The COVID-19 pandemic led to a mass use of teleconsultation. The aim of this study is to understand the family doctors' perspective over the utility of teleconsultation in their future clinical practice.
MethodsA cross-sectional study was realized through the application of an online survey, between September 18th and December 4th, 2020. The target population were family medicine physicians and residents who worked in a primary health unit belonging to the portuguese National Healthcare Service. A descriptive analysis of the characteristics of the participants and of their answers to the survey was performed.
Results377 responses were received. It was identified as the main advantage the greater accessibility (68,7%), as the main disadvantage the impossibility to perform physical examination (81,2%) and as the main obstacle the lack of appropriate resources to teleconsultation (70,0%). The majority of the participants acknowledge that teleconsultation represents a valuable asset to the future of medicine (83,6%). 80,6% of the doctors would like to implement a teleconsultation period in their schedule and 76,1% think that teleconsultation will become essential to future clinical practice.
ConclusionPublished studies support our findings, regarding advantages, disadvantages and obstacles. It is acknowledged that currently neither portuguese population nor family medicine are ready for teleconsultation, although this is considered to be a useful tool to future clinical practice.
La pandemia de covid-19 impuso masivamente la teleconsulta. El objetivo es conocer la perspectiva de los médicos de familia respecto a la utilidad de la teleconsulta en la futura práctica clínica.
Materiales y métodosFue realizado un estudio transversal con la aplicación de un cuestionario online, entre 18 de septiembre y 4 de diciembre de 2020. La población diana fueron los médicos de familia y los internos con formación específica en Medicina General y Familiar que ejercen en la atención primaria de salud del Servicio Nacional de Salud portugués. Las características de los participantes y sus respuestas fueron sometidas a una análisis descriptiva.
ResultadosSe obtuvieron 377 respuestas. La principal ventaja fue una mayor accesibilidad (68.7%), la principal desventaja fue la imposibilidad de realizar el examen físico (81.2%) y el principal obstáculo fue la falta de recursos adecuados (70.0%). La mayoria de los participantes reconocen que la teleconsulta representa un beneficio en el futuro de la medicina (83,6%). 80,6% de los médicos respondieron que les gustaria integrar la teleconsulta dentro del horário. Para 76,1% de los médicos encuestados la teleconsulta se volverá esencial en la prática médica futura.
Discusión y conclusiónLos estudios publicados sobre el tema corroboran sus hallazgos, es decir, en relación con las ventajas, desventajas y obstáculos. En este estudio, se reconoce que actualmente ni la población portuguesa ni la Medicina General y Familiar están preparadas para la teleconsulta, pero se considera que esta es una herramienta útil para la práctica clínica futura.
The first cases of novel coronavirus (nCoV) were first detected in China in December 2019, with the virus spreading rapidly across the world. This led World Health Organization (WHO) to declare the outbreak as a pandemic on 11 March 2020.1
The COVID-19 pandemic has necessitated a rapid response from primary care services and has prompted practitioners to consider implementing alternative methods of remote consultation to minimize the absence of face-to-face visits.2
The first description of telephone use for clinical diagnóstico appeared in a medical journal in 1879.3 And since then, this method of consultation has been increasingly used. 4
With the onset of the pandemic, it has become obvious that:5
- 1.
A sizable proportion of outpatient visits in various settings can be clinically managed effectively from a distance. 5
- 2.
Most health care systems in private and public sectors have already deployed electronic health records, thereby ensuring continuity of care for their patients.5
- 3.
