Aims to describe the initial symptoms most related to the prognosis of Covid-19.
DesignThis is a retrospective cross sectional, quantitative, data analyzed study.
SiteThis study was made in the family medicine centers (n=82) of Çorlu district of Tekirdağ province, in Turkey.
ParticipantsThe study included patients (n=1.506) who had a positive PCR test for Covid-19 from March to September 2020. And we asked them their initial symptoms which bring them to the family medicine centers before the test.
Main measurementsThe participants’ age, gender, presence of chronic disease, and initial symptoms which they come to a healthcare facility were evaluated. These variables were analyzed in terms of length of hospital stay, intensive care unit admission and mortality rates.
ResultsThe most common initial symptom in Covid-19 patients was cough. The presence of a chronic disease, the shortness of breath, malaise, the loss of smell and taste, and vomiting were found to be associated with an increased mortality rate. Advanced age, the presence of cough, malaise, the loss of smell and taste, and vomiting as the initial symptoms were found to have increased the likelihood of being admitted to the intensive care unit.
ConclusionsThe authors advise placing more attention on the initial symptoms of cough, malaise, the loss of smell and taste and vomiting in Covid-19 patients. Because these symptoms are related with severe prognosis indicators.
Describir los síntomas iniciales más relacionados con el pronóstico de COVID-19.
DiseñoEste es un estudio retrospectivo de análisis de datos transversales, cuantificativos.
EmplazamientoEste estudio se realizó en los centros de medicina familiar (n=82) del distrito de Çorlu de la proviencia de Tekirdağ, en Turquía.
ParticipantesEl estudio incluyó pacientes (n=1.506) que tuvieron una prueba de PCR positiva para COVID-19 de marzo a septiembre de 2020. Se les preguntaron sus síntomas iniciales que los llevan a los centros de medicina familiar antes de la prueba.
Mediciones principalesSe evaluaron la edad, el sexo, la presencia de enfermedad crónica y los síntomas iniciales de los participantes que llegaron a un centro de atención médica. Estas variables se analizaron en términos de duración de la estancia hospitalaria, ingreso a la unidad de cuidados intensivos y tasas de mortalidad.
ResultadosEl síntoma inicial de presentación más común en los pacientes con COVID-19 fue la tos. La presencia de una enfermedad crónica, la falta de aliento, el malestar, la pérdida de olor y sabor y los vómitos se asociaron a una mayor tasa de mortalidad. La edad avanzada, la presencia de tos, malestar, la pérdida de olor y sabor, y vómitos fueron los síntomas iniciales que se encontraron para incrementar la probabilidad de ser admitido en la unidad de cuidados intensivos.
ConclusionesLos autores aconsejan prestar más atención a los síntomas iniciales de tos, malestar, pérdida de olor y sabor y vómitos en pacientes con COVID-19, porque estos síntomas están relacionados con indicadores de pronóstico severo.
Most important tool the scientists have in the fight against the Covid-19 pandemic at the moment is diagnosing the patients at the early disease stages and taking the required isolation measures. The isolation of the infected patients from the community can thereby prevent the disease spread.1
The identification of SARS-CoV-2 RNA by real-time reverse transcriptase-polymerase chain reaction (RT-PCR) testing of nasopharyngeal and oropharyngeal swabs is used as the gold standard diagnostic method. However, the knowledge and the precise interpretation of the initial patient complaints and symptoms associated with the coronavirus infection are essential due to the high cost of diagnostic tests, the difficulties faced by the patients in accessing the test facilities, the insufficient number of the employees working in Covid-19 testing, and the fact that Covid-19 tests are not 100% accurate.2
In the first few months of the pandemic in Turkey, the patients presenting with fever and respiratory symptoms (cough, shortness of breath) in addition to the travel history, the high risk of occupational exposure, and the history of contact with Covid-19 patients were diagnosed by Covid-19 testing in the hospitals in the provinces and the districts.3 In the following months, symptoms related to the involvement of body systems other than the respiratory system (nausea, vomiting, the loss of smell and taste, abdominal pain, and diarrhea) were also observed in the infected patients. The recognition and the precise interpretation of initial presenting symptoms and complaints to avoid the risk of overlooking the disease manifestations in various body systems and knowing the effects of these symptoms and complaints on prognosis are of great importance concerning the isolation and the follow-up of the infected patients.
The present study aims to help clinicians improve their recognition of Covid-19. The study also aims to describe the initial symptoms most related to the prognosis of Covid-19. The study intends to help the clinicians set diagnostic criteria that would suggest a high index of suspicion for Covid-19 by determining how these relations affect prognosis, and foresee the possible prognosis in an individual patient, and finally contribute to the literature data about the efficient use of diagnostic tests in health facilities of countries with limited test opportunities.
