Diabetes is one of the growing health problems in the Middle East región in general and Saudi Arabia in particular. The increasing number of the population and changes in the pattern of life in the region expose a large number of the population to diabetes and its complications. The following review discusses the magnitude of the diabetes problem in Saudi Arabia, diabetic peripheral neuropathy, diabetic arterial disease, diabetic foot and the impact of education to prevent diabetic foot diseases on the outcome of diabetic foot problems. According to my knowledge, this is the first review which shows the magnitude of diabetic foot problems and its risk factors in Saudi Arabia.
The Diabetes Education Study
diabetic peripheral neuropathy
peripheral arterial disease.
The Kingdom of Saudi Arabia has undergone a lot of changes in different aspects of daily life habits towards westernization. According to Khan,1 increasing trends in the per capita availability of total food (90%), oils and fats (200%), animal fat (171%), animal protein (207%), meat (313%), milk (120%), eggs (648%) and sugar (68%) have been observed in Saudi Arabia over the period of the Sixties and the Seventies. These changes in the dietary pattern during the short span of two decades mimic a transition that took 137 years in Japan and 200 years in the United Kingdom.2
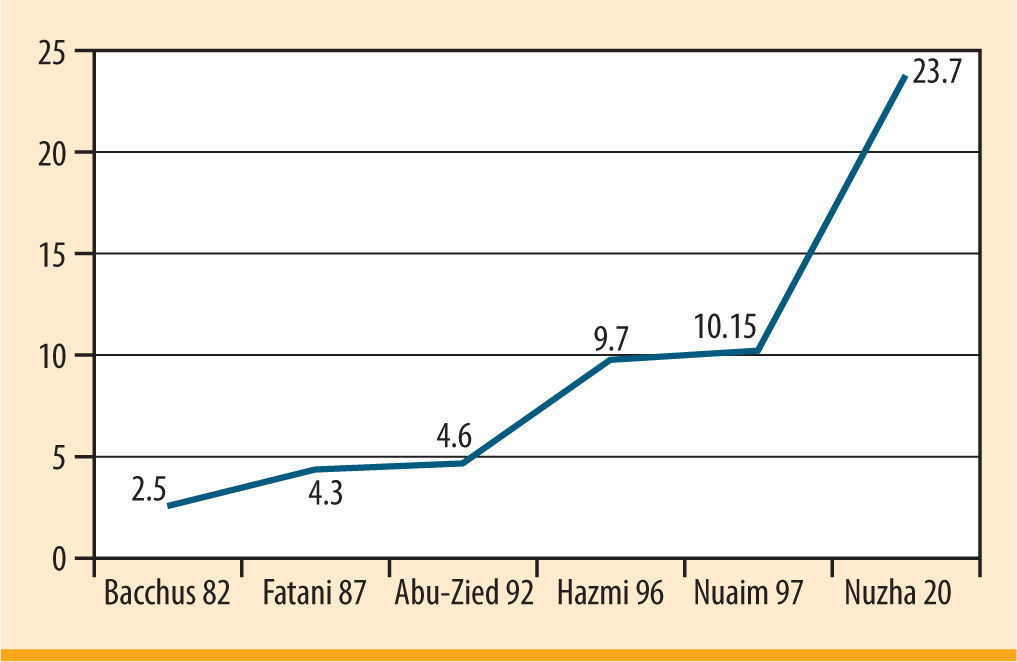
In recent decades rapid demographic changes have taken place in the form of increasing urbanization in many parts of Saudi Arabia. In the early 1970s, 25% of the Saudi Arabian population lived in urban areas; by the early 1990s more than 75% where living there.3,4 Living in a urbanization has changed the pattern of life style of the population. A steady increase in diabetes prevalence has been detected in Saudi Arabia (figure 1).
In 1982, Bacchus RA,5 published the first study estimated prevalence of diabetes in Saudi Arabia the sample included males of all ages, the percentage obtained was of 2.5%. Interestingly the prevalence of diabetes started to increase at 35 years of age reaching its peak at the 45-54 age groups.