The necessary logistics can be developed promptly, including the necessary training where needed, staffing and workflow with minimal disruptions or dislocations.5
Teleconsultation is defined as a consultation performed at a distance, using information and communication technologies. The clinical record is mandatory and it allows the healthcare professional to consult and evaluate the clinical history, as well as to carry out the care plan.6
The benefits of telehealth were recognized by individuals engaging in telehealth in Saudi Arabia as enhancing the standard of treatment, improving access to healthcare, and saving both time and money. The use of the technology also enables better communication between the healthcare providers and the patients. Nevertheless, the decreasing quality of patient-doctor relationship cannot be ignored. There are also privacy issues regarding the accumulated data: comparing to face-to-face consultations, telemedicine has increased risks related to privacy and security.7
In the United Kingdom (UK) National Health Service (NHS), there has been growing interest in the use of video as a method of consultation between clinician and patient over the last 10 years, and randomized controlled trials have shown such consultations to be acceptable, safe and effective in selected patients. Video is now playing an increasingly important role in providing patients with access to healthcare, either for those with COVID-19 symptoms or with other conditions. 8
During 2020, due to the COVID-19 pandemic, the implementation of teleconsultation in the daily clinical practice of portuguese Family Doctors became a reality. Therefore, it is essential to reflect on the advantages and disadvantages of this type of consultation and its role in the future of clinical practice.
Thus, the main goal of this work is to present the perspective of portuguese Family Doctors on teleconsultation as a tool in their future clinical practice. Hence, we intend to survey possible obstacles, advantages, disadvantages and in what circumstances the use of teleconsultation could be an asset in the future.
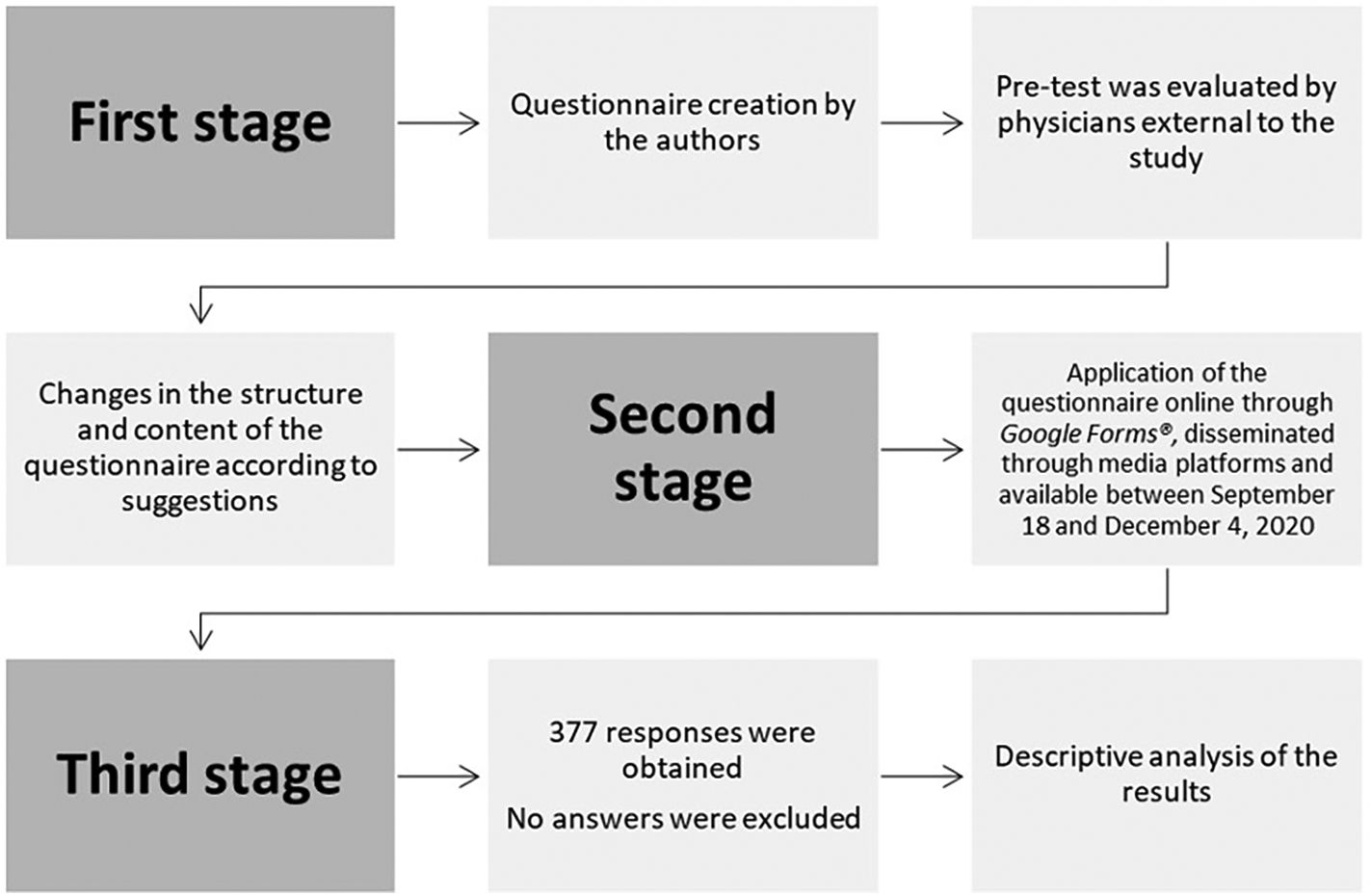
Material and methodsA cross-sectional study was conducted, with an analytical component, via the application of an online questionnaire. The applied questionnaire is available for consultation in full in appendix 1.
Study populationFamily Medicine physicians and residents who worked in a primary health unit belonging to portuguese NHS. The sample size was calculated based on the number of Family Medicine physicians in Portugal in 2019, according to Ordem dos Médicos statistics (7451)9, and the number of Family Medicine residents, according to Bilhete de Identidade dos Cuidados de Saúde Primários (Bi-CSP) (2227).10 The sample size was calculated using Sample Size Calculator by Raosoft®, for a population of 9678, with