Material and methodsThis is a retrospective cross sectional, quantitative, data analyzed study. The universe of the study was composed of all patients in the Çorlu district who tested positive for Covid-19 using PCR testing, the gold standard method in diagnosing coronavirus infection, between March 2020 and the end of September 2020 (n=1.506). This study was made in the family medicine centers (n=82) of Çorlu district of Tekirdağ province, in Turkey. Çorlu district is in the west of Turkey. It is a district with a population of approximately 350 thousand, and where industries and factories are concentrated. The patients with ground-glass opacities on thoracic computed tomography (CT) scans considered the radiological manifestations of Covid-19, and the symptomatic patients with a negative PCR test were excluded from the study. The participating patients were grouped according to the sociodemographic characteristics such as age, gender, and the presence of chronic diseases. The patients were stratified according to the age groups in line with the age stratification used by the Turkish Ministry of Health in declaring the Covid-19 statistics to the public: 0–5 years young children (high risk for Covid-19 prognosis), 6–13 years (older children), 14–24 years (young adults), 25–49 years (adults), 50–64 years (older adults), and 65 years and older (older people).4 The presence of chronic diseases in the participating patients was grouped as follows: cardiovascular diseases, respiratory diseases, endocrine and metabolism disorders, rheumatic diseases, neurological diseases, and others. The other group includes the conditions involving the systems other than those stated above and lasting more than six months. The status of chronic disease presence of the participants was determined according to the chronic diseases defined in their personal e-nabız systems. e-nabız system; It is the database of the Ministry of Health of the Republic of Turkey where personal health data are registered but can be viewed by doctors with the consent of the individuals. The chronic disease status of the participants was taken from this database.
The initial symptoms and complaints of the participating the patients upon presenting to the healthcare facilities were questioned. The symptoms were grouped as follows: fever, cough, pain (muscle and joint pain, headache, sore throat, pain radiating to the back, and chest pain), malaise, the loss of smell and taste, diarrhea, nausea, vomiting, and expectoration. The initial symptoms and complaints were taken from the family medicine center data records arranged at the patients’ first application to the health institution.
The length of hospital stay, the admission to the intensive care unit, and mortality data were retrieved from the hospital records to evaluate prognosis, retrospectively. During this evaluation, the patients were categorized into two groups as the patients with a length of hospital stay of 14 days or shorter and the patients with a length of hospital stay of longer than 14 days, based on the official quarantine period of 14 days in Turkey. The statistical analysis was performed using SPSS (Version 25.0, IBM, Chicago, IL, USA) software package. Basic patient characteristics were expressed using descriptive statistics. A chi-square test was used in the comparison of categorical variables. A binary logistic regression analysis was used to determine the effects of symptoms on the admission to the intensive care unit, mortality, and length of hospital stay. The variables that were found to be significant between the groups were included in the multiple regression analysis. Multivariate regression analysis method was used here. The odds ratio was given with a confidence interval (CI) of 95% on the regression table. A p-value of less than 0.05 was considered statistically significant.
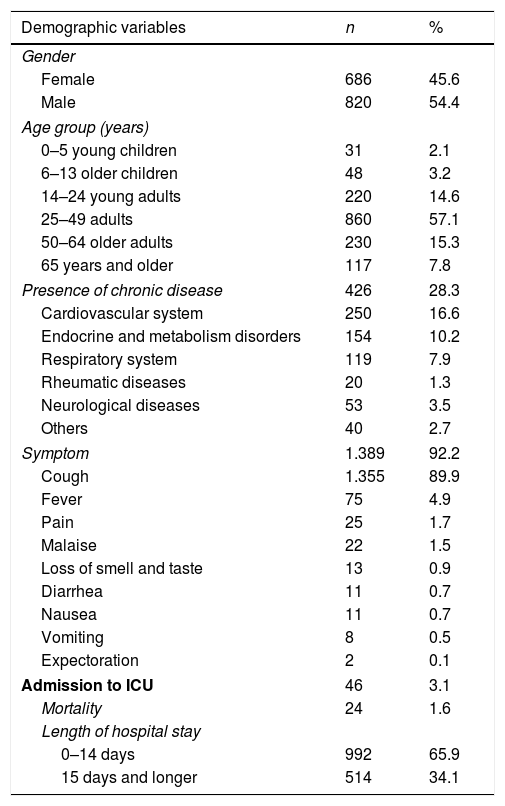
ResultsThe mean age of the study participants was 38.6±16.5 years (min: 1, max: 87). Of these patients, 28.3% (n=426) had one or more chronic diseases. Of the participating patients, 92.2% had at least one or more symptoms (n=1.389). Of all participating patients with positive Covid-19 PCR test, 3.1% (n=46) were admitted to the intensive care unit, and 1.6% (n=24) died. The mean length of the hospital stay of the patients was 13.4±5.9 (min: 1, max: 83) days. The analysis of sociodemographic features of the study patients is presented in Table 1. According to this table, Covid-19 most commonly occurred in adults aged 25–64 years whereas the disease occurred in all age groups. The most common presenting symptom in Covid-19 patients was cough (89.9%, n=1.355). The frequency distribution of other symptoms is presented in Table 1.