An interesting paper published in 1987 by Fatani,6 reported an overall prevalence of 4.3% .Also the steady rise of prevalence according to age was noticed in this paper. The prevalence was 7% and 10.2% among males aged 35-54 and >55 years respectively and 16% and 18.7% among females aged 35-54 and >55 years old respectively. In 1992 Abu-Zeid and Al-Kassab,7 found that the overall prevalence of diabetes mellitus was 4.6%. Interestingly in this study the prevalence of diabetes in Southern Arabia Saudi among men was of 17% and 22% among men aged 41-50 years and 51-60 years respectively and 11% and 26% among women aged 41-50 years and 51-60 years respectively.
In 1996 El-Hazmi MA et al.,8 reported the results of one of the national surveys done in Saudi Arabia to quote the prevalence of diabetes mellitus. He stated that the overall prevalence of diabetes in the survey was of 9.7%.
After a short time, the result of another national survey,9 published in Diabetes Medicine journal. In this survey the results showed that the age adjusted prevalence of DM was significantly higher in the urban population (males 12%, 95% CI= 11-13 and females 14%, 95% CI= 13-15) than in the rural population (males 7%, 95% CI= 7-8 and females 7.7%, 95% CI= 7-9) which is among the highest in the world.
In 2004, Al-Nozha,10 reported in his national survey for risk factors for coronary artery diseases that the prevalence of diabetes had reached 23.7%. Table 1 showed the key studies done in Saudi Arabia to show the prevalence of diabetes mellitus.
Prevalence of diabetes mellitus in Saudi Arabia
| Study | Year | Age | Prevalence |
| Bacchus, et al.5 | 1982 | 1,385 malesAll age group | 2.5% |
| Fatani et al.6 | 1987 | 5,222males | Over all 4.3%W 5.9%M 2.9% |
| Abu-Zeid et al.7 | 1992 | 2,150Semi urban>10 years | Over all prevalence4.6% |
| El-Hazmi et al.8 | 1996 | 14,660 participants>14 years | 9.7% |
| Al-Nuaim et al.9 | 1997 | 13,177 participants≥15 years | Urban:M 12%W 14%Rural:M 7%W 7.7% |
| Al-Nozha et al.10 | 2004 | 16,917 participants30-70 years | 23.7% |
It is interesting to point out that Al-Nozha et al. had conducted his survey among a groupof the population exposed to multiple risks which favor the development of diabetes (age group >30 years) ,so in my opinion this was backed up by the high prevalence reported in the survey (23.7%). On the other hand if we looked at other studies,5–9 including participants from lower age groups we will notice a low prevalence of diabetes.
In my opinion I think it is important to mention the age group when we talk about prevalence of diabetes in Saudi Arabia (table 1).
Obesity is another health problem among the population of Saudi Arabia and is considered as a risk factor for diabetes and diabetic foot problems.
El-Hazmi and Warsy,11 reported in their national survey which took place in 1997 that the prevalence of overweight in the Saudi population was of 22.23% and 25.20% in males and females respectively while obesity was 13.05% and 20.26% in males and females respectively. In 2005, Al-Nozha et al.,12 reported a new prevalence rate for overweight and obesity. For overweight, it was 42.4% and 31.8% for males and females respectively, and for obesity it was 26.4% and 44% for males and females respectively. The prevalence of gross obesity (BMI >40 m/kg2) was of 3.2%.12
The high prevalence of inactivity among Saudis represents a major public healthconcern. Al-Nozha et al.,13 showed that the prevalence of inactivity among participants (N = 16,917) included in the national survey done between 1995-2000 for the risk of coronary artery diseases in Saudi Arabia was of 96.1% which is very high. There were significantly (p <0.001) more inactive females (98.1%) than males (93.9%). Inactivity prevalence rises with increasing age category, especially in males, and decreases with the increase of education levels. Inactivity was the highest in the central region (97.3%; 95% CI = 96.8-97.8%) and the lowest in the southern region of Saudi Arabia (94.0%; 95% CI= 93.294.8%).13
In 2008, Al-Nozha et al.,14 published data which showed the prevalence of dyslipidemia among the population of Saudi Arabia. They found that the prevalence of High Cholesterolemia (total cholesterol > 5.2 mmol/L) was 54% with mean cholesterol level of 5.4±1.52 mmol/L. The prevalence of High Cholesterolemia among males was of 54.9% and 53.2% among females, while it was 53.4% among urban Saudis and 55.3% among rural Saudis. For hypertriglyceridemia (total triglycerides ≥1.69 mmol/L). The prevalence was of 40.3% with mean triglycerides level of 1.8±1.29 mmol/L. Males had statistically significant higher hypertriglyceridemia (p <0.0001) with prevalence of 47.6% compared to 33.7% in females.
