The global prevalence of diabetes mellitus has reached epidemic proportions, and consequently the prevention and management of the disease is now a major public health challenge. This study aims to determine the prevalence of type 2 diabetes mellitus (T2DM) in the Basque Country, and identify new cases and the management of the disease based on data sourced from administrative databases.
MethodsRecords of all citizens living in the Basque Country aged ≥35 were reviewed and an algorithm was established to detect the presence of T2DM from registered diagnoses and prescriptions. Information from a four-year period was extracted detailing the demographic variables, requirements recommended by clinical practice guidelines, the level of management of the disease in accordance with local guidelines and the presence of ischemic heart disease.
ResultsIn 2011, there were 134,421 diagnosed cases of T2DM, representing a known prevalence of 9.12%. There were 8,896 new cases. The three main control criteria, glycosylated haemoglobin (HbA1c), LDL-cholesterol (LDLc) and blood pressure (BP), were met in 23.2% of people diagnosed with ischemic heart disease diagnosis and in 24.5% of people without a diagnosis of ischemic heart disease.
ConclusionsThe prevalence observed in the Basque Country is lower than that observed in Spain, and the achievement of targets for HbA1c, BP, and LDLc was slightly better, except the BP values, which were similar. The data recorded in this study could lead to the development of strategies to improve clinical care for patients with type 2 diabetes.
La prevalencia mundial de la diabetes mellitus tipo 2 (DM2) ha adquirido niveles de epidemia y su prevención y control se ha convertido en uno de los retos más importantes de salud pública. Este estudio tiene como finalidad determinar su prevalencia, nuevos casos y control en el País Vaco, a partir de bases de datos administrativas.
MétodosSe analizaron todos los registros de los ciudadanos del País Vasco con edad ≥35 años y se estableció un algoritmo para detectar la presencia de DM2 a partir de diagnósticos y prescripciones registrados. Se extrajo información relativa a un período de 4 años de variables demográficas, recomendaciones de las guías de práctica clínica, grado de control de la enfermedad de acuerdo con las guías locales y presencia de cardiopatía isquémica.
ResultadosEn 2011, 134.421 personas tenían DM2, es decir, una prevalencia conocida del 9,12%. Hubo 8.896 casos nuevos. Los criterios principales de control (hemoglobina glicosilada (HbA1c), colesterol LDL (LDLc) y presión arterial (PA)) se alcanzaron en el 23,15% de las personas con diagnóstico de cardiopatía isquémica y en el 24,54% de personas sin diagnóstico de cardiopatía isquémica.
ConclusionesLa prevalencia observada en el País Vasco es más baja que la observada en España, y el alcance de los objetivos para HbA1c, PA y LDLc fue ligeramente mejor excepto en la PA que fueron similares. Los datos registrados en este estudio podrían dar lugar al desarrollo de estrategias para mejorar la atención clínica de los pacientes con DM2.
From a clinical perspective, diabetes mellitus is a group of metabolic diseases characterised by chronic hyperglycemia secondary to an absolute or relative defect in insulin secretion and accompanied, to a greater or lesser extent, by lipid and protein metabolism disorders, leading to a number of chronic microvascular and macrovascular complications.
This chronic disease is now recognised as one of the most important health issues given its high prevalence and the impact on healthcare services and consequent economic impact.1 According to recent Spanish studies based on a population survey, the prevalence in Spain of type 2 diabetes (T2DM) is estimated at 13.8% (95% CI, 12.8–14.7) in individuals aged ≥18 years (of which 6% (95% CI, 5.4–6.7) had unknown T2DM),2 while the worldwide figure is 8.3%.3 Although, glycaemic control and management of cardiovascular risk factors (CVRFs) can reduce the incidence of diabetic complications, several studies have indicated that only 7–12% of patients with diabetes achieve optimum control of all CVRFs.4–6
In order to address the problem posed by the scale of T2DM, changes have had to be made to the structure and organisation of healthcare services to ensure a more efficient use of available resources, such as the effective coordination of all levels of care, implementation of multidisciplinary teams, self-care education and collaboration with diabetes patients’ associations.