a prevalence of estimated response distribution of 50%, a confidence interval of 95% and an error margin of 5%. A sample size of 370 individuals was calculated. Retired physicians, physicians or residents with other specialties and physicians who didn't work in the Portugal NHS, the Autonomous Region of Madeira regional health service or in the Autonomous Regions of Azores regional health service were excluded from the study.
InterventionsAn online questionnaire was applied through Google Forms®. This questionnaire, consisting of 30 questions, was created by the authors and based on the pre-existing literature on the subject and was submitted to a pre-test by Family Medicine physicians and residents external to the study in order to evaluate the conceptual and theoretical structure. After the pre-test some changes were made to the structure and content of the questionnaire. Through the application of the questionnaire, it was possible to gather some sociodemographic data, such as sex, age, demographic region of work place, degree of medical differentiation and organization model of the health care unit of work. The different questions were grouped according to the subtopics to characterize. Thus, the questionnaire was divided into the following sections: teleconsultation characterization, teleconsultation preferences, obstacles, advantages and disadvantages and teleconsultation in the future. Each one of these sections was composed of a different number of questions. The invite to participate in the survey was sent through digital platforms to the target population. The questionnaire was available for answer between September 18th and December 4th, 2020. Every two weeks, the survey was reminded in the digital sharing groups and sharing through peer groups was encouraged.
Statistical analysisA statistical analysis using Microsoft Office Excel® and Statistical Package for the Social Sciences® 26th version was performed, namely a descriptive analysis with the valuation of frequency and prevalence for the studied variables.
Ethical considerationsThis project was submitted and approved by the Ethical Commission of Centro Hospitalar Universitário de São João / Faculdade de Medicina da Universidade do Porto and by the Ethical Commission of Administração Regional de Saúde (ARS) do Norte (appendix 2 e 3, respectively). Participation in the study required the acceptance of informed consent by the participants. This informed consent was described and preceded the online questionnaire.
Results377 responses were obtained. Most participants had ages between 25 and 34 years old (63,4%), with the second most frequent age range being between 35 and 44 years old (19,3%). Most participants were female (76,7%). As to the degree of differentiation the sample is balanced, comprising 48,8% of Family Medicine physicians and 51,2% of residents. (Table 1).
