Editado por: Dr. Josep Vidal Alaball General Generalitat de Catalunya Spain
Más datosTo analyze the opinions of nursing professionals on the current limitations and future potential of digital tools in healthcare.
DesignQualitative and descriptive study.
LocationThe study took place during an asynchronous MOODLE course on the use of ICT in healthcare, specifically aimed at nursing professionals.
ParticipantsThe number of nurses enrolled in the course was 150.
MethodsA qualitative study was conducted focusing on the positive and negative aspects that telenursing can offer in the context of a Moodle training in new technologies for nurses. A thematic analysis was carried out following the method proposed by Braun and Clarke.
ResultsIn the end 68 nurses participated in the forum. Their statements, opinions and perceptions were analyzed and 28 descriptive codes were obtained and subsequently categorized into positive and negative aspects.
ConclusionsNurses positively value the usefulness of digital tools and identify a wide range of benefits of telenursing in daily practice. At the same time, they point out crucial limitations that may slow down the adoption of telenursing, pointing to areas for improvement such as training and digital literacy of both patients and professionals. They consider that telenursing can humanise care, but insist on the need to prevent its use from increasing health inequalities.
Analizar las opiniones de los profesionales de enfermería sobre las limitaciones actuales y el potencial futuro de las herramientas digitales en la atención sanitaria.
DiseñoEstudio cualitativo y descriptivo.
LugarEl estudio se desarrolló durante un curso MOODLE asíncrono sobre el uso de las TIC en la atención sanitaria, dirigido específicamente a profesionales de enfermería.
ParticipantesEl número de enfermeras inscritas en el curso fue de 150.
MétodosSe realizó un estudio cualitativo centrado en los aspectos positivos y negativos que puede ofrecer la teleenfermería en el contexto de una formación Moodle en nuevas tecnologías para enfermeras. Se realizó un análisis temático siguiendo el método propuesto por Braun y Clarke.
ResultadosFinalmente participaron en el foro 68 enfermeras. Se analizaron las declaraciones, las opiniones y las percepciones de las mismas, obteniéndose 28 códigos descriptivos que posteriormente se categorizaron en aspectos positivos y negativos.
ConclusionesLas enfermeras valoran positivamente la utilidad de las herramientas digitales e identifican una amplia gama de beneficios de la teleenfermería en la práctica diaria. Al mismo tiempo, señalan limitaciones cruciales que pueden ralentizar la adopción de la teleenfermería, señalando áreas de mejora como la formación y la alfabetización digital tanto de pacientes como de profesionales. Consideran que la teleenfermería puede humanizar la asistencia, pero insisten en la necesidad de evitar que su uso aumente las desigualdades en salud.
Advances in electronic technology, information technology and communications at the end of the 20th century have provided an ideal scenario for the development of ICT (Information and Communication Technologies) applied to health, especially for remote management and exchange of information, knowledge and practices related to the provision of health and healthcare.1 Industrialized countries and developing countries have experienced growing interest in this field and are producing processes of reform and modernization of the health sector that aim at greater equity in the provision of services, effectiveness and utility based on the use of ICT.2
Telemedicine, according to the World Health Organization (WHO), is defined as the provision of remote health services carried out by health professionals using ICT. Telenursing could be defined as the use of telecommunications technology in the nursing discipline to improve patient care, among other applications. Telenursing is within the global concept of telemedicine and the term is accepted and used to visualize the role of the nurse in the use of ICT.3 There are various forms of telenursing although the best known is the one that involves both the patient and the nurse being connected in real time via a mobile device or computer, although the telephone could also be used. This form of telenursing is called synchronous (or live) tele-nursing. Other modalities could be asynchronous telenursing where the patient and the nurse do not communicate in real time but communicate via e-mail or similar. Another modality would involve monitoring health parameters remotely, which would then be received by the nurse for analysis, helping to make decisions about future care. However, all these modalities are complementary and can occur with the same patient, depending on the needs of the moment.4
The International Council of Nurses (ICN) considers telenursing as a service that allows nurses to provide care to rural or remote populations, maintaining effective communication with patients, where they intervene to effectively promote and disseminate healthy lifestyle, self-care and other topics of importance to people's health care.5
In the same line, but this year 2023, the ICN states that the nursing profession must contribute to and keep pace with this [digital] transformation to ensure digital health technology is developed and applied in a way that meets the needs of individuals, families, communities and the health workforce.6
Current evidence shows that telemedicine and telenursing have developed during the COVID-19 pandemic and the 2020 confinement,7–10 but the extent to which these changes are longstanding is still unknown.11,12 However, numerous benefits of the use of telemedicine and tele-nursing in patient communication and follow-up13 have been documented. And even at other levels such as environmental impact,14 cost reduction and system efficiency.15
In this paper, we present a qualitative study that aims to analyze the opinions of nurse professionals about the current limitations and future potential of digital tools in healthcare. Professionals were enrolled in a training programme about new technologies in healthcare, in which thematic discussions through an electronic forum were held.