In recent years, there has been consensus on the implementation of a multidisciplinary approach to the prevention of T2DM and the management of patients in primary care. Therefore, from 1993 until the present, the Spanish Group for the Study of Diabetes in Primary Healthcare (GEDAPS) has issued guidelines with the main recommendations for the diagnosis, management and treatment of diabetes. Additionally, the Spanish National Healthcare System (SNS) has developed strategic plans to address the disease,7 and Osakidetza-Basque Health Service has subsequently incorporated these recommendations into their own guidelines.8
Despite the scientific evidence available through international publications9,10 and the national guidelines,11 the management of these patients is still inadequate. Several observational studies conducted in Spain12–14 and in other countries15–17 have shown that there is a gap between recommendations and clinical practice.
Publications regarding population registers from other countries have highlighted the importance of this type of data.15,16,18–23 The digitalisation of healthcare systems and medical records has facilitated access to the data related to all patients with T2DM registered in the public healthcare system in the Basque Country. The analysis of these data provides an accurate reflection of the current management of type 2 diabetic patients in our region. Consequently, this study aims to determine the prevalence, incidence and the management of patients with type 2 diabetes in the Basque Country.
Materials and methodsEthics statementThe study protocol was approved by the Ethical Committee of Clinical Research of Euskadi (PI2014074). Informed consent was not obtained because patients’ healthcare records were anonymized and de-identified prior to analysis.
Study population and sources of informationThe study included all T2DM patients with public healthcare insurance in the Basque Country, regardless of whether or not they had visited healthcare services during the observation period (September 2007–August 2011). The Basque Country is one of the seventeen autonomous communities of Spain. These autonomous communities have the power to establish their own health plans and to organise their own health services. In Spain citizens have universal healthcare coverage, and each individual is assigned to a GP. This doctor acts as the gateway to the other healthcare departments and services.
As the records included in the administrative database and the electronic health records (EHR) are often incomplete or inadequately coded, the method for including patients with T2DM in the database in this study consisted of considering all those who, according to Osakidetza's sources (data on diagnoses, prescriptions and procedures, from people in outpatient care, in primary and specialised care and in emergency and hospital admissions), had been diagnosed with T2DM or unspecified diabetes mellitus (including complications) at any point in their life or who had been prescribed antidiabetic medication. Those patients who had been diagnosed at any point of contact with type 1 diabetes mellitus or for whom all diagnoses corresponded to unspecified diabetes mellitus, yet the only medication prescribed was insulin, were excluded from this group.
From the above sources and records and in line with the methodology described, the study population was identified, i.e. all those with T2DM in the Basque Country and aged 35 or over (this cut-off age was established on the grounds that type 2 diabetes is uncommon at younger ages). The four-year study period was divided into four periods: Year one – ending 31-08-2008; Year two – ending 31-08-2009; Year three – ending 31-08-2010; Year four – ending 31-08-2011. For each period, onset of T2DM in each individual was prior to the starting point of the period and the individual had to be active (Living Basque residents with public healthcare insurance) at the beginning of the period (though not necessarily for the whole year).
After filtering the database, 149,015 records were obtained of patients with T2DM at any time during the 4-year period.
Variables and analysisThe variables related to diabetes care were collected from digital medical records in primary care. For each of the four periods, the following data were recorded about the patients: age, gender, body mass index (BMI), systolic and diastolic blood pressure (SBP and DBP), smoking habits, flu vaccines, foot examination, glycosylated haemoglobin (HbA1c), serum cholesterol, microalbuminuria or albumin/creatinine ratio in a urine sample (nephropathy screening), fundus photography and cardiovascular risk (CVR). Since many people had more than one evaluation of these variables in each period, the last recorded evaluation in each period has been used.
The main aims of the study were to monitor the percentage of patients with T2DM who were annually evaluated (process indicators) in terms of the variables mentioned above, as well as those with values within the ranges recommended by the clinical practice guidelines (results indicators).
To assess the levels of control, we used the current objectives of the Diabetes Clinical Practice Guidelines (CPG) for the Basque Country: HbA1c ≤7%, BP ≤140/80mmHg and BMI <30kg/m2. In the present study, we used LDLc ≤100mg/dl for those with a previous diagnosis of ischemic heart disease and LDLc ≤130mg/dl for those without an ischemic heart disease diagnosis to compare with other consensus standards or CPG because the CPG of T2DM10 advocates using statins to treat LDLc in relation to patients’ CVR.