Sociodemographic characteristics of Covid-19 patients with a positive PCR test, frequency of presenting symptoms, length of hospital stay, and the rates of admission to intensive care unit and mortality.
| Demographic variables | n | % |
|---|---|---|
| Gender | ||
| Female | 686 | 45.6 |
| Male | 820 | 54.4 |
| Age group (years) | ||
| 0–5 young children | 31 | 2.1 |
| 6–13 older children | 48 | 3.2 |
| 14–24 young adults | 220 | 14.6 |
| 25–49 adults | 860 | 57.1 |
| 50–64 older adults | 230 | 15.3 |
| 65 years and older | 117 | 7.8 |
| Presence of chronic disease | 426 | 28.3 |
| Cardiovascular system | 250 | 16.6 |
| Endocrine and metabolism disorders | 154 | 10.2 |
| Respiratory system | 119 | 7.9 |
| Rheumatic diseases | 20 | 1.3 |
| Neurological diseases | 53 | 3.5 |
| Others | 40 | 2.7 |
| Symptom | 1.389 | 92.2 |
| Cough | 1.355 | 89.9 |
| Fever | 75 | 4.9 |
| Pain | 25 | 1.7 |
| Malaise | 22 | 1.5 |
| Loss of smell and taste | 13 | 0.9 |
| Diarrhea | 11 | 0.7 |
| Nausea | 11 | 0.7 |
| Vomiting | 8 | 0.5 |
| Expectoration | 2 | 0.1 |
| Admission to ICU | 46 | 3.1 |
| Mortality | 24 | 1.6 |
| Length of hospital stay | ||
| 0–14 days | 992 | 65.9 |
| 15 days and longer | 514 | 34.1 |
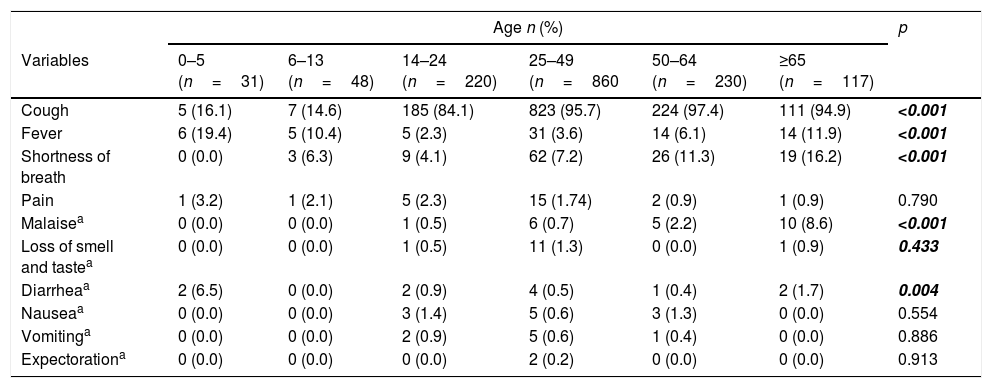
The analysis of the distribution of the presenting symptoms and the complaints of the Covid-19 patients across the age groups was showed in Table 2. According to this table cough was uncommon in the 0–14 age group while the frequency of cough increased with increasing age (p<0.001). The frequency of fever was significantly higher in the 0–5 age group and the patients aged 65 years and older compared to that in the other age groups (p<0.001). The shortness of breath was rarely observed in children aged 0–14 years while the frequency of this symptom significantly increased with increasing age (p<0.001). The presenting complaints of Covid-19 patients did not vary according to gender while only vomiting was more frequent in females (87.5%) than in males (12.5%) (p=0.017).
The analysis of the distribution of the presenting symptoms and complaints across the age groups in Covid-19 patients with a positive PCR test.
| Age n (%) | p | ||||||
|---|---|---|---|---|---|---|---|
| Variables | 0–5 (n=31) | 6–13 (n=48) | 14–24 (n=220) | 25–49 (n=860 | 50–64 (n=230) | ≥65 (n=117) | |
| Cough | 5 (16.1) | 7 (14.6) | 185 (84.1) | 823 (95.7) | 224 (97.4) | 111 (94.9) | <0.001 |
| Fever | 6 (19.4) | 5 (10.4) | 5 (2.3) | 31 (3.6) | 14 (6.1) | 14 (11.9) | <0.001 |
| Shortness of breath | 0 (0.0) | 3 (6.3) | 9 (4.1) | 62 (7.2) | 26 (11.3) | 19 (16.2) | <0.001 |
| Pain | 1 (3.2) | 1 (2.1) | 5 (2.3) | 15 (1.74) | 2 (0.9) | 1 (0.9) | 0.790 |
| Malaisea | 0 (0.0) | 0 (0.0) | 1 (0.5) | 6 (0.7) | 5 (2.2) | 10 (8.6) | <0.001 |
| Loss of smell and tastea | 0 (0.0) | 0 (0.0) | 1 (0.5) | 11 (1.3) | 0 (0.0) | 1 (0.9) | 0.433 |
| Diarrheaa | 2 (6.5) | 0 (0.0) | 2 (0.9) | 4 (0.5) | 1 (0.4) | 2 (1.7) | 0.004 |
| Nauseaa | 0 (0.0) | 0 (0.0) | 3 (1.4) | 5 (0.6) | 3 (1.3) | 0 (0.0) | 0.554 |
| Vomitinga | 0 (0.0) | 0 (0.0) | 2 (0.9) | 5 (0.6) | 1 (0.4) | 0 (0.0) | 0.886 |
| Expectorationa | 0 (0.0) | 0 (0.0) | 0 (0.0) | 2 (0.2) | 0 (0.0) | 0 (0.0) | 0.913 |
Chi-Square test.