MethodsThis study used qualitative-descriptive design. This type of studies provides detailed description of bias aspects of events or experiences from a subjective perspective.16 Besides, qualitative-descriptive design allows for capturing the richness and complexity of the phenomenon under study17 and it builds a comprehensive and detailed account of a phenomenon without extensive interpretation or theorization.18,19
In order to ensure rigour and quality, the interpretative paradigm approach of Guba and Lincoln has been followed in this research.20
The study was developed alongside a self-paced asynchronous MOODLE course training on telenursing, specifically aimed at nurse professionals. The course contained six units (Introduction to telenursing, Definitions, Usability, Clinical Security, Confidentiality and Privacy, and Applications and Recommendations) and lasted 40 days, from September to October 2023. On each unit, the course instructors proposed questions and debates to the learners. Participants’ comments on the benefits of using telehealth in Primary Care as well as their negative aspects or areas for improvement. Non-probabilistic convenient sampling was used for the selection of participants based on their accessibility, participation in the discussion forums and availability during the study period. The only exclusion criterion was not participating into the proposed discussions.
In this research, a thematic analysis of the textual content of the forum was carried out. In this sense, the research team entered the data into a database for subsequent thematic analysis, following the method proposed by Braun and Clarke.21 According to the method proposed by these authors, the process of analysis in this study focused on the elaboration of mutually exclusive and collectively exhaustive categories. In this way, these categories were intended to reflect the phenomenon under study and not another topic. For a correct triangulation of the data,22 a review of the textual elements obtained and their categorisation by one researcher was carried out, followed by a review by a second researcher. In this way, we broadened, deepened, and reduced the possibility of misunderstanding, thus clarifying the meaning and veracity of the information obtained in the testimonies. This triangulation was also achieved by obtaining the different perspectives of the members of the research team, which included a nurse and two telecommunications engineers. Finally, the resulting report was discussed as a team and, through reflective thinking and critical reasoning, changes were made until a consensus was reached. This project has been approved by the Ethics Committee of the Catholic University of Valencia with the code UCV/2022-2023/001 and informed consent was obtained from all participants.
ResultsThe number of students enrolled in the course was 150. A total of 68 participants (62 female) participated in the debate in the forum of the MOODLE platform, representing a 45% participation rate. The selection of participants was based on the criterion of contributing to the discussion forums.
Although data saturation was reached after the analysis of participant 41's comments, the research team decided to analyze all the texts obtained to ensure that no relevant themes were lost from the analysis. No new thematic categories emerged after comment 41.
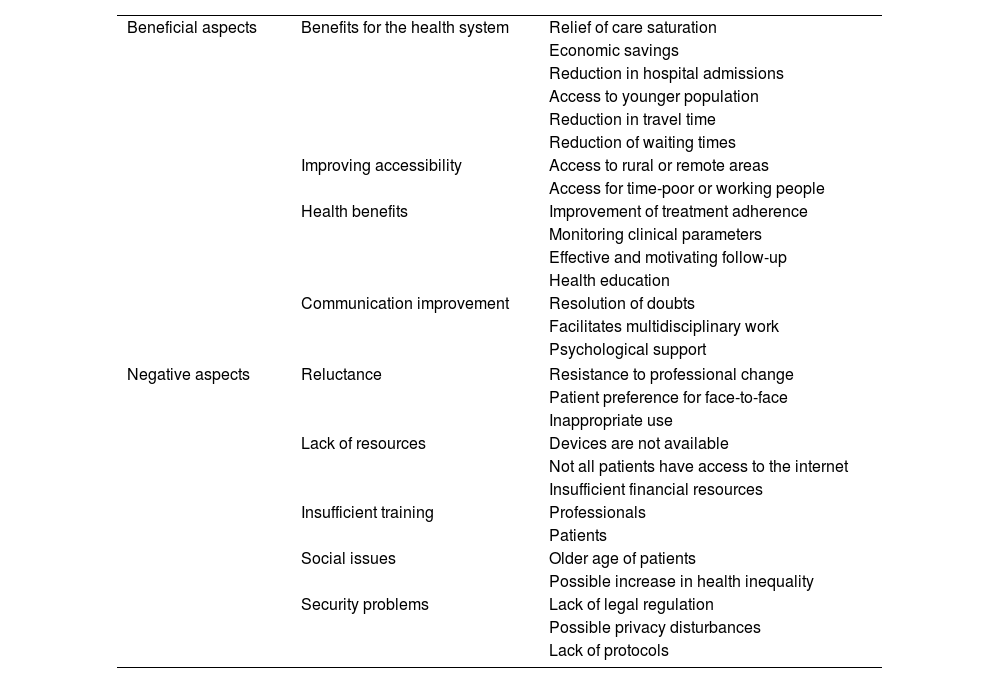
A content analysis of the collected responses performed, resulting in 28 descriptive codes (Table 1). The codes were grouped into two main themes (beneficial aspects and negative or non-beneficial aspects) and nine sub-themes (Table 1).