Smoking was another health problem in Saudi Arabia. It is difficult to determine the actual prevalence of smoking due to multiple social and religious barriers, so there was a considerable variation on the prevalence of smoking in studies done in Saudi Arabia. Al-Haddad NS, Al-Habeeb TA, Abdelgadir MH, Al-Ghamdy YS and Qureshi NA,15 concluded on their study published in 2003 that the prevalence of smoking in the region of Al-Gassim was of 52.3%. Interestingly 85% were adult smokers, 8.6% began smoking before the age of 12. Smokers gave overlapping reasons to smoke including peer pressure; non-smokers gave religious and health resons against smoking. Of all smokers, 92.8% wanted to learn cessation strategies, 11.8% were ignorant of dangers and 32.4% reported manifestations of nicotine withdrawal.
In another study,16 done among health staffs in a primary care unit in a general hospital in Riyadh, the prevalence of smoking was 19% while it was 14% for ex smokers.
Jamal S Jarallaha et al.17 concluded that the overall prevalence of smoking was 21.1% for males and 0.9% for females. Most smokers (78%) were young to middle-aged (21-50 years old). Smoking prevalence was higher among married people, among uneducated people, and among those in certain occupations: manual workers, businessmen, army officers, and office workers.17
In conclusion, the changes in demography of Saudi Arabia, the pattern of life style and the acquiring of bad medical habits like tobacco smoking were the causes that raised the prevalence of type 2 diabetes mellitus in Saudi Arabia and expose a large number of the population with diabetes complications.
Risk factors for diabetic footFoot examination and risk categorization were among the least concerned examinations by most of the physicians dealing with diabetes.
In a cross sectional study conducted in Gurayat province,18 among primary care physicians to evaluate the current referral system between the diabetic center and the primary health care centers, only 3 referral forms (of a total of 215 forms) contained data about foot examination.
Peripheral diabetic neuropathy (PDN) and peripheral arterial disease (PAD) were the main determinant risk factors for the occurrence of diabetic foot. Loss of protective sensation backs up many of diabetic foot ulcers.
Poor glycemic control is considered one of the poor vaticinator of diabetic foot lesions.
Faiza A Qari and Daad Akbar,19 reported that 79% (27/34) of their studied patients were uncontrolled.
Al-Nuaim AR et al.,20 in their study looked for the pattern and factors associated with glycemic control of Saudi Arabia diabetic patients and reported that 50% of the patients with type 2 diabetes that they studied have an uncontrolled diabetes (Random blood glucose >10 mmol/L). In this study,20 patients with poor glycemic control were significantly older than patients with good glycemic control (p = 0.0001).The researchers concluded insulin therapy is most certainly underutilized, given the high rate of poor glycemic control, high rate of relative poor glycemic control and high rate of relative occurrence of complications among Saudi Arabia diabetic patients. In another study done by Faiza A Qari,21 which compared the glycemic control among diabetic patients at the University and Erfan private hospital. Concluding that even after great efforts, a target level of HbA1c was not achieved in both groups of patientsin private and governmental hospitals.21 Only 58% at King Abdulaziz University Hospital versus 54% at Erfan group were achieved acceptable level (HbA1c <8%).21 Even in primary health care service, the glycemic control was not so good. In a study done by Azab AS,22 targeted patients with diabetes attending primary health care centers in Riyadh (991 diabetic patients were involved), 21% of patients achieved an excellent glycemic control in the first reading and 25% in the second reading (fasting blood glucose <10 mmol/L) while those with poor control represented 49% and 44% of the patients in two readings (fasting blood glucose >10 mmol/L).22
Diabetic peripheral neuropathyDiabetic peripheral neuropathy (DPN) is a common complication of diabetes mellitus that eventually affects the majority of diabetic patients and is associated with significant morbidity and disability.23 It affects sensory, autonomic and motor neurons of the peripheral nervous system. The prevalence of diabetic peripheral neuropathy varies widely due to the different diagnostic criteria.