Sample characterization.
| Variable | n | % | |
|---|---|---|---|
| Sex | Female | 289 | 76,66% |
| Male | 88 | 23,34% | |
| Age (years) | < 25 | 1 | 0,27% |
| 25–34 | 239 | 63,40% | |
| 35–44 | 73 | 19,36% | |
| 45–54 | 25 | 6,63% | |
| 55–64 | 31 | 8,22% | |
| ≥ 65 | 8 | 2,12% | |
| Differentiation degree | Physician | 184 | 48,81% |
| Resident | 193 | 51,19% | |
| Country region | ARS* Alentejo | 6 | 1,59% |
| ARS* Algarve | 4 | 1,06% | |
| ARS* Centro | 60 | 15,92% | |
| ARS* Lisboa e Vale do Tejo | 94 | 24,93% | |
| ARS* Norte | 207 | 54,91% | |
| Madeira Regional Health Service | 5 | 1,33% | |
| Azores Regional Health Service | 1 | 0,27% | |
| Health Care Unit organization model | UCSP† | 47 | 12,47% |
| model A USF‡ | 87 | 23,08% | |
| model B USF‡ | 243 | 64,46% | |
ARS* - Administração Regional de Saúde (Region Healthcare Administration).
UCSP†- Unidade de Cuidados de Saúde Personalizados (Personalized Healthcare Unit).
USF‡ − Unidade de Saúde Familiar (Family Healthcare Unit).
Table 2 shows the teleconsultation characterization. 43,0% of the inquired said that they used to do teleconsultation before the COVID-19 pandemic. When asked about the use of teleconsultation during the COVID-19 pandemic the responses changed and the teleconsultations users increased to 99,5%. The favorite teleconsultation modality among the participants before and during the pandemic was without a doubt the phone call. On an increasing scale from 0 to 5, 36,3% of the doctors classify their degree of satisfaction with teleconsultation as positive, but we point out that 38,2% were neither satisfied nor dissatisfied.
Teleconsultation characterization.
| Variable | N | % | |
|---|---|---|---|
| Teleconsultation before the pandemic | Yes | 162 | 42,97% |
| No | 215 | 57,03% | |
| If yes, in what percentage? | ≤20% | 150 | 92,59% |
| 21–40% | 6 | 3,70% | |
| 41–60% | 2 | 1,23% | |
| 81–100% | 2 | 1,23% | |
| No answer | 2 | 1,23% | |
| If yes, in what modality? | Teleconsultation with phone call | 69 | 42,59% |
| Teleconsultation with phone call, Teleconsultation with e-mail | 77 | 47,53% | |
| Teleconsultation with phone call, Teleconsultation with e-mail, Teleconsultation with WhatsApp® | 1 | 0,62% | |
| Teleconsultation with video call | 4 | 2,47% | |
| Teleconsultation with video call, Teleconsultation with phone call, Teleconsultation with e-mail | 2 | 1,23% | |
| Teleconsultation with e-mail | 9 | 5,56% | |
| Teleconsultation during the pandemic | No | 2 | 0,53% |
| Yes | 375 | 99,47% | |
| If yes, in what percentage? | ≤20% | 21 | 5,60% |
| 21–40% | 93 | 24,80% | |
| 41–60% | 129 | 34,40% | |
| 61–80% | 93 | 24,80% | |
| 81–100% | 39 | 10,40% | |
| If yes, in what modality? | Teleconsultation with phone call | 121 | 32,35% |
| Teleconsultation with phone call, Teleconsultation with e-mail | 238 | 63,64% | |
| Teleconsultation with phone call, Teleconsultation with e-mail, Teleconsultation with Messenger®, Teleconsultation with phone message | 1 | 0,27% | |
| Teleconsultation with phone call, Teleconsultation with e-mail, Teleconsultation with WhatsApp® | 1 | 0,27% | |
| Teleconsultation with video call | 4 | 1,07% | |
| Teleconsultation with video call, Teleconsultation with phone call | 1 | 0,27% | |
| Teleconsultation with video call, Teleconsultation with phone call, Teleconsultation with e-mail | 6 | 1,60% | |
| Teleconsultation with e-mail | 2 | 0,53% | |
| Doctors' satisfaction with teleconsultation | 1 | 24 | 6,37% |
| 2 | 72 | 19,10% | |
| 3 | 144 | 38,20% | |
| 4 | 126 | 33,42% | |
| 5 | 11 | 2,92% | |
As to the teleconsultation modality, most participants (38,2%) prefer phone call exclusively, 16,7% video call exclusively and 16,7% phone call and/or e-mail. Nevertheless, video call is the modality most often considered as the one that best suits the Family Medicine practice (59,2%).