Themes, subthemes, and codes.
| Beneficial aspects | Benefits for the health system | Relief of care saturation |
| Economic savings | ||
| Reduction in hospital admissions | ||
| Access to younger population | ||
| Reduction in travel time | ||
| Reduction of waiting times | ||
| Improving accessibility | Access to rural or remote areas | |
| Access for time-poor or working people | ||
| Health benefits | Improvement of treatment adherence | |
| Monitoring clinical parameters | ||
| Effective and motivating follow-up | ||
| Health education | ||
| Communication improvement | Resolution of doubts | |
| Facilitates multidisciplinary work | ||
| Psychological support | ||
| Negative aspects | Reluctance | Resistance to professional change |
| Patient preference for face-to-face | ||
| Inappropriate use | ||
| Lack of resources | Devices are not available | |
| Not all patients have access to the internet | ||
| Insufficient financial resources | ||
| Insufficient training | Professionals | |
| Patients | ||
| Social issues | Older age of patients | |
| Possible increase in health inequality | ||
| Security problems | Lack of legal regulation | |
| Possible privacy disturbances | ||
| Lack of protocols | ||
Many benefits for the health system are mentioned by participants, especially those related to cost and resource savings, alleviation of the burden of care or savings in resources. Perhaps in a few years we will see more development of these ideas, although the truth is that I suppose they will be carried out mainly because of the need to alleviate an overcrowded system… (Participant 2) We could go a long way on the issue of care, waiting lists and saturation of nursing schedules. (Participant 56) It is currently a challenge, but I think it will develop more and more naturally…. And when the administration sees that it is more profitable to implement it in the long term. (Participant 33)
Participants also point to tele-nursing to bring healthy advice and information to young people. It would even be a good tool to interact with the younger community. (Participant 41)
Some participants even consider that it could have an impact on reducing hospital admissions, benefiting not only the system but also the patients themselves and their families. …support with good communication skills could reduce morbidity and mortality and avoid unnecessary transfers and hospital admissions. (Participant 52)
Many of the participating nurses value tele-nursing as a useful tool for improving patient accessibility to health services, by facilitating access for people living in rural areas. I think in busy consultations, [telenursing] is a way to reach more people or patients living in rural areas. (Participant 11) It should also be considered that in many rural areas, technology is not as integrated as in cities. However, it would be interesting to implement it especially in these places, thus reducing the waiting time and the distance to travel to receive health care. (Participant 36)
One aspect that was much commented on by the participants and which generated a lot of interest in the forum was the proposal to use tele-nursing with young people with chronic pathology who do not usually come to the centres for work reasons. [Telenursing] would be very useful for the recruitment of the working adult population (30–50 years old) with chronic illnesses who do not follow up with nurses due to lack of knowledge or difficulties in attending due to work schedules. (Participant 33) For me the problem is the one who at 40–50 years of age is diagnosed with hypertension or diabetes and considers that it is not necessary to go to the nurse because the doctor's control is enough. For this type of patients who work and consider that it is not important to come to the nurse's office, tele-nursing is important. (Participant 28)
The participating nurses believe that tele-nursing has a positive impact on health and can bring many benefits. These include improved adherence to treatment, continuous monitoring of health parameters, improved follow-up in chronic pathology, surgery, etc. It would be a good idea to include it in adult programmes and as a support to improve adherence to treatment, if they really had the right resources, I think it would be a fantastic tool. (Participant 13) For behavioural and motivational therapies, such as weight loss and balanced diet, more regular nursing follow-up in a virtual manner could be very effective. (Participant 37)
They also point to the health benefits of the open channel with patients and the public that the use of telenursing brings, helping to disseminate healthy advice and health education. I think that in Primary Care we have fixed telephones, corporate e-mails, computers, some webcams, that allow us to carry out tele-nursing for appointments, follow-ups, counselling, and health education, among other activities. (Participant 20) From my personal experience, I see a lot of applications in primary health care, as well as in counselling for parents of children, caregivers of the elderly, etc. (Participant 24)