The known prevalence of T2DM was estimated, stratified by age and gender. The mean was calculated for all continuous variables. The value was always provided over the total number of patients, excluding those for whom values were missing.
Logistic regressions were used to see the effect of gender and age groups, in the dependent variables (BMI, HbA1c, LDLc and BP): the test has been performed and the patients have reached the CPG objectives (correctly controlled). Analyses were considered significant at p<0.05.
Statistical calculations were undertaken using Stata, Data Analysis and Statistical Software, Release 12 (StataCorp, LP, College Station, TX).
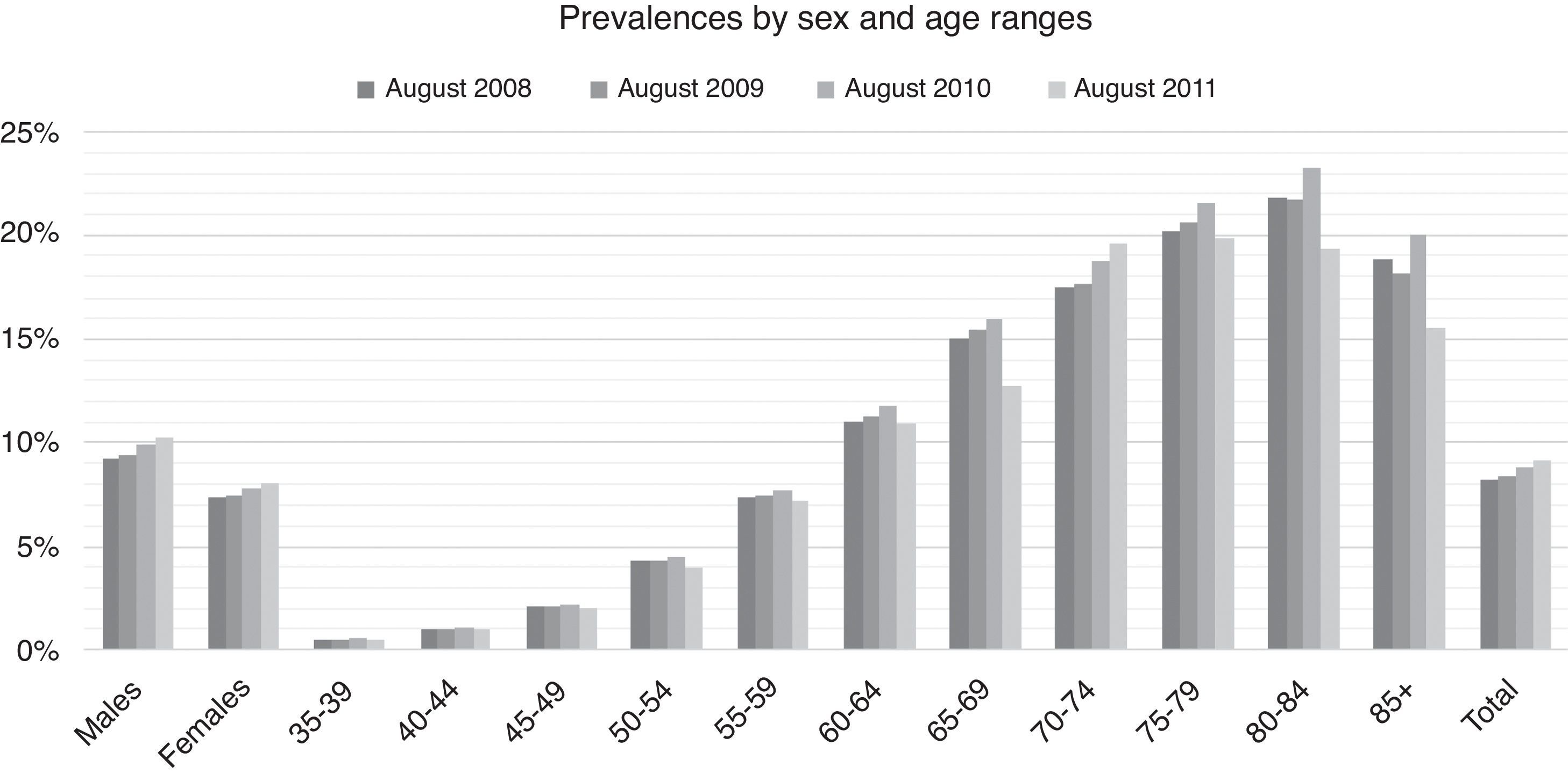
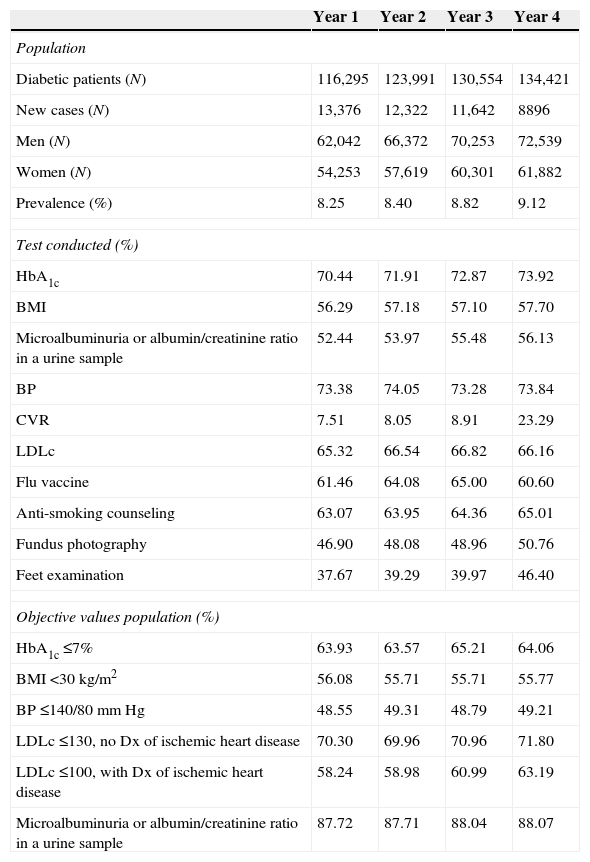
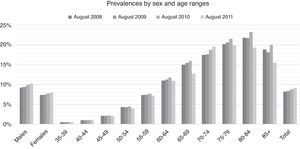
ResultsFrom 2007 to 2011The prevalence of T2DM over the four-year period increased from 8.25% in year 1 to 9.12% in year 4, reaching 8.40% in year 2 and 8.82% in year 3. The four-year period showed a higher prevalence in men (from 9.20% in year 1 to 10.28% in year 4). For women this prevalence grew from 7.38% in year 1 to 8.06% in year 4. The differences between gender were statistically significant in the four periods (p<0.001 for all periods). By age ranges, prevalence increased up to the age of 84 years and then decreased from the age of 85 onwards (see Fig. 1). It should be noted that although there was an increase in patients with T2DM between 2007 and 2011, there was a decrease in new diagnoses over the same period. Similarly, there was an increase in the number of screening tests for the disease as well as the values obtained by these patients, resulting in improved management of the disease. These data are compiled in Table 1.
Evolution of the tests performed and the objective values in patients with type 2 diabetes.
