The implementation of a standardized language in Nursing Care Plans (SNCP) allows for increased efficiency in nursing data management, and from our experience, its short-term effectiveness in patients with type 2 diabetes mellitus (T2DM) has been established.1 Nevertheless, up-to-date data on the relationship between SNCP and patients’ long-term health outcomes remain unclear. The aim of this study was to evaluate the effectiveness of implementing SNCP with NANDA-International (NANDA-I) nursing diagnoses2 and interventions (NIC3) in the Computerized Clinical Records registration, in the improvement of metabolic, weight, and blood pressure control in patients with T2DM after 4-year follow-up.
This study was conducted as part of a broader project with its methodology being described elsewhere;1 consisting in a 4-year prospective follow-up study carried out between March 2008 and February 2012. For the purposes of this paper we analyze only to the baseline and after 4-year of follow-up data. 30 primary health care centers (Madrid, Spain) consented to participate (23,488 T2DM outpatients), and data were collected from Computerized Clinical Records under routine clinical practice conditions.
18,320 patients were identified in the Usual Nursing Care Plans (UNCP) group, and 5168 in the SNCP group. However, the number of patients in the SNCP group with at least one HbA1c over the 4-year of follow-up was 2105, and for this reason we decided to select a random sample of an equal size in the UNCP group. Ensuring that patients in both groups were more likely to have collected all the necessary variables for them.
The study was approved by the research ethics committee of the Ramón y Cajal Hospital (Madrid), and it was determined that no informed consent was necessary in this type of study.
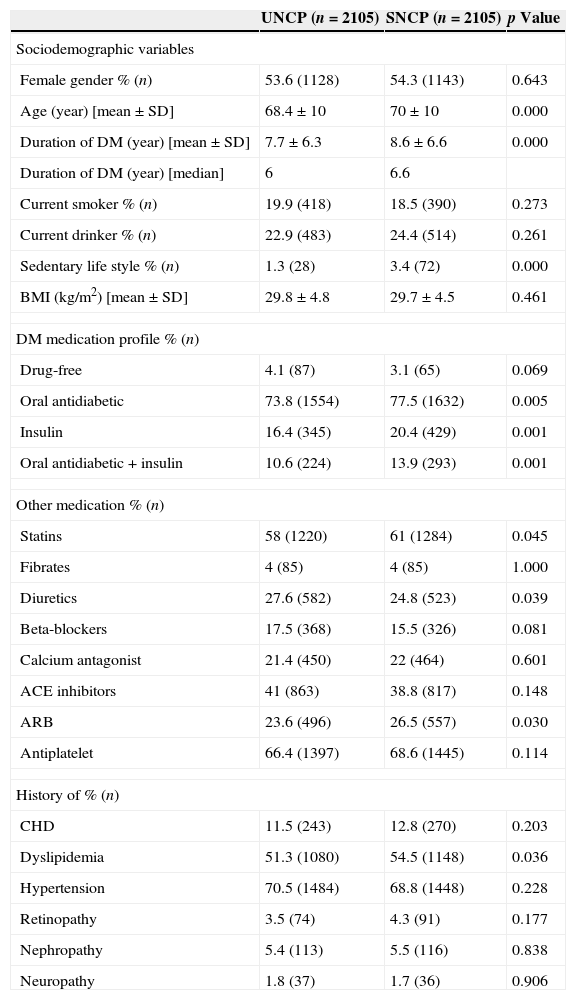
The two groups were homogeneous in gender, but not in age, diabetes evolution time and sedentary life style (Table 1, first part). Patients in the SNCP group had a higher prevalence of dyslipidemia; received more treatment for diabetes (oral antidiabetics and insulin) and for cardiovascular disease, had poorer HbA1c (7.13% vs. 7.01%; p<0.001), and better Diastolic Blood Pressure (DBP) (75.9mmHg vs. 76.5mmHg; p<0.01), and LDL-Cholesterol (114.05mg/dl vs. 116.5mg/dl; p<0.01) than patients in the UNCP group.