The frequency of cough, fever, shortness of breath, and malaise as the initial symptoms in Covid-19 patients with a positive PCR test were significantly higher among patients with a chronic disease than the other patients Cough was seen in 95.3% of patients with chronic disease, while the rate of incidence in those without chronic disease was 87.9% (p<0.001). Fever was seen in 8.2% of patients with chronic disease, while the rate of incidence in others was 3.7% (p<0.001). While the rate of shortness of breath as the initial symptom in patients with chronic disease was 27.9%, it was 0.0% in those without chronic disease (p<0.001). While the rate of malaise as the initial symptom in patients with chronic disease was 3.1%, this rate was 0.1% in those without chronic disease (p<0.001).
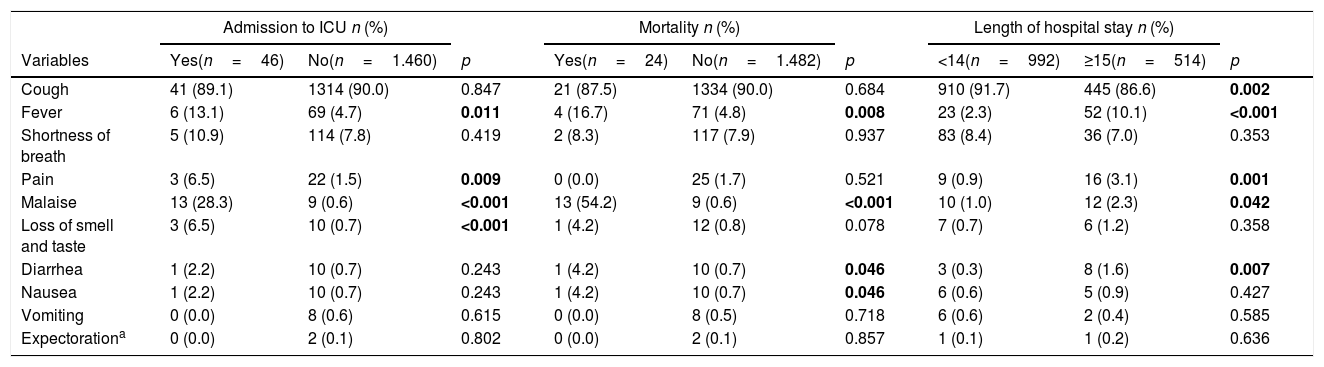
The analysis of the relationship between initial symptoms of Covid-19 patients and the length of hospital stay, the admission to the intensive care unit, and mortality revealed that the length of hospital stay was longer than 14 days in the patients with fever, pain, malaise, and diarrhea (p<0.001, p<0.001, p=0.042, and p=0.007, respectively). In contrast, the patients with a cough had a hospital stay shorter than 14 days (p=0.002) (Table 3).
The relationship between the initial symptoms and prognostic markers in Covid-19 patients.
| Admission to ICU n (%) | Mortality n (%) | Length of hospital stay n (%) | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Variables | Yes(n=46) | No(n=1.460) | p | Yes(n=24) | No(n=1.482) | p | <14(n=992) | ≥15(n=514) | p |
| Cough | 41 (89.1) | 1314 (90.0) | 0.847 | 21 (87.5) | 1334 (90.0) | 0.684 | 910 (91.7) | 445 (86.6) | 0.002 |
| Fever | 6 (13.1) | 69 (4.7) | 0.011 | 4 (16.7) | 71 (4.8) | 0.008 | 23 (2.3) | 52 (10.1) | <0.001 |
| Shortness of breath | 5 (10.9) | 114 (7.8) | 0.419 | 2 (8.3) | 117 (7.9) | 0.937 | 83 (8.4) | 36 (7.0) | 0.353 |
| Pain | 3 (6.5) | 22 (1.5) | 0.009 | 0 (0.0) | 25 (1.7) | 0.521 | 9 (0.9) | 16 (3.1) | 0.001 |
| Malaise | 13 (28.3) | 9 (0.6) | <0.001 | 13 (54.2) | 9 (0.6) | <0.001 | 10 (1.0) | 12 (2.3) | 0.042 |
| Loss of smell and taste | 3 (6.5) | 10 (0.7) | <0.001 | 1 (4.2) | 12 (0.8) | 0.078 | 7 (0.7) | 6 (1.2) | 0.358 |
| Diarrhea | 1 (2.2) | 10 (0.7) | 0.243 | 1 (4.2) | 10 (0.7) | 0.046 | 3 (0.3) | 8 (1.6) | 0.007 |
| Nausea | 1 (2.2) | 10 (0.7) | 0.243 | 1 (4.2) | 10 (0.7) | 0.046 | 6 (0.6) | 5 (0.9) | 0.427 |
| Vomiting | 0 (0.0) | 8 (0.6) | 0.615 | 0 (0.0) | 8 (0.5) | 0.718 | 6 (0.6) | 2 (0.4) | 0.585 |
| Expectorationa | 0 (0.0) | 2 (0.1) | 0.802 | 0 (0.0) | 2 (0.1) | 0.857 | 1 (0.1) | 1 (0.2) | 0.636 |
Chi-Square test.