Epidemiological cross-sectional studies are the most appropriate studies to draw valid conclusions regarding the prevalence of diabetic neuropathy if they are population-based and can obtain response rates. In contrast, hospital-based studies may not reflect the true prevalence of this complication. Recommendations for standardized classification of diabetic neuropathy made by The American Diabetic Association and Academy of Neurology include measurement of at least one parameter of five main categories: symptom profiles, neurological examination, quantitative sensory testing, nerve conduction studies and autonomic function testing.24
It is estimated from a comprehensive collection of epidemiologic studies that the prevalence of neuropathy in patients with is of approximately 30% in hospital patients and 20% in community patients.25
In 1994, Kumar et al.,26 reported a higher prevalence rate (41.6%) of neuropathy among patients with type 2 diabetes in a population-based study in three cities in the United Kingdom. While the prevalence was 26% in the Oxford community-based study,27 which did not include patients over 75 years of age.
Reported prevalence of neuroarthropathy among diabetic patients of Saudi Arabia was very scarce in literature.
Nielsen JV,28 reported a prevalence of 38% among Saudi patients with type 2 diabetes with duration of 10 years. In the same study a comparison of 212 Saudi diabetic patients in the age group from 46-69 years were compared with Swedish patients with type 2 diabetes. No significant difference was noticed between the two groups.28
Abdulrahman Al-Tahan,29 in his paper published in 1994 on the Saudi medical journal reported that the prevalence of diabetic neuropathy was 33.9% and it was the commonest encountered type of neuropathy among the Saudi population.
An interesting paper published in Bahrain medical bulletin by Daad H Akbar,30 discussed the discordance between symptoms and electrophysiological testing in Saudi diabetic patients in diagnosing diabetic neuropathy. It was a cross sectional study of Saudi diabetic patients with symptoms of neuropathy followed up in medical outpatient clinic at King Abulaziz University Hospital, between January 1998 and May 1999, neuropathy was diagnosed using the Michigan neuropathy program.30 The prevalence of normal nerve conduction was 36% and the abnormal conduction was 64%.30
Another interesting study done by Abdulsalam A Al-Sulaiman, Hassan M Ismail, Ali I Al-Sultan,31 studied nerve conduction abnormalities among newly diagnosed diabetic patients with type 2 diabetes (within 4 weeks from the diagnosis). The researchers found the presence of these abnormalities in all participants (29 patients) which meant that the prevalence of neuropathy based on their criteria was of 100%.31
An interesting paper,32 published in the Saudi journal of kidney disease and transplantation found that the prevalence of diabetic neuropathy was of 66.8%. This study concluded that baseline creatinine clearance and proteinuria, high systolic blood pressure, advanced age and longer duration of diabetes were the most significant risk factors for developing complications.32 The interesting part of this study is that from the following complications; angiographically proven coronary artery disease, stroke, myocardial infarction, angina, retinopathy, blindness, peripheral vascular disease, neuropathy, hypertension, diabetic foot, amputation and end stage renal disease, 37% of patients developed >6 concomitant complications, 28% developed 5 concomitant complications, 17% developed 4 and the rest developed <3.32 This finding may explain the high prevalence of neuropathy among these patients.
Akbar DH, Mira SA, Zawawi TH, Malibary HM,33 in their paper published in 2000 in the Saudi medical journal pointed to subclinical diabetic neuropathy which they considered it as a common complication in Saudi diabetic patients. They conducted prospective study extended from January 1998 until April 1999. Patients were assessed for diabetic neuropathy using the Michigan Neuropathy Program.34 Symptomatic diabetic neuropathy was found in 56% while sub clinical neuropathy was found in 57% of asymptomatic patients.33
Qidwai SA, Khan MA, Hussain SR and Malik MS,35 published in the Saudi medical journal in 2001 is among those few studies done on this area. The researchers conducted retrospective study based on reviewing medical records of 296 diabetic patients between June of 1998 and July of 1999. Included participants had long standing, poorly controlled diabetes mellitus and associated peripheral neuropathy.35 Participants were evaluated clinically and radiologically for the presence of neuroarthropathic changes in the feet. The researchers found that the prevalence of diabetic neuropathy was 12.5% and 4% for neuroarthropathy.35 The joints involved were tarsometatarsal (76%), metatarsophalangeal (59%), subtalar (47%) and interphalangeal joints (41%).35
Peripheral arterial disease- •
The prevalence of peripheral arterial disease (PAD) is higher among diabetic than non-diabetic patients in both population and hospital based studies.36,37 True prevalence of PAD in people with diabetes has been difficult to determine due to:
- •
Most of the patients are asymptomatic
- •
Many do not report their symptoms
- •
Screening modalities have not been uniformly agreed upon
- •
Pain perception may be blunted by the presence of PAD
Data from the Framingham Heart Study,38 revealed that 20% of symptomatic patients with PAD had diabetes.
