–2.7) | 3.1 (3.0–3.2) |
| Statin+ion exchange resin, % (95% CI) | 0.4 (0.4–0.4) | 0.3 (0.2–0.3) |
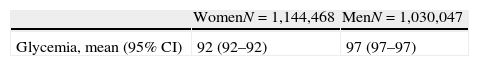
Diabetes mellitus type 2 was more prevalent in men than in women, although women were more often treated and a higher percentage achieved optimal glycemic control (glycated hemoglobin <7%). In addition, 60% and 66% of women and men with diabetes presented LDL cholesterol levels <130mg/dl, respectively. The percentages for controlled hypertension in this population were 69% for women and 63% for men. Approximately 70% of treated individuals received oral hypoglycemic agents alone; 15% received both oral hypoglycemic agents and insulin (Table 4).
Prevalence of diabetes mellitus type 2 and characteristics of the population diagnosed with diabetes mellitus type 2, by sex and standardized to the European population.
| WomenN=1,144,468 | MenN=1,030,047 | |
| Glycemia, mean (95% CI) | 92 (92–92) | 97 (97–97) |
| Prevalence of diagnosed and controlled diabetes | WomenN=1,144,468 | MenN=1,030,047 |
| Diagnosed diabetes, % (95% CI) | 8.8 (8.7–8.8) | 13.8 (13.8–13.9) |
| Diagnosed or treated diabetes, % (95% CI) | 11.8 (11.7–11.8) | 16.2 (16.1–16.2) |
| Drug-treated diabetes, % (95% CI) | 77.8 (77.5–78.1) | 72.2 (71.9–72.4) |
| Glycated hemoglobin,a % (95% CI) | 6.8 (6.8–6.8) | 7.0 (7.0–7.0) |
| Glycated hemoglobin <7%,a % (95% CI) | 64.7 (64.2–65.1) | 59.2 (58.8–59.6) |
| Glycated hemoglobin 7–7.9%,a % (95% CI) | 15.3 (15.0–15.7) | 17.0 (16.8–17.3) |
| Glycated hemoglobin ≥8%,a % (95% CI) | 20.0 (19.6–20.4) | 23.8 (23.4–24.1) |
| Characterization of diabetes treatment | WomenN=113,247 | MenN=125,479 |
| Biguanide, % (95% CI) | 72.8 (72.4–73.1) | 76.4 (76.1–76.7) |
| Sulfonylurea, % (95% CI) | 33.1 (32.7–33.5) | 37.2 (36.8–37.5) |
| Insulin, % (95% CI) | 30.7 (30.3–31.1) | 28.4 (28.1–28.7) |
| Thiazolidinedione, % (95% CI) | 4.6 (4.5–4.8) | 4.2 (4.0–4.3) |
| Alpha-glucosidase inhibitor, % (95% CI) | 3.2 (3.1–3.4) | 3.2 (3.1–3.3) |
| DPP-4 inhibitor, % (95% CI) | 2.6 (2.5–2.7) | 2.6 (2.5–2.7) |
| Other hypoglycemic agents, % (95% CI) | 8.9 (8.6–9.1) | 7.8 (7.6–8.0) |
| Oral hypoglycemic agents, % (95% CI) | 69.3 (68.9–69.7) | 71.6 (71.3–71.9) |
| Oral hypoglycemic agents and insulin, % (95% CI) | 15.5 (15.3–15.8) | 15.6 (15.4–15.9) |
| Treated with 1 drug, % (95% CI) | 60.2 (59.8–60.6) | 56.2 (55.9–56.6) |
| Treated with 2 drugs, % (95% CI) | 27.4 (27–27.7) | 31.2 (30.9–31.5) |
| Treated with ≥3 drugs, % (95% CI) | 12.4 (12.2–12.6) | 12.6 (12.4–12.8) |
CI, confidence interval; DPP-4, dipeptidyl peptidase-4.
Finally, 17% out of 44,481 women and 19% out of 49,115 men diagnosed with all three diseases presented an optimal control for all three (systolic and diastolic blood pressure <140/90mmHg, glycated hemoglobin <7% and LDL-cholesterol <130mg/dl and <100mg/dl for individuals in primary and secondary prevention, respectively).