The length of intensive care unit stay was longer among Covid-19 patients with a positive PCR test who presented with fever, pain, malaise, and the loss of smell and taste (p=0.011, p=0.009, p<0.001, and p<0.001, respectively) (Table 3).
Among Covid-19 patients with a positive PCR test, the mortality rate was significantly higher in those with fever and malaise as the presenting symptoms (p=0.008 and p<0.001, respectively). The relationship between the prognostic factors and initial symptoms is presented in Table 3.
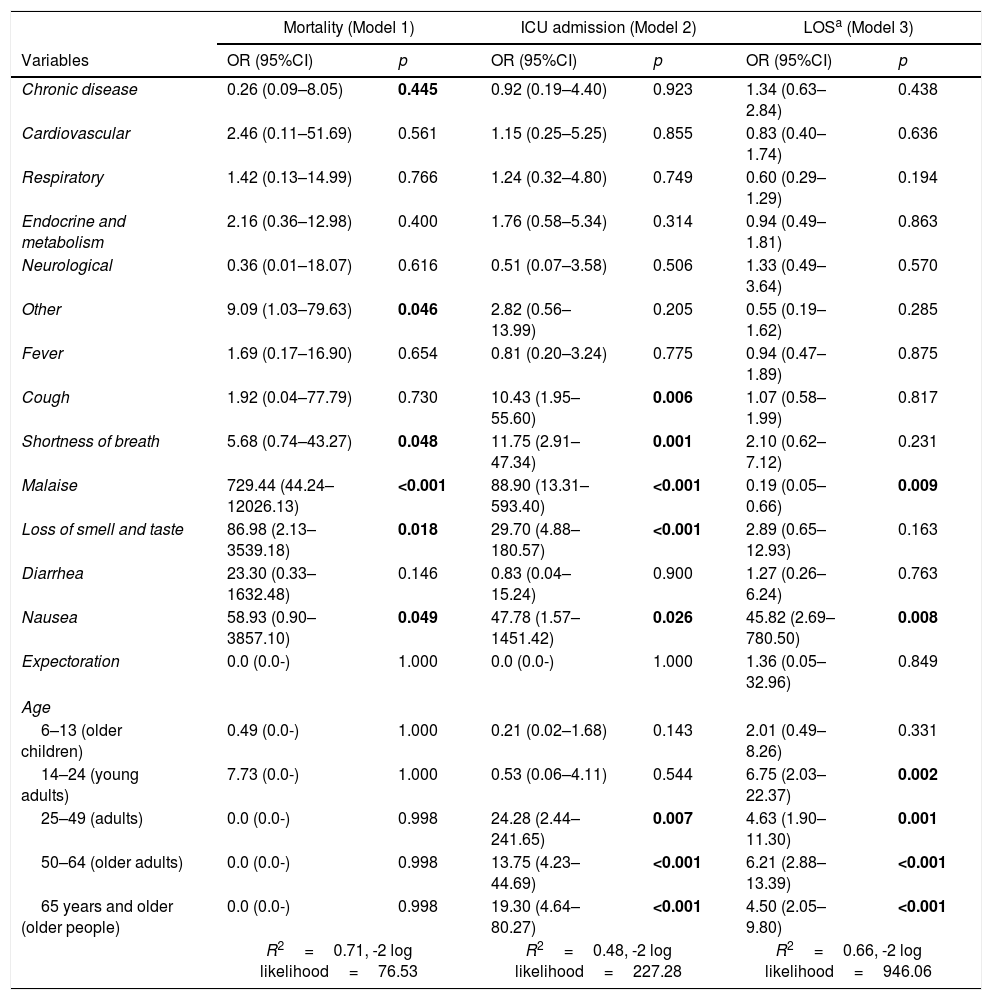
When the relationship between prognostic factors (the length of hospital stay, admission to intensive care unit, mortality) and age, the presence of chronic disease and initial symptoms was evaluated in Covid-19 patients with a positive PCR test using logistic regression analysis, the presence of a chronic disease (OR=0.26, p=0.045) the shortness of breath (OR=5.68, p=0.048), malaise (OR=729.44, p<0.001), the loss of smell and taste (OR=86.98, p=0.018), and vomiting (OR=58.93, p=0.049) were found to be associated with an increased mortality rate (Table 4/Model 1).