When using pulse deficits as criterion for detection of PAD, the researchers on the Rochester, MN survey,39 which was a population based survey among diabetic patients diagnosed in 1,945 – 69 found that 8% had PAD at the time of initial diagnosis of diabetes.
In an epidemiological study,38 involving two residential areas in Chennai in South India with 1262 participants aged >20 years using a Doppler to detect PAD with a cut value of 0.9, the researchers found that among normoglycemic patients the prevalence rates of PVD were of 2.7%, among those with impaired glucose tolerance 2.9% and among diabetic patients it was 6.3%.
Sulatn O Al-Sheikh et al.40 conducted a prospective cross sectional study which included 471 Saudi patients aged ≥45 years attended the primary health care center at King Khalid University Hospital between February – March 2006, using ABI <0.9 to define PAD. They found that the prevalence of PAD was 11.7% and 92.7% of them were asymptomatic.41
Faiza A Qari and Daad Akbar,42 retrospectively studied medical notes of 34 diabetic patients admitted to King Abdulaziz University Hospital in Jeddah from June 1997 to June 1999 with diabetic foot. They concluded that 50% of those patients suffered from PAD.42
Sulimani RA, Famuyiwa OO, Mekki MO,43 in their retrospective study which was carried out to estimate the magnitude and pattern of foot lesions seen in King Khalid University Hospital among diabetic patients found that the prevalence of PAD was of 54.5%.43
AbdulRashid S and Ashar AK,44 in their paper published on the journal of surgery of Pakistan reported the results of an analysis of 50 cases of amputations done at Al-Noor Specialist Hospital in Mekkah, found that there were 43/48 (86%) amputations due to diabetes with peripheral neuropathy and circulatory disorder .
Almoutaz A.Ahmed in his review done in 2006 about the epidemiology of diabetes in Gurayat province found that the prevalence of PAD among patients with type 2 diabetes attending the diabetic center in the province was of 10.5% using symptoms and pulse deficit as criteria for PAD.45
Al-Wakeel et al.,46 studied 184 diabetic patients with nephropathy between Jan 2003 – June 2006. Researchers found that the prevalence of peripheral vascular disease was of 65.7%.44 This study concluded that baseline creatinine clearance and proteinuria, high systolic blood pressure, advanced age and longer duration of diabetes were the most significant risk factors for developing complications.46
EducationEducation is one of the important issues that need to be covered well in patients with diabetes.
The Diabetes Education Study (DIABEDS),47 was a randomized, controlled trial of the effects of patient and physician education. Patients randomly assigned to experimental and control groups. Patients in the randomized experimental group were offered up to seven modules of patient education. The results of the study showed that there was significantly greater reductions in fasting blood glucose between experimental and control group (−27.5 mg/dL versus −2.8 mg/dL, p <0.05) and glycosylated hemoglobin (−0.43% versus + 0.35%, p <0.05) as compared with control subjects.47
Iftikar Uddin, Tahir J. Ahmed, AbdurRahman A.Kurkuman and Rahila Iftikar,48 found that education is significantly effective in controlling blood glucose (p <0.005).