Nurses consider tele-nursing to be useful for improving professional–patient communication, resolving doubts in an agile way, and accompanying people with emotional support needs. From primary care it would be possible to carry out many interventions with telehealth, and as a paediatric nurse I consider it a fantastic resource to help parents to solve day-to-day doubts such as those related to complementary feeding or vaccinations. (Participant 49) In my opinion, [telenursing] is undoubtedly an improvement in the nurse–patient relationship and can facilitate communication. (Participant 61)
They also consider it to be a valuable tool for more effective communication between professionals. [Telenursing] facilitates the work of the multidisciplinary team and allows information to reach areas that are more difficult to access, shortening waiting lists. (Participant 58)
Interestingly, several nurses see the use of tele-nursing to further humanize care. From my point of view, telenursing is a good option in the accompaniment of chronically or palliatively ill patients, to bring the profession closer and humanize it a little more if possible. (Participant 21)
One of the main problems reported by nurses is resistance to change, fear of the unknown or of inappropriate use, by both professionals and patients. …my feeling is that the professionals themselves find it difficult to recognize the benefits of this form of patient monitoring, control, and education, preferring face-to-face [sessions or care]. (Participant 31) Often, fear of the unknown prevents us from moving forward and learning new things (Participant 47). I believe that the difficulty of access to technologies in some sectors and the inappropriate use by some professionals are the biggest handicaps. (Participant 11)
They also consider that patients might prefer face-to-face care. The majority [of patients] prefer to come to the consultation in person. (Participant 54) Even though with the pandemic, telephone care in primary care has become somewhat more normalised in some cases, I note that the population still prefers “face-to-face” care. (Participant 45)
Participants are concerned about the lack of adequate or obsolete equipment, logistical and financial support to implement telenursing. I believe that today, we professionals do not have the necessary resources to do our work well through tele-nursing. (Participant 17) I think that currently, the biggest barrier to the use of ICTs in practice is the material resources. Specifically, those that are either outdated and delay many of the tasks that we want to carry out digitally, or because we do not have the App, the webcam, or other key elements in telenursing. (Participant 14)
In the opinion of our participants, patients are also affected by financial and logistical constraints. I believe that one of the main limitations is the lack of resources (especially financial resources), because to be able to offer this service in an equitable way, users should be able to have access to the internet, regardless of their purchasing power. (Participant 36)
Nurses are aware of the importance of being well trained to be able to apply new digital systems. They also consider it useful and necessary to train patients to be able to use telenursing. From my point of view and in agreement with my colleagues, I reiterate the lack of resources and training when it comes to carrying out quality telenursing. (Participant 12) At present, I believe that there is a lack of material means and a lack of training to be able to apply it properly. (Participant 22) I believe that this is a thriving sector that can bring multiple benefits to both patients and professionals, although it requires training and education for both patients/families and healthcare staff. (Participant 25)
Aspects such as the advanced age of health service users, as well as the fact that tele-nursing may exacerbate social inequalities, are of particular concern to nurses. …the most important handicap is that our population is mainly an ageing population that does not have the opportunity to “jump on the bandwagon” of these new technologies. (Participant 64) …in vulnerable or isolated populations such as rural villages with no coverage or people with few resources, telenursing could increase health inequalities. (Participant 38)
The participants consider that in the implementation of health technologies it is important to consider the privacy of users, legal coverage and the protocols that guide their actions as professionals. The main problem I find is that today, to carry out telecare, we must resort to various apps or programs from our own electronic devices, which puts the security and privacy of patients and ourselves at risk. (Participant 40) I think that it is a very changing reality, that we lack training, regulation, the creation of protocols for use and systems for evaluating its quality. (Participant 20)
Despite the natural barriers of training and access to resources, telenursing has the potential of transforming nursing. As this study shows, nurses are positive about its usefulness, being able to identify numerous benefits. However, they are also aware of current limitations and areas for improvement.