Age, presence of a chronic disease, initial presenting symptoms, and prognostic factors (mortality, admission to intensive care unit, length of hospital stay) in Covid-19 patients with a positive PCR test.
| Mortality (Model 1) | ICU admission (Model 2) | LOSa (Model 3) | ||||
|---|---|---|---|---|---|---|
| Variables | OR (95%CI) | p | OR (95%CI) | p | OR (95%CI) | p |
| Chronic disease | 0.26 (0.09–8.05) | 0.445 | 0.92 (0.19–4.40) | 0.923 | 1.34 (0.63–2.84) | 0.438 |
| Cardiovascular | 2.46 (0.11–51.69) | 0.561 | 1.15 (0.25–5.25) | 0.855 | 0.83 (0.40–1.74) | 0.636 |
| Respiratory | 1.42 (0.13–14.99) | 0.766 | 1.24 (0.32–4.80) | 0.749 | 0.60 (0.29–1.29) | 0.194 |
| Endocrine and metabolism | 2.16 (0.36–12.98) | 0.400 | 1.76 (0.58–5.34) | 0.314 | 0.94 (0.49–1.81) | 0.863 |
| Neurological | 0.36 (0.01–18.07) | 0.616 | 0.51 (0.07–3.58) | 0.506 | 1.33 (0.49–3.64) | 0.570 |
| Other | 9.09 (1.03–79.63) | 0.046 | 2.82 (0.56–13.99) | 0.205 | 0.55 (0.19–1.62) | 0.285 |
| Fever | 1.69 (0.17–16.90) | 0.654 | 0.81 (0.20–3.24) | 0.775 | 0.94 (0.47–1.89) | 0.875 |
| Cough | 1.92 (0.04–77.79) | 0.730 | 10.43 (1.95–55.60) | 0.006 | 1.07 (0.58–1.99) | 0.817 |
| Shortness of breath | 5.68 (0.74–43.27) | 0.048 | 11.75 (2.91–47.34) | 0.001 | 2.10 (0.62–7.12) | 0.231 |
| Malaise | 729.44 (44.24–12026.13) | <0.001 | 88.90 (13.31–593.40) | <0.001 | 0.19 (0.05–0.66) | 0.009 |
| Loss of smell and taste | 86.98 (2.13–3539.18) | 0.018 | 29.70 (4.88–180.57) | <0.001 | 2.89 (0.65–12.93) | 0.163 |
| Diarrhea | 23.30 (0.33–1632.48) | 0.146 | 0.83 (0.04–15.24) | 0.900 | 1.27 (0.26–6.24) | 0.763 |
| Nausea | 58.93 (0.90–3857.10) | 0.049 | 47.78 (1.57–1451.42) | 0.026 | 45.82 (2.69–780.50) | 0.008 |
| Expectoration | 0.0 (0.0-) | 1.000 | 0.0 (0.0-) | 1.000 | 1.36 (0.05–32.96) | 0.849 |
| Age | ||||||
| 6–13 (older children) | 0.49 (0.0-) | 1.000 | 0.21 (0.02–1.68) | 0.143 | 2.01 (0.49–8.26) | 0.331 |
| 14–24 (young adults) | 7.73 (0.0-) | 1.000 | 0.53 (0.06–4.11) | 0.544 | 6.75 (2.03–22.37) | 0.002 |
| 25–49 (adults) | 0.0 (0.0-) | 0.998 | 24.28 (2.44–241.65) | 0.007 | 4.63 (1.90–11.30) | 0.001 |
| 50–64 (older adults) | 0.0 (0.0-) | 0.998 | 13.75 (4.23–44.69) | <0.001 | 6.21 (2.88–13.39) | <0.001 |
| 65 years and older (older people) | 0.0 (0.0-) | 0.998 | 19.30 (4.64–80.27) | <0.001 | 4.50 (2.05–9.80) | <0.001 |
| R2=0.71, -2 log likelihood=76.53 | R2=0.48, -2 log likelihood=227.28 | R2=0.66, -2 log likelihood=946.06 | ||||
Advanced age (OR=19.30, p<0.001) and the presence of cough (OR=10.43, p=0.001), malaise (OR=88.90, p<0.001), the loss of smell and taste (OR=29.70, p<0.001), and vomiting (OR=47.78, p=0.026) as the initial symptoms were found to have increased the likelihood of being admitted to the intensive care unit (Table 4/Model 2).
Advanced age (OR=4.5, p<0.001), malaise (OR=0.19, p=0.009), and vomiting (OR=45.82, p=0.008) were associated with a length of hospital stay of longer than 14 days (Table 4/Model 3).
