Osteoporosis (OP) is a condition characterized by loss of bone mass and resistance with increased risk of fractures.1 Bone deterioration can occur over a number of years without presenting any symptoms. If detected when fracture appear, the disease is already advanced. The most common OP associated fractures sites are hip, spine and wrist. The diagnostic tool to evaluate bone mineral density (BMD) is DEXA (dual energy X-ray absorptiometry) by which nowadays it is possible to applied a new software that quantifies a parameter, reflection of the structural bone condition: Trabecular Bone Score (TBS).2 TBS is strongly correlated with the number of trabeculae and their connectivity and negatively with the space between trabeculae. High TBS value means that microarchitecture bone is dense, well connected with little spaces between trabeculaes. Conversely, a low TBS value means that the microarchitecture of bone is incomplete and poorly connected with wide spaces between trabeculae.3
Osteoporotic fractures represent a major cause of morbidity and disability in elderly, so OP is increasingly a disease of social importance. The general practitioner (GP) plays an essential role for early OP diagnosis, of crucial importance for fractures prevention. We describe clinical, demographic and pharmacological characteristics of post-menopausal women suffering from vertebral fractures attending a primary care center in three years (1st November 2015–1st November 2018). Clinical parameters are shown in Table 1. Attended GP's surgery 1300 patients, 550 males and 750 females, 55% of whom in menopause (412), 21 of them presented an osteoporotic vertebral fracture in these three years (5%).
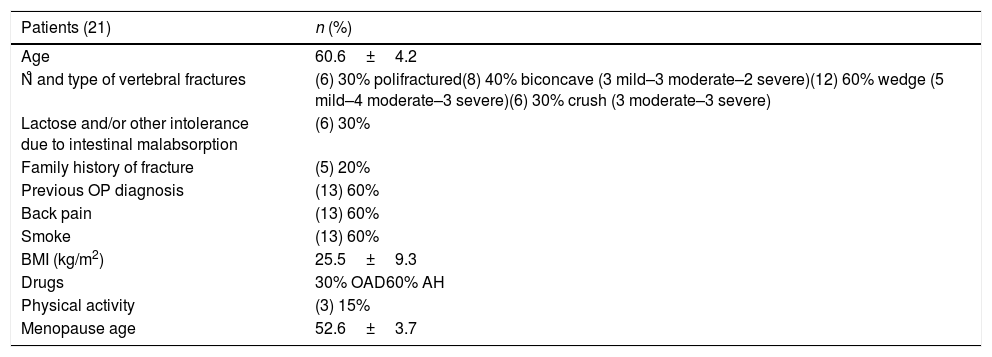
Clinical parameters of recruited women, including age, menopausal age, type and severity of vertebral fractures (Genant's method) and some risks factors for OP.
| Patients (21) | n (%) |
|---|---|
| Age | 60.6±4.2 |
| N̊ and type of vertebral fractures | (6) 30% polifractured(8) 40% biconcave (3 mild–3 moderate–2 severe)(12) 60% wedge (5 mild–4 moderate–3 severe)(6) 30% crush (3 moderate–3 severe) |
| Lactose and/or other intolerance due to intestinal malabsorption | (6) 30% |
| Family history of fracture | (5) 20% |
| Previous OP diagnosis | (13) 60% |
| Back pain | (13) 60% |
| Smoke | (13) 60% |
| BMI (kg/m2) | 25.5±9.3 |
| Drugs | 30% OAD60% AH |
| Physical activity | (3) 15% |
| Menopause age | 52.6±3.7 |
OAD, oral anti-diabetic; AH, anti-hypertensive.
Only 15% of women with vertebral fracture practiced physical activity and 60% smoked. All theme assumed colecalciferol and (60%) 13 women had a previous OP diagnosis, but due to poor compliance 6 of them had stopped bisphosphonate therapy. Some patients, despite significant differences in terms of BMD, presented similar TBS values. 6 subjects (30%), despite the normal BMD values, suffered atraumatic fractures. Therefore, the quantitative parameter must be integrated with the qualitative one. Moreover major BMI correlated with greater bone fragility and both qualitative and quantitative parameters did not correlate with serum 25OH-VitaminD levels. Vitamin-D alone is not able to prevent OP and reduce fracture risk; it would be important to prevent bone fragility by doing physical activity and abolishing smoking instead. Furthermore, this case-series analysis revealed the poor adherence to anti-absorptive therapy, because OP is a silent disease. As several factors influence risk of fractures, it's important to know validated algorithms for fracture estimation,4 but even these one present some weak points. Important risk factors are not considered in the most common algorithms, such as the risk of falls, physical activity, 25OH-D deficiency, and some important laboratory tests are not taken into consideration such as bone remodeling markers. This is important to establish the fracture risk threshold to considered for setting the treatment threshold. Is interesting to note that 10% (2) post-menopausal women had never underwent DEXA before the appearance of fracture. So GP role is essential to screen patients for DEXA, to emphasize the importance of lifestyles, to address bone specialist not only patients with densitometric OP diagnosis, but also those who present risk factors for OP in order to keep them under strict control, to immediately start therapy. GP has to note not only the quantitative BMD value, but the qualitative one too. TBS value, in fact, in combination with BMD, increase the number of patients at risk correctly identified. Moreover GP is the only one who can increase awareness of the importance of therapy adherence, because of his strict relationship with patients.
Financial supportThere is not financial support.
Conflicts of interestThere are not conflicts of interest. All authors are responsible for the entire content of the letter.