More than half of the participants considered management of Hypertension and Diabetes and general health appointments to be able to be done by teleconsultation. Also, 40,9% considered that acute diseases could be managed by teleconsultation. The preferences are shown in Table 3.
Teleconsultation preferences.
| Variable | N | % | |
|---|---|---|---|
| Preferred modality to perform teleconsultation by family doctors | None | 40 | 10,61% |
| Teleconsultation with phone call | 144 | 38,20% | |
| Teleconsultation with phone call, Teleconsultation with e-mail | 63 | 16,71% | |
| Teleconsultation with video call | 63 | 16,71% | |
| Teleconsultation with video call, None | 1 | 0,27% | |
| Teleconsultation with video call, Teleconsultation with phone call | 22 | 5,84% | |
| Teleconsultation with video call, Teleconsultation with phone call, Teleconsultation with e-mail | 11 | 2,92% | |
| Teleconsultation with video call, Teleconsultation with e-mail | 12 | 3,18% | |
| Teleconsultation with e-mail | 20 | 5,31% | |
| No answer | 1 | 0,27% | |
| Modality of teleconsultation considered most suitable to Family Medicine practice | None | 36 | 9,55% |
| Teleconsultation with phone call | 81 | 21,49% | |
| Teleconsultation with phone call, Teleconsultation with e-mail | 29 | 7,69% | |
| Teleconsultation with video call | 119 | 31,56% | |
| Teleconsultation with video call, None | 1 | 0,27% | |
| Teleconsultation with video call, Teleconsultation with phone call | 35 | 9,28% | |
| Teleconsultation with video call, Teleconsultation with phone call, Teleconsultation with e-mail | 53 | 14,06% | |
| Teleconsultation with video call, Teleconsultation with e-mail | 15 | 3,98% | |
| Teleconsultation with e-mail | 8 | 2,12% | |
| Medical actions possible to be performed by teleconsultation | First approach to acute illness | 212 | 56% |
| Follow-up of patients with acute diseases | 103 | 27% | |
| Follow-up of patients with chronic diseases | 257 | 68% | |
| Receiving exams and notify the patient | 309 | 82% | |
| Health education | 230 | 61% | |
| Therapeutic adjustments | 206 | 55% | |
| Evaluation of treatment response | 222 | 59% | |
| Therapeutic reconciliation | 85 | 23% | |
| Assess the need of Temporary Incapacity Certificate (absence from work) | 97 | 26% | |
| Medication and physiotherapy credential renewal | 279 | 74% | |
| None | 5 | 1% | |
| Type of consultation feasible to be performed by teleconsultation | Acute illness | 154 | 40,85% |
| Hypertension | 241 | 63,93% | |
| Diabetes | 210 | 55,70% | |
| Pregnancy | 42 | 11,14% | |
| Adult health | 259 | 68,70% | |
| Family planning | 68 | 18,04% | |
| None | 52 | 13,79% | |
The obstacles most frequently identified were “lack of appropriate resources (phoneline, camera, etc.)” (70%), “maladjustment of patient to the necessary means (e-mail, electronic device, …)” (64,5%) and “influence in doctor-patient relationship” (51,2%).