DiscussionIn the present study, approximately nine out of ten Covid-19 patients with a positive PCR test were symptomatic upon admission to the hospital, and cough was the most common presenting symptoms.
The study found that advanced age, presence of a chronic disease, shortness of breath, malaise, loss of smell and taste, and nausea upon initial admission were associated with an increased mortality rate. At the same time, admission to the intensive care unit was associated with advanced age and the presence of cough, the shortness of breath, malaise, the loss of smell and taste, and nausea on initial admission. Advanced age and the presence of malaise and nausea on admission were associated with a length of hospital stay of longer than 14 days.
The hospitals in the provinces and towns and the Family Health Centers (FHCs) located in the districts have taken important tasks in fighting against the coronavirus pandemic in Turkey. The diagnostic tests were not performed in the FHCs. As per the Public Health Guidelines of the Scientific Committee, the family physicians referred patients, suspected of having coronavirus infection for diagnostic tests to be performed in the test centers. PCR testing for Covid-19 is performed in the hospitals located in the towns and provinces in Turkey. The reason for avoiding Covid-19 testing in the FHCs is that healthy individuals often present to the FHCs for routine follow-up visits, and by avoiding Covid-19 testing in these facilities intends to minimize the disease spread among these healthy individuals and to maintain preventive healthcare services safely.5
The initial symptoms of coronavirus infection are heterogeneous. In a study of 138 patients admitted to the Covid-19 pneumonia in Wuhan city, the most common clinical symptoms were fever (99%), malaise (70%), non-productive cough (59%).6 Different from the literature data, the most common presenting symptom was cough and not fever. Uncommon occurrence of an alarming symptom as fever may complicate the diagnosis of Covid-19. In a study of 1.099 patients from Wuhan city and other districts in China, the rate of fever (axillary body temperature above 37.5°C) was 44% on initial admission and 89% among the hospitalized patients.7 In the present study, the rate of respiratory symptoms increased with age, and fever was the most common presenting symptom in the 0–6 age group. The rate of chronic diseases increases with age, and the authors consider this change presenting symptoms in Covid-19 patients. The relation of age with fever in the 0–6 age group and with cough in adults should not be overlooked. The reason for the low frequency of fever as the initial symptom in the older people can be explained by the easy access of these patients to paracetamol-containing medications, reserve paracetamol pills are found at most homes, and that these patients have made a habit of taking paracetamol pills without seeing a doctor when they have a fever.
In a Spanish study, respiratory symptoms such as cough and shortness of breath were less common in Covid-19 patients older than 65 years than in young adults.8 In a study by Machhi et al., cough was identified as the most common symptom in the first 14 days in the patients with a mild disease course.9 Cough being the most common presenting symptom and its more frequent occurrence in young adults are thought to be an important factor in rapid disease spread in the study area. Thus, the presence of this symptom on initial presentation should suggest Covid-19. Cough is an essential symptom in air-borne infections because bodily fluids spilled by cough are important in the transfer and spread of an infection.
In a study in China, malaise was reported to be one of the most common symptoms of Covid-19, and the rate of malaise was 37% in the patients with a mild disease and 39% in the patients with a severe disease course.10 Malaise, as a disease symptom, was often observed as from the disease onset and has been the most intractable symptom depending on the clinical course of the disease.11 In the present study, the frequency of malaise, as the initial presenting symptom, was lower than those reported in the literature; however, it was more common in the patients older than 65 years. This finding suggests that the presence of this non-specific symptom that can accompany many disease conditions should raise the suspicion of Covid-19 in the patients older than 65 years.
In the first cohort studies conducted in China, the loss of smell and taste (anosmia and dysgeusia) was reported as common symptoms in Covid-19 patients.12 In a study of 59 patients in Italy, 34% of the patients had loss of smell or taste, and 19% had loss of both sensations.10 They suggested that loss of smell could be an independent risk factor and used it as a marker for detecting the patients with a mild disease presentation.13 It is unclear whether this symptom could be a distinctive feature of Covid-19. It is, however, considered that this symptom occurs in the coming days in the disease course. There is also no evidence as to whether it leaves permanent damage.14 In the present study, the loss of smell and taste was rare as the initial presenting symptom. Although it is considered a distinctive feature, this symptom's rare occurrence on initial presentation poses another diagnostic challenge.
One study reported that only 16% of Covid-19 patients present with gastrointestinal symptoms, including anorexia, nausea, vomiting, diarrhea, and abdominal pain.15 Gastrointestinal symptoms such as nausea, vomiting, and diarrhea were found to be more common in Covid-19 patients in a study conducted in Turkey.16 It remains unknown whether coronavirus is transmitted through the fecal-oral route; however, fecal-oral transmission was reported during the SARS outbreak.17 Gastrointestinal symptoms in the present study were diarrhea, nausea, and vomiting. Although the rate of these symptoms as the initial presenting symptoms was lower than that reported in the literature, they were more common in the 0–14 age group. The presence of gastrointestinal symptoms in pediatric patients should raise the flag for possible diagnosis of Covid-19.