DiscussionThis analysis of more than 2.1million individual EMR from primary care centers in Catalonia identified hypertension as the most prevalent cardiovascular risk factor (38% in women and 41% in men), followed by hypercholesterolemia (37% and 40%) and DM2 (12% and 16%), respectively. The control of cardiovascular risk factors was acceptable (>60%) for hypertension and DM2, but low for those diagnosed with hypercholesterolemia (<40 and <30% in those with and without CVD history, respectively). In all cases, the most frequently used drugs concurred with the recommendations of current clinical practice guidelines.16–18 The role of primary care is crucial to the control of chronic disorders in the community. Our results indicate that there is room for improvement in optimal control of the cardiovascular risk factors, not only at a population level but also in the most vulnerable groups, which contain a high proportion of the population CVD risk. Population risk should be based on the best available methods (i.e., coronary risk charts) to focus public health efforts efficiently while achieving the largest population health benefit.19
Comparison with previous studiesThe estimated prevalence of hypertension and diabetes diagnosis and treatment in our study was similar to that observed in previous nationwide epidemiological studies.9,10,20 However, comparisons for hypercholesterolemia are difficult because different thresholds are used to diagnose or treat this disorder.9,10,21,22
The outstanding mean value of HDL cholesterol in Catalan women (60mg/dl) concurs with the DARIOS Study results.10 This protective factor may be related to the low incidence of myocardial infarction observed in the female population in South Europe,23,24 and should considered in the design and implementation of prevention strategies in the region. Finally, CVD risk should be estimated with instruments validated for the population.25
Notably, treatment profiles for all three disorders studied followed the recommendations described in the most updated, evidence-based, clinical practice guidelines.16–18 These guidelines (accessible via the EMR system) standardize procedures, reduce unjustified variations in clinical practice, and encourage physician behavior that promotes interventions supported by the best evidence available.26,27 However, the low control of hypercholesterolemia, as measured with LDL cholesterol, must be highlighted. Despite statin therapy in 90% of individuals diagnosed with hypercholesterolemia, less than one third of individuals requiring primary prevention of CVD had LDL-cholesterol <130mg/dl. These results were only slightly better when we calculated the proportion of individuals with history of CVD and LDL-cholesterol below the recommended threshold (<100mg/dl). Indeed, the 2004 LIPICAP Study, which included primary care patients diagnosed with hypercholesterolemia, reports similar results.28
On the other hand, the control of hypertension and diabetes was higher than that previously reported and could reflect the implementation of more efficient strategies of controlling cardiovascular risk factors in primary care settings.29,30 In our study, diuretics and ACE inhibitors were the most used antihypertensive agents, as recommended in clinical practice guidelines.16 However, ARA-II was the most frequently prescribed in the PRESCAP 2006 Study.29 In addition, the proportion of women with controlled hypertension was higher than in men. These results concurred with those observed in previous Spanish population-based studies.10,31 The high proportion of individuals controlled and treated with just one drug for hypertension compared with previous studies could be due to the age of the participants included (i.e., up to 74 years).32 On the other hand, biguanide and sulfonylurea were the most frequently used drugs in our study for managing DM2. The UKPDS study highlighted the effects of both drugs for controlling glucose levels.33 In addition, more than 40% of individuals with diabetes were treated with 2 or more drugs, concurring with eControl study results in Catalonia, which included almost 290,000 individuals with diabetes mellitus aged 30–89 years,34 and with the SFIDA study conducted in Italy.35
Use of primary care computerized registries for researchComputerization of primary care EMRs has made available large volumes of routinely collected data. Integrating clinical decision support systems (e.g., electronic clinical practice guidelines) in EMR should improve clinical outcomes, patient safety, particularly important for improving the management of chronic diseases.36 In addition, avoid duplication of tests, audit the effectiveness of care and finally provide data for research.37 Indeed, an increasing number of studies have used EMR databases to assess the prevalence and control of cardiovascular risk factors.6,38–40
The results of these studies may help to improve both the pharmacological and non-pharmacological interventions recommended for CVD prevention. The objective is to increase the opportunities to avert or at least slow down the clinical expression of atherosclerosis in the general population. New knowledge may help to produce evidence-based documents to guide health professionals’ actions. Indeed, the most recently released clinical practice guidelines for all three disorders described in the present study (hypercholesterolemia, hypertension and diabetes) have been integrated with our EMR system.16–18
Characteristics and limitations of the studyThe present study was conducted in primary care settings in Catalonia. The sample represents 59% of the total population of this area (and 78% of those attending Catalan Health Institute primary care centers), aged 35–74 years. Older individuals were excluded from analysis because we aimed to know the mean cardiovascular risk of the population, which cannot be estimated by Framingham REGICOR in those older than 75 years. On the one hand, individuals attended in primary care could have more pathologies than the non-attended population. However, the universal coverage of our public health system minimizes these differences. On the other hand, the differences between studies in the observed prevalences, estimated using the recorded diagnosis or diagnosis and treatment, may reflect some problems in the quality of the records used. However, in our case the previous validation of this database minimizes potential problems related to underreported data.6,41 In addition, high-quality reporting is key not only to ensure better quality of care for patients but also to improve databases that could have great potential for epidemiological studies and population comparisons. Further studies are planned for analyzing the treatments for hypertension, diabetes mellitus type 2 and hypercholesterolemia in depth.
In conclusion, hypertension was the most common cardiovascular risk factor in the Catalan population aged 35–74 years, followed by hypercholesterolemia and diabetes. Diuretics and ACE inhibitors were the most common drugs used to treat hypertension; biguanides and statins were most often used for treating diabetes and hypercholesterolemia, respectively. Good control was achieved in approximately two thirds of hypertensive patients (68% of women and 66% of men), as well as two thirds of women and more than half of men diagnosed with diabetes (65% and 59%); however, closer to one third of patients, with and without history of CVD, had adequately controlled hypercholesterolemia.
- •
Major efforts have been made to estimate the prevalence of cardiovascular risk factors in Spain using general population samples collected for research purposes.
- •
The use of routinely collected data to create large databases suitable for research could optimize the large amount of resources invested in our universal National Health System.
- •
Hypertension was the most prevalent cardiovascular risk factor, followed by hypercholesterolemia and diabetes mellitus type 2.
- •
The most recently released clinical practice guidelines for all three disorders have been integrated with our electronic medical record system.
This project was supported by a grant from the Agència d’Informació, Avaluació i Qualitat en Salut (grant number: 483/13/2009). Dr. Grau was funded by grants from Health Institute Carlos III-FEDER, Spain (Miguel Servet CP12/03287).
Conflicts of interestThe authors declare no conflicts of interest.
Members of the @GPC-ICS Group: Ester Amado, Arantxa Catalán-Ramos, Ramon Ciurana, Eva Comin, Alicia Consola, Xavier Cos, Josep Davins, Alicia Franzi, Eva Frigola, María Grau, Manuel Iglesias-Rodal, Manel Mata, Angels Pons, José Luis del Val García, Jose Mª Verdu.
The authors would like to thank Xavier Basagaña and Isaac Subirana for the statistical review. We appreciate the revision of the English text by Elaine Lilly, Ph.D., of Writer's First Aid.