The mean fasting blood glucose before education started among participants was 10.7 mmol/L and became 7.3 mmol/L after education.48
Alkhaldi YM and Khan MY,49 published an interesting paper auditing diabetic a health education program applied to diabetic patients (198 patients) at a large primary health care center in Asir region. The researchers found that compliance to appointment was good in 60% and poor in 30% of diabetic patients.49 Also, they found that 73% of diabetic patients had received at least one health education topic, 27% did not received any health education at all, only 33% of diabetic patients had adequate health education.49 Eighty percent (80%) were questioned about diabetes and 77% were educated about the diets role. They also found that the essential structure for the diabetes education program was found to be unsatisfactory and recommended a structured education program to be applied.49
Another interesting study done in a primary health care center in Abha,50 where 475 diabetic patients were registered and followed up, the files of 198 diabetic patients who fulfilled the inclusion criteria set for this study were reviewed.50 The aim of this study was to examine the impact of health education delivered in the PHC setting on the control of diabetes and to investigate any gender difference affecting the validity of health education message. Males received significantly more health education sessions (4.2+1.9 versus 1.8+1.3 p <0.01).50 Females had significantly poorer diet compliance than males (p <0.05). The researchers concluded that the only significant factor predicting poor glycemic control was the sex of the patient showing that females are more prone to hyperglycemia and poor control of their diabetic state than males (OR = 2.84) and recommended that the female patients should be taken into account when designing health education messages.50
Organized follow up using a structured follow up sheet showed significant outcomes. Moharram MM and Farahat FM,51 showed that the use of a flow sheet would improve performance of family physicians in diabetes care. Based on one year intervention study conducted in 7 family practice clinics in Taif Armed Forces Hospitals, Taif, Saudi Arabia from March 2006 to June 2007, the researchers concluded that a flow sheet can be effective in improving quality of care not only for diabetes but also for other chronic conditions.51
Mohammed H. AlDoghether,52 in his study assessed whether it is possible by diabetic foot reminder to improve foot examination of diabetics in primary health care centers.52 The researcher used pre and post evaluation to measure the effect of the content of the education on the quality of foot examination. The results showed that there was a dramatic improvement on performing foot examination after using the reminder over 4 months52. Further improvement might be expected over applying the reminders during a year or more. The researcher informed that one of the main reasons for the success in implementing the diabetic foot examination reminder is the employment of multidisciplinary approach.
In conclusion, education was found to be effective to improve glycemic outcome but unfortunately, there is a lack of research in this area and few studies were published which tested the effectiveness of education in Saudi diabetic patients.
Dermatological foot diseasesLiterature search for dermatological diseases of the foot among Saudi diabetics' patients refilled very scanty publications.
An interesting national survey done by Sammer K. Zimmo published in 2007,53 reviewed the common dermatological foot diseases among 4,401 Saudi individuals. This survey showed that 43% of the participants had foot diseases. The prevalence of fungal infection was of 19.9%; and 15.52% of them suffered from Tinea Pedis, 5.56% from Onychomycosis and 23% from non fungal diseases.53
Of all participants 5.5% had warts and 3.68% had corns.53 Skin examination showed that 57% of affected patients had planter hyperkeratosis. 45% had fissures, 10% ulceration. 53
Diabetes was the third prevalent cause for dermatological foot diseases (12%) proceeded by dermatological diseases (42%) and obesity (13%).53
Diabetic footUlceration of the foot in diabetes is common and disabling and frequently leads to amputation of the leg.
In a community survey done in the United Kingdom, the prevalence of diabetic foot ulcers was 5.3% in patients with type 2 diabetes.27 Also they found that 7.4% of patients with type 1 and 2 diabetes had a history of active or previous foot ulcers. 27 In USA in a hospital based survey done by Ramsey SD and his colleagues found the prevalence was of 5.8%.54
In another survey done in Netherlands, a mean incidence of new ulceration among patients with type 2 alone was found to be 2.1% annually.55
In a study done in Iran by Afsaneh Alavi56 done to examine the characteristics of patients with diabetic foot ulcers attending an outpatient diabetic clinic in Kerman province which is located in the southeastern of Iran, the investigator examined 247 patients with diabetes with mean age 52+12 years, the prevalence of diabetic foot was 4%, callus 12% and 50% for heal cracks.56
Nielsen JV28 found that the prevalence of diabetic foot was 4.7% among a sample of 375 Saudi patients with type 2 diabetes. He did a comparison with Swedish diabetic patients (age group 46-69 years), prevalence of ulcers was (2.3%) in Saudi group which was significantly lower than in Swedish patients. This conclusion may be explained by different styles of footwear.28
Faiza A Qari and Daad Akbar,19 in their paper reported that 59% of their studied patients had foot ulcers 19 and 65% of these patients with ulcers need Debridement.