As to the main advantages of teleconsultation, 68,7% of the participants identified “better accessibility”, 63,1% “safety and infectious disease control” and 59,2% “reduction of time spent by the patient”.
The “impossibility to perform physical examination” and the “limitation on non-verbal communication” were the main disadvantages considered by the participants (81,2% and 70,6%, respectively). table 4 presents all the obstacles, advantages and disadvantages selected by the participants.
Obstacles, advantages and disadvantages.
| Variable | N | % | |
|---|---|---|---|
| Main obstacles identified by family doctors | No warranty of privacy and data protection | 51 | 13,53% |
| Difficulty in managing/organizing the agenda | 178 | 47,21% | |
| Lack of appropriate resources (phoneline, camera, internet connection, software, …) | 264 | 70,03% | |
| Maladjustment of professionals to the necessary means (e-mail, software, hardware, …) | 10 | 2,65% | |
| Maladjustment of patient to the necessary means (e-mail, software, …) | 243 | 64,46% | |
| Non-adherence of patient to teleconsultation | 145 | 38,46% | |
| Difficulty communicating with the patient | 191 | 50,66% | |
| Influence in doctor-patient relationship | 193 | 51,19% | |
| Lack of health professionals training in teleconsultation | 43 | 11,41% | |
| No obstacles | 2 | 0,53% | |
| Main advantages of teleconsultation | Improvement of doctor-patient relationship | 4 | 1,06% |
| Better accessibility | 259 | 68,70% | |
| Costs reduction for the patient | 107 | 28,38% | |
| Reduction of time spent by the patient (dislocation, waiting room, …) | 223 | 59,15% | |
| Better surveillance/follow up | 17 | 4,51% | |
| Better management of doctor's agenda | 56 | 14,85% | |
| Greater consultation adherence | 11 | 2,92% | |
| Safety and infectious disease control | 238 | 63,13% | |
| Greater convenience for the patient | 134 | 35,54% | |
| Greater convenience for the doctor | 29 | 7,69% | |
| Possibility of telecommuting (from home, …) | 123 | 32,63% | |
| Greater patient responsibility and autonomy | 65 | 17,24% | |
| No advantages | 22 | 5,84% | |
| Main disadvantages of teleconsultation | Damage of doctor-patient relationship | 166 | 44,03% |
| Non warranty of privacy/ data protection | 43 | 11,41% | |
| Limitation on non-verbal communication | 266 | 70,56% | |
| Influence in diagnostic (overdiagnosis) | 104 | 27,59% | |
| Influence in diagnostic (underdiagnosis) | 142 | 37,67% | |
| Unnecessary exams prescription | 157 | 41,64% | |
| Not accessible to all population | 161 | 42,71% | |
| Overmedication | 15 | 3,98% | |
| Impossibility on performing physical examination | 306 | 81,17% | |
| Difficulty in communication (anamnesis, medication dosage, …) | 139 | 36,87% | |
| Consultation duplication (possibility of not avoiding a face-to-face consultation) | 156 | 41,38% | |
| Patient discontent | 77 | 20,42% | |
| No disadvantages | 0 | 0,00% | |
88,6% of the participants considered the patient should have the possibility to opt for a face-to-face consultation each time the doctor suggests a teleconsultation.
The majority of the participants acknowledge that teleconsultation represents a valuable asset to the future of medicine (83,6%) and about 80,6% of the doctors would like to implement a teleconsultation period in their schedule.
In the opinion of the Family Doctors that participated in the study, neither the portuguese population nor the portuguese Family Doctors are ready for teleconsultation (73,5% and 63,7%). 78,3% think that it would be relevant to have training in this area.
In the opinion of 78,1% of the surveyed doctors, teleconsultation will become essential to future clinical practice. Table 5 shows the results related to the future perspective of teleconsultation.