Basal characteristics of participants (first part: upper side section) and mean values (SD) and changes of basal and final parameters in both groups (second part: lower side section).
| UNCP (n=2105) | SNCP (n=2105) | p Value | |
|---|---|---|---|
| Sociodemographic variables | |||
| Female gender % (n) | 53.6 (1128) | 54.3 (1143) | 0.643 |
| Age (year) [mean±SD] | 68.4±10 | 70±10 | 0.000 |
| Duration of DM (year) [mean±SD] | 7.7±6.3 | 8.6±6.6 | 0.000 |
| Duration of DM (year) [median] | 6 | 6.6 | |
| Current smoker % (n) | 19.9 (418) | 18.5 (390) | 0.273 |
| Current drinker % (n) | 22.9 (483) | 24.4 (514) | 0.261 |
| Sedentary life style % (n) | 1.3 (28) | 3.4 (72) | 0.000 |
| BMI (kg/m2) [mean±SD] | 29.8±4.8 | 29.7±4.5 | 0.461 |
| DM medication profile % (n) | |||
| Drug-free | 4.1 (87) | 3.1 (65) | 0.069 |
| Oral antidiabetic | 73.8 (1554) | 77.5 (1632) | 0.005 |
| Insulin | 16.4 (345) | 20.4 (429) | 0.001 |
| Oral antidiabetic+insulin | 10.6 (224) | 13.9 (293) | 0.001 |
| Other medication % (n) | |||
| Statins | 58 (1220) | 61 (1284) | 0.045 |
| Fibrates | 4 (85) | 4 (85) | 1.000 |
| Diuretics | 27.6 (582) | 24.8 (523) | 0.039 |
| Beta-blockers | 17.5 (368) | 15.5 (326) | 0.081 |
| Calcium antagonist | 21.4 (450) | 22 (464) | 0.601 |
| ACE inhibitors | 41 (863) | 38.8 (817) | 0.148 |
| ARB | 23.6 (496) | 26.5 (557) | 0.030 |
| Antiplatelet | 66.4 (1397) | 68.6 (1445) | 0.114 |
| History of % (n) | |||
| CHD | 11.5 (243) | 12.8 (270) | 0.203 |
| Dyslipidemia | 51.3 (1080) | 54.5 (1148) | 0.036 |
| Hypertension | 70.5 (1484) | 68.8 (1448) | 0.228 |
| Retinopathy | 3.5 (74) | 4.3 (91) | 0.177 |
| Nephropathy | 5.4 (113) | 5.5 (116) | 0.838 |
| Neuropathy | 1.8 (37) | 1.7 (36) | 0.906 |
| UNCP | SNCP | Unadjusted SNCP effect (95%CI)* | Adjusted SNCP effect (95%CI)** | |
|---|---|---|---|---|
| Hba1c (%) mean (SD) | ||||
| N patients | 2,105 | 2,105 | ||
| Basal | 7.01 (1.09) | 7.13 (1.05) | ||
| 2 years | 6.96 (1.03) | 7.02 (0.98) | ||
| 4 years | 6.96 (1.01) | 7.06 (1.05) | ||
| Change | −0.059 (0.99) | −0.067 (1.0) | −0.008 (−0.068 to 0.052) | −0.06 (−0.54 to 0.41) |
| p Value | 0.007 | 0.002 | 0.789 | 0.792 |
| LDL cholesterol (mg/dl) mean (SD) | ||||
| N patients | 1,931 | 1,968 | ||
| Basal | 116.5 (29.8) | 114.05 (28.3) | ||
| 2 years | 105.5 (27.04) | 103.1 (26.08) | ||
| 4 years | 102.0 (27.3) | 101.2 (26.5) | ||
| Change | −14.7 (29.9) | −12.7 (29.5) | 2.03 (−0.83 to 3.97) | −6.24 (−19.7 to 7.21) |
| p Value | <0.001 | <0.001 | 0.041 | 0.358 |
| SBP (mmHg) mean (SD) | ||||
| N patients | 2,064 | 2,087 | ||
| Basal | 134.1 (12.6) | 133.9 (12.05) | ||
| 2 years | 132.07 (11.4) | 132.18 (11.2) | ||
| 4 years | 132.4 (12.1) | 131.7 (11.7) | ||
| Change | −1.85 (12.3) | −2.23 (11.7) | −0.376 (−1.14 to 0.39) | −4.59 (−10.1 to 0.91) |
| p Value | <0.001 | <0.001 | 0.337 | 0.101 |
| DBP (mmHg) mean (SD) | ||||
| N patients | 2,064 | 2,087 | ||
| Basal | 76.5 (7.3) | 75.9 (6.9) | ||
| 2 years | 74.8 (7.2) | 74.2 (6.6) | ||
| 4 years | 74.6 (7.3) | 73.7 (6.7) | ||