On the positive side, the nurses participating in this research noted that telenursing was useful for effective and motivating follow-up and improve communication with patients. These benefits have also been pointed out by other authors who indicate that telenursing is not only useful in the clinical follow-up of patients with chronic pathology but could also be effective in improving lifestyle behaviours in chronic diseases,23–25 including promoting self-efficacy and physical activity.26 Alcazar et al., points out that telenursing can be a facilitator to foster a good, closer nurse–patient relationship.27
Our participants have also indicated that this technology can be useful to reduce complications, monitor health parameters, avoid unnecessary admissions, and resolve doubts quickly. Along the same lines, other studies have concluded that telenursing helps to detect complications more quickly after surgery,28 to solve problems or questions faster,29,30 to reduce symptoms and discomfort,31 to reduce unnecessary admissions32 and even to reduce mortality.33 It is also a useful tool to educate and support young people with chronic pathology.34
As for the negative aspects or limitations pointed out by the participants, it is important to point out that these are the same ones that are often mentioned in the adoption of other technologies35 and that in many cases could be overcome with training and institutional support.36 Telenursing cannot be used with all patients and in all situations, but it may be a further role of nurses to teach the patient to use it, thus reinforcing their digital leadership. It is interesting to note that in previous studies,27 reluctance to use tele-nursing on the part of the professionals was observed. However, this is not the case with the participants in this study, who are generally enthusiastic about the idea of its future use. Nevertheless, as participants rightly pointed out, it is important to consider the barriers that patients may present. The health system needs to be sensitive to patients’ needs to avoid widening health inequalities.8,37
While this qualitative study offers valuable insights into the perspectives and experiences of nurses engaged in a MOODLE course, it is important to acknowledge some limitations that may impact the generalizability of these findings. The study was conducted with a relatively small sample of students from a specific course which may not fully capture the diversity of opinions and experiences that could exist within a broader professional group of nurses. Subjects who chose to participate in the forums may have different characteristics or experiences compared to those who declined, potentially leading to a skewed representation of opinions. Future studies will include secondary analysis about the participants (e.g., age range, urban vs. rural practice, years of experience) to better understand the contexts from which the perceptions are drawn. Finally, as with any self-reported data, there is a possibility of social desirability bias, where participants may provide responses, they perceive as socially acceptable rather than their true opinions. It is important to contextualize that the data used for the study comes from the direct participation of the 45% of the professionals enrolled in the course and the researchers had no access to the opinions and perceptions of remaining 55%, which may affect these findings.
The COVID-19 pandemic has significantly accelerated the adoption of telemedicine, transforming the way healthcare services are delivered. Several studies and reports have highlighted the impact of telemedicine on patient care delivery, patient satisfaction, and safety during the confinement period.38,39 The experiences gained during the pandemic have paved the way for a more integrated approach to healthcare, combining both in-person and virtual care to meet the diverse needs of patients. The study's outcomes could benefit from a more pronounced emphasis on articulating prospective interventions on the use of tele-nursing in specific clinical domains (e.g.: diabetes control) and the definition of new training policies. Future work should assess how these perceptions about the new ICTs contribute to improve patient care, the satisfaction of healthcare professionals and the sustainability of the national healthcare system.40
ConclusionsThe participating nurses note many positive aspects of the use of tele-nursing, especially for patients, but also for practice management. It is encouraging that they value this resource as a “humaniser” of care, to improve nurse–patient communication and to reach those we cannot reach now. Nurses need support and resources but are highly motivated to apply tele-nursing in their daily work in Primary Care.
- -
Telemedicine and tele-nursing have clear advantages such as increased accessibility to specialists, reduced travel times for patients, reduced costs of health care delivery.
- -
Telenursing could have the potential to transform the nursing discipline and nurses themselves are positive and hopeful about its use in the immediate future.
- -
It is noted that nurses believe in the use of tele-nursing as a tool to humanise healthcare.
This project has been approved by the Ethics Committee of the Catholic University of Valencia with the code UCV/2022-2023/001 and informed consent was obtained from all participants.
FundingThe authors received no financial support for the research, authorship, and/or publication of this article.
Conflict of interestThe authors of this article declare that they have no conflict of interest in relation to this research.