In a study examining disease prognosis, 13.8% of the patients required hospitalization, and of these patients, 6.7% required admission to the intensive care unit.18 Covid-19 has a more severe course in older people and those with a chronic disease.19 A modeling study related to the disease prognosis based on the data of Covid-19 patients in China reported that the rate of hospitalization increased with age, and a hospitalization rate of 1% was reported in the 20–29 age group, a rate of 4% was reported in the 50–59 age group, and a rate of 18% was reported in the patients aged older than 80 years. Advanced age was found to be associated with an increased mortality rate.20
It becomes apparent in recent studies that the presence of an accompanying chronic disease, apart from advanced age, is another factor affecting prognosis. In a study involving 1.139 Covid-19 patients, the disease was found to be more common and had a high mortality rate in the patients with cardiovascular disease, hypertension, chronic obstructive pulmonary, and diabetes.21 In a study examining 355 patients who died of Covid-19 in Italy, only three patients did not have an underlying comorbid condition.22 In the present study, one of every three patients had an accompanying chronic disease. Similar to that in the literature, the presence of a chronic disease is one of the factors affecting prognosis in the present study. Thus, older patients presenting to the healthcare facilities during the pandemic must be questioned for the presence of a chronic disease and referred to test centers without any further delay in case of high suspicion index for Covid-19.
The studies examining the relationship between disease symptoms, the patient complaints, and disease prognosis reported that the presence of fever and the shortness of breath increases the rate of admission to the intensive care unit. A meta-analysis study found that cough, nausea, headache, sore throat, expectoration, diarrhea, myalgia, and fatigue are not associated with the admission to the intensive care unit and prognosis.23 A Turkish study found a low rate of admission to the intensive care unit and a low mortality rate in Covid-19 patients with COPD and asthma if there is a cough. The reason for this finding was suggested to be high pneumococcal vaccination rates among patients with chronic pulmonary disease aged 65 years and older in Turkey.24
In a study by Mao et al. in China, central nervous system manifestations were reported in 36.4% of Covid-19 patients, and the loss of smell was reported in approximately 5% of the patients. These neurological symptoms were associated with a severe disease course.25 In a Turkish study, the patients with the loss of smell and taste were reported to have a low hospitalization rate. A possible explanation for this finding is the occurrence of these symptoms in the early disease stage.26 In the present study, the loss of smell and taste uncommon as an initial presenting symptom although this symptom was one of the factors affecting mortality. Therefore, the authors of the present study consider that spotting these symptoms may not ease disease diagnosis, but their presence should be taken as an alarming sign for poor prognosis.
ConclusionIn conclusion, running diagnostic tests in every individual is the most crucial tool in combating coronavirus infection, for which there is no known definitive therapy and preventive vaccine despite its widespread occurrence. The authors advise physicians working in healthcare facilities without testing facilities should place more attention on the initial presenting complaints of cough, fever, malaise, and nausea in the patients suspected of having coronavirus infection if they are to be referred to advanced healthcare facilities. It is essential to consider that these symptoms are associated with poor prognosis and deserve an approach accordingly. The authors recommend evaluating cough together with other possible factors, and the isolation of the patients without a further delay in case of a high index of suspicion for Covid-19, and the administration of antitussive therapy to relieve cough. Reducing the additional contribution of cough to the contagiousness of infection may be necessary.
Fever in children, unlike in adults, is associated with disease prognosis, and the authors suggest that Covid-19 should be added to the algorithmic approach to the children with fever.
It is essential to know that loss of smell and taste, a distinctive clinical finding for Covid-19, is among uncommon presenting symptoms, but this symptom affects prognosis. Therefore, the authors suggest that the possibility of Covid-19 should not be ruled out, and further evaluation should be made even if this symptom is absent on initial admission.
Keeping in mind that age above 65 years, the presence of a comorbid chronic condition, malaise, and nausea as the presenting symptoms could be a marker of poor prognosis in the patients with a high index of suspicion for Covid-19, the patients presenting to the primary healthcare facilities with these features must be referred to an advanced healthcare facility without further delay.
- •
Fever measurement is performed while entering common areas all over the world for the purpose of screening Covid-19.
- •
A common algorithm could not be created to suspect Covid-19 in health centers where PCR testing cannot be performed.
- •
Although the symptoms seen in Covid-19 have been shown in many studies, there are not enough studies showing what the initial symptoms are and the relationship of these symptoms with prognosis.
- •
This study shows that for covid-19 screening, the complaint of cough should be considered as the first application complaint rather than fever control in common areas.
- •
In health centers where Covid-19 PCR testing cannot be performed, Covid 19 provides information to an algorithm to be created from initial symptoms.
- •
This study particularly reveals the frequency of initial symptoms of Covid 19, as well as their relationship with prognosis.
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Conflict of interestAuthors do not have any conflict of interest to declare.
No funding.