Teleconsultation in the future.
| Variable | N | % | |
|---|---|---|---|
| Time spent on a teleconsultation versus a face-to-face consultation | Less | 105 | 27,85% |
| Equal | 180 | 47,75% | |
| Longer | 92 | 24,40% | |
| Should the patient have the right to ask for a face-to-face consultation when a teleconsultation is suggested? | No | 43 | 11,41% |
| Yes | 334 | 88,59% | |
| Will teleconsultation be a valuable asset in the family doctors' future clinical practice? | No | 62 | 16,45% |
| Yes | 315 | 83,55% | |
| Are you considering implementing a teleconsultation period in your schedule in the future? | No | 73 | 19,36% |
| Yes | 304 | 80,64% | |
| If you consider implementing a teleconsultation period in your Schedule, in what percentage? | ≤20% | 163 | 53,62% |
| 21–40% | 117 | 38,49% | |
| 41–60% | 22 | 7,24% | |
| 61–80% | 1 | 0,33% | |
| Is the portuguese population ready for teleconsultation? | No | 277 | 73,47% |
| Yes | 100 | 26,53% | |
| Are portuguese family doctors' ready for teleconsultation? | No | 240 | 63,66% |
| Yes | 137 | 36,34% | |
| Would it be relevant to have training in teleconsultation? | No | 82 | 21,75% |
| Yes | 295 | 78,25% | |
| Will teleconsultation become essential in the future clinical practice? | No | 90 | 23,87% |
| Yes | 287 | 76,13% | |
Overall, there are few published studies on the perspective of family doctors about telemedicine during the pandemic. Studies previous to the pandemic on telemedicine in primary health care address specific areas as teledermatology or follow-up of specific pathologies/complaints or address the study of platforms that allow the integration of patient data and discussion between specialties; there are also guides and protocols with recommendations on the practice of telemedicine. 11–14
For example, in the late 2020, due to the necessity created by the pandemics, a practice pointer, that summarized the evidence on the use of video consultations in healthcare and offered practical recommendations for its implementation, both for doctors and patients, was published. This practice pointer was also directed to primary health care. This article highlights that in some countries, such as the United Kingdom and the United States of America, doctors are now permitted to use non-medical digital platforms for video consultations, like Skype®, WhatsApp® and FaceTime®.15 In Portugal, the RSE Live® platform was developed, allowing teleconsultations to be carried out since 2018. This app allows health care professionals to perform real time teleconsultation with the patients and also between professionals.16,17 However, despite the platform creation prior to the pandemic, our study reveals that teleconsultation by phone call was preferred by portuguese Family Doctors over video consultation.
Nevertheless, the COVID-19 pandemic, by hastily boosting the use of teleconsultation, had a great influence on teleconsultation's impact on health care services and on the capability of doctors to adapt to it.
Primary care managed the main share of COVID-19 related care and, during the pandemic, continued to function in many countries as the first point of contact for a broad spectrum of patients.18 Thus, it's essential the optimization of these resources in primary care settings. Although this investigation showed that most participants have an interest in implementing a teleconsultation period in their schedule and recognized that teleconsultation represents a valuable asset to the future of medicine, they also think that neither the portuguese population nor the portuguese Family Doctors are prepared for this type of consultation. In fact, most respondents expressed the need to have training in this area, findings also found in a spanish study where the majority of the participants considered that training was needed for video consultation.19
This study shows that the main advantages of teleconsultation are greater accessibility, safety in terms of infection control and reduction in the time spent by the patient. As disadvantages, the study identified primarily the impossibility on performing physical examination, the limitation in non-verbal communication and the damage of doctor-patient relationship, findings that agree with the ones from Gomez T, et al. study.20 It should also be noted that none of the participants thought that there would be no disadvantages with teleconsultation, so it is consensual that teleconsultation will always have some harm associated.