In 1991, Sulimani RH et al,43 in a retrospective study stated that the prevalence of diabetic foot lesions was found to be 10.4%.
In another study,32 done in King Khalid University Hospital, Riyadh from January 2003 to June 2006 which included 184 diabetic nephropathy patients who were referred to nephrology clinic; the researchers found that the prevalence of diabetic foot was of 13.5%. Also the researchers in this study concluded that baseline creatinine clearance and proteinuria, high systolic blood pressure, advanced age and longer duration of diabetes were the most significant risk factors for developing complications.32
Qari FA,57 in her study which aimed to know the characteristics and risk factors of 13 diabetic patients undergoing chronic hemodialysis at King Abdulaziz University Hospital in Jeddah found that 7.7% of the participants had gangrenous foot. She explained her findings due to poor glycemic control, inadequate treatment of hypertension, high smoking rate and an inadequate screening for microalbuminuria.57
Amputation among patients with diabetic foot problemsThe prevalence of amputation among diabetic patients in Saudi Arabia varied between studies, variation in prevalence of peripheral arterial diseases and other risk factors and availability of appropriate health services may explain that.
Sulimani RA and his colleagues,43 in a retrospective study carried out to estimate the magnitude and pattern of foot lesions detected in diabetic patients living in Saudi Arabia showed that the amputation rate was significantly high among those with diabetic foot lesions. Thirty patients out of 88 patients (34.1%) with diabetic foot lesions have undergone amputation. The analysis of the foot lesions showed that 10 cases had cellulites, 33 cases had ulcers, 29 cases had gangrene and 16 cases had abscesses. Interestingly from those with diabetic foot lesions, 48 patients (54.5%) suffered from PAD and 43 patients (48.8%) suffered from peripheral neuropathy. In this study,43 the overall prevalence of amputation was of 3.2%
Meshikhes A.-W. N et al.,58 in 1998 published an interesting Retrospective review of the case notes of 68 diabetic patients presented with foot sepsis and treated in a department of Surgery, Dammam Central Hospital, Dammam, Eastern Province, Saudi Arabia over a 2 year period from January 1st, 1994 to December 31st, 1995. Forty patients (59%) were observed to have amputation. There were 8 (13%) complications: amputation stump infections (two), flap necrosis (one), skin graft necrosis (one), dehisced stump (one), and gangrene of the tip of big toe (one), vascular graft thrombosis (one) and proximal graft occlusion (one).
Another cross sectional study done by Nielsen JV,28 showed that the prevalence of amputations below the ankle was of 3.4% (0.5-6).
Another prospective study,59 of diabetic patients with foot ulcers at Saudi Aramco Medical Services Organization included 62 patients from December 2003 to December 2004 with mean age of 64.8 + 12 years. During the study period, 19% (12 of 62) of the patients had amputations represented by 2 above-knee amputations, 3 below-knee amputations, and 7 limb-sparing surgeries. Most of the patients were having advanced ulcers before the amputation.
In another study done in Jordon,60 the researchers found that the overall prevalence of amputation was 5%.The rate of amputation was directly proportional to high HbA1c >8% (p = 0.01). Age and gender were not found to have an impact on prevalence of amputation.
An interesting international multi center study,61 established to enable a comparison of lower extremity amputation incidence rates between different centers around the world published in the British journal of surgery in 2000 showed the highest amputation rates was of 43.9 per 100,000 population per year for first major amputation in men and the lowest was 2.8 per 100,000 per year.
Interestingly, the multidisciplinary approach may decrease the rate of amputation significantly.62
ConclusionThe high prevalence of diabetes and the increasing prevalence of risk factors for diabetic foot as well as poor constructed education for preventing diabetic foot diseases stand behind the growing prevalence of diabetic foot lesions in Saudi Arabia.
Large community base surveys need to be conducted to assess the current situation and auditing the running programs.
Potential conflicts of interestThe author is not aware of any conflicts of interest related to the subject of the review.