| Change | −1.86 (7.4) | −2.14 (6.9) | −0.279 (−0.74 to 1.82) | −3.60 (−6.18 to −1.03) |
| p Value | <0.001 | <0.001 | 0.235 | 0.007 |
| BMI (kg/m2) mean (SD) | ||||
| N patients | 1,650 | 1,860 | ||
| Basal | 29.8 (4.8) | 29.7 (4.5) | ||
| 2 years | 29.7 (4.9) | 29.5 (4.6) | ||
| 4 years | 29.7 (5.1) | 29.5 (4.7) | ||
| Change | −0.33 (2.2) | −0.32 (2.04) | 0.006 (−0.15 to 0.16) | 0.28 (−0.73 to 1.29) |
| p Value | <0.001 | <0.001 | 0.939 | 0.579 |
UNCP: Usual Nursing Care Plans; SNCP: Standardized Nursing Care Plans; HbA1c: Glycated hemoglobin; LDL cholesterol: low-density lipoprotein-Cholesterol; SBP: Systolic Blood Pressure; DBP: Diastolic Blood Pressure; BMI: Body Mass Index.
The variable Change (mean at the 4-year follow-up value minus mean baseline value) was calculated in both groups for the following variables: HbA1c, LDL cholesterol, SBP, DBP, and BMI.
At the 4-year follow-up, both groups experienced a modest decline in their parameter values (Table 1, second part). The unadjusted effect of SNCP improved health outcomes, except for LDL cholesterol and BMI. After adjusting for baseline parameter values and age, duration of T2DM, type of treatment, physical inactivity and dyslipidemia, a lowering effect on all health outcomes was observed, except for BMI. DBP showed a significant and relevant reduction (decrease of 3.60mmHg); however, Systolic Blood Pressure (SBP) showed a relevant but not significant reduction (decrease of 4.59mmHg). Finally, those in the SNCP group saw a relative risk reduction of 32.3% (95%CI=0.4–64.1%) and a absolute risk reduction of 1% (2% vs. 2.9%; p=0.047) for stroke; however, increased incidence of Myocardial Infarction was seen, but not significant (1.3% vs. 1%; p=0.39).
Therefore, after 4-year follow-up, patients in the SNCP group reached a persistent and significant reduction in DBP, but not significant in SBP, compared to patients in the UNCP group. Moreover, SNCP appears to be helpful in reducing the incidence of stroke. As reported in the VALUE study,4 reductions in SBP of between 2 and 4mmHg, during follow-up (4.2 years), had a very significant impact on the prevention of stroke in hypertensive patients at high risk, with patients with T2DM falling into this risk category. Finally, the strict blood pressure control observed in the UKPDS 38 study5 was associated with better stroke risk reduction compared to the finding in study; however, patients in the UKPDS 38 were not followed under routine clinical practice conditions and the duration of treatment was over 8-years.
Conflict of interestThere are no conflicts of interest to declare.
This article has been supported by the Fondo de Investigación Sanitaria, Instituto de Salud Carlos III (PI07/0865) and we thank the Madrid Nurse Diagnosis Study Group, who collaborated in the study: Carmen De Burgos-Lunar, Juan Carlos Abánades-Herranz, Rosa Arnal-Selfa, Luis Sánchez-Perruca, José Mª Mena-Mateo, Asunción Cañada-Dorado, Inmaculada García-Ferradal, María del Carmen Mustieles-Moreno, and Flora Espejo-Matorrales.