This study showed that, with the pandemic, teleconsultation started to have more users, but the most used modalities were the same as before, namely the phone call and the e-mail. The video call, although considered the most suitable, keeped relatively low usage rates, which may be related with the lack of technology, by both the doctor and the patient, with the physician's preference or with the lack of infrastructures to maintain a safe and effective communication. This findings are also discussed in an UK reflection article about the impact of COVID-19 pandemic on primary care.21 Furthermore, they also point out that, given that the remote consultation can be difficult for marginalized groups in society, traditional means of consultation must remain available when needed.21 These facts are also confirmed by the participants in the present study, who claim as main obstacles the lack of appropriate resources and the maladjustment of patients to the necessary means to teleconsultation. Moreover, most admit that the patient should always have the option to opt for a face-to-face consultation when the doctor suggests a teleconsultation. In Australia, a guide for appropriate use of telephone and video consultations for General Practitioners was developed.22 This guide underlines the need for General Practitioners and practice teams to ensure that patients are informed about the option to continue attending the practice for consultation if this is clinically appropriate and safe for the patient, practice staff and the community.22
It's known that teleconsultation can improve patient accessibility, reduce consultation duration and it's associated with greater satisfaction by patients and physicians.23 Particularly regarding satisfaction, a 2020 review described the determinants of satisfaction with telemedicine and how they compared with in-person visits from both the perspective of patients and of providers.24 This review suggested that the expansion of telemedicine depends on the satisfaction of both intervenients, patients and doctors. It also reported a 95–100% satisfaction rate from patients with telemedicine when compared with in-person appointments.24 In our study, the satisfaction of doctors with teleconsultation was positive. However, the patients were not included in the target population, therefore their satisfaction was not assessed. In the authors' opinion more studies are necessary in order to perceive patient satisfaction with teleconsultation in the portuguese population.
So, more studies are necessary to investigate the influence of teleconsultation on clinical practice, particularly with regard to the doctor-patient relationship, the quality of care provided, the adherence to treatment and the possible violation of data protection policy. Investigations focused on the patient perspective would also be important in the development of this matter. Our investigation allowed us to know for the first time the perspective of portuguese Family Doctors on teleconsultation and it showed that, in their opinion, teleconsultation will be a valuable asset in the future. That said, it is imperative to develop more studies that deepen the knowledge in this promising area.
ConclusionThe COVID-19 pandemic changed the clinical practice of the portuguese Family Doctors with an increase in the use of teleconsultation. The favorite method of teleconsultation was the phone call, although most of the participants found video call to be the most suitable one for primary care practice. The main obstacles identified were the lack of adequate resources, the maladjustment of the patient and the influence in doctor-patient relationship. The most consensual advantages were greater accessibility, safety and the reduction of the time spent by the patient; as to disadvantages, the limitation in non-verbal communication, the damage in the doctor-patient relationship and the impossibility of performing physical examination were pointed out.
Most participants are interested in implement a teleconsultation period in their schedule. However, and despite recognizing teleconsultation as an essential ally in medical practice in the future, the doctors that participated in the study also acknowledge that, currently, neither the portuguese population nor the portuguese Family Doctors are prepared for teleconsultation, being considered relevant training in the area.
Financial sourcesThere were no external financial sources for this article.
EthicsObtained the assent by the Ethics Committee of Centro Hospitalar de São João/Faculdade de Medicina da Universidade do Porto and Ethical Commission of Administração Regional de Saúde (ARS) do Norte.
Key points| What is known on the topic:The COVID-19 pandemic led to a mass use of teleconsultation, but little is known about physicians' perception of this type of consultation.Is essential to reflect on the advantages and disadvantages of this type of consultation and the perspective of Portuguese Family Doctors on teleconsultation as a tool in their future clinical practice. |
| What this study contributes:Most participants are interested in implementing a teleconsultation period in their schedule.Despite recognizing teleconsultation as an essential ally in medical practice, it is also recognized by the participant doctors that currently neither the Portuguese population nor the Portuguese Family Doctors are prepared for teleconsultation. |