| Year 1 | Year 2 | Year 3 | Year 4 | |
|---|---|---|---|---|
| Population | ||||
| Diabetic patients (N) | 116,295 | 123,991 | 130,554 | 134,421 |
| New cases (N) | 13,376 | 12,322 | 11,642 | 8896 |
| Men (N) | 62,042 | 66,372 | 70,253 | 72,539 |
| Women (N) | 54,253 | 57,619 | 60,301 | 61,882 |
| Prevalence (%) | 8.25 | 8.40 | 8.82 | 9.12 |
| Test conducted (%) | ||||
| HbA1c | 70.44 | 71.91 | 72.87 | 73.92 |
| BMI | 56.29 | 57.18 | 57.10 | 57.70 |
| Microalbuminuria or albumin/creatinine ratio in a urine sample | 52.44 | 53.97 | 55.48 | 56.13 |
| BP | 73.38 | 74.05 | 73.28 | 73.84 |
| CVR | 7.51 | 8.05 | 8.91 | 23.29 |
| LDLc | 65.32 | 66.54 | 66.82 | 66.16 |
| Flu vaccine | 61.46 | 64.08 | 65.00 | 60.60 |
| Anti-smoking counseling | 63.07 | 63.95 | 64.36 | 65.01 |
| Fundus photography | 46.90 | 48.08 | 48.96 | 50.76 |
| Feet examination | 37.67 | 39.29 | 39.97 | 46.40 |
| Objective values population (%) | ||||
| HbA1c ≤7% | 63.93 | 63.57 | 65.21 | 64.06 |
| BMI <30kg/m2 | 56.08 | 55.71 | 55.71 | 55.77 |
| BP ≤140/80mmHg | 48.55 | 49.31 | 48.79 | 49.21 |
| LDLc ≤130, no Dx of ischemic heart disease | 70.30 | 69.96 | 70.96 | 71.80 |
| LDLc ≤100, with Dx of ischemic heart disease | 58.24 | 58.98 | 60.99 | 63.19 |
| Microalbuminuria or albumin/creatinine ratio in a urine sample | 87.72 | 87.71 | 88.04 | 88.07 |
N represents the total number of patients, (%) the percent of patients with Type 2 diabetes and Dx represents diagnosis.
In the first and last annual periods, 70.4% and 73.9% had at least one HbA1c value respectively; and of these, 63.9% and 64.1% met the target (≤7%) respectively. Some 73% in the first period and 74% in the last period had at least one BP evaluation. Of these patients, 49% (first period) and 63.9% (last period) had an SBP of ≤140mmHg and DBP of ≤90mmHg.
In the fourth year of the study, foot examinations, flu vaccinations and anti-smoking counseling were conducted with 46.40%, 60.60% and 65.01% of patients, respectively. Fundus photography was performed on 50.76% of patients either during this period, or in the two previous years, in line with the criteria established in the Basque Country for this type of screening (every 3 years).13 Nephropathy screening data were collected for 56.13% of the patients, where 88.07% of these patients achieved the target value.
The differences in the test conducted between year 1 and year 2 of study, year 2 and year 3, and year 3 and year 4 were statistically significant for nephropathy screening, BP, LDLc, feet examination, flu vaccine and fundus photography (all p<0.001). For BMI, we have found differences just between year 2 and year 3, and year 3 and year 4 (all p<0.001) and for RCV just between year 3 and year 4 (p<0.001) and finally, for HbA1c between year 1 and year 2 (p<0.001) and year 3 and year 4 (p=0.003).
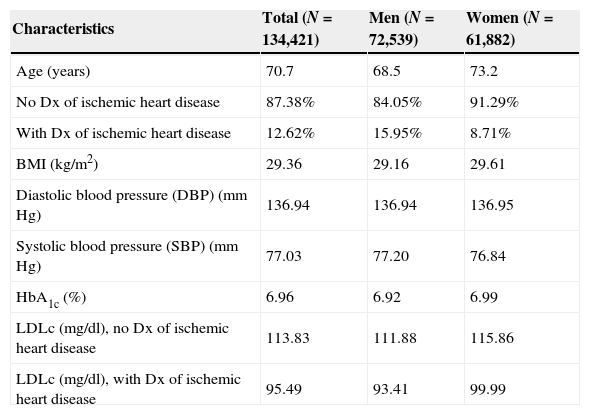
Situation in 2011The mean clinical and laboratory characteristics of the population in year 4 are summarised in Table 2. In the last annual period, from a total population of 1,473,943 people over 35 years of age, 134,421 people were diagnosed with T2DM, which represents a known prevalence of 9.12%. The mean age in this period was 70.7, 68.5 in males and 73.2 in females. Thirteen percent of these patients had ischemic heart disease. The mean of the HbA1c was 6.96 and the mean of BMI was 29.4. The mean concentration of LDLc was 113.83mg/dl for patients without ischemic heart disease and 71.8% of patients met the target of LDLc ≤130. For patients diagnosed with ischemic heart disease, the LDLc mean was 95.49mg/dl and 63.19% had LDLc values ≤100mg/dl. The mean values of BP control were 137/77mmHg on average and 49.21% of patients had SBP ≤140 and DBP ≤80mmHg.
Average of control variables for the population with type 2 diabetes in the fourth year of the study.
| Characteristics | Total (N=134,421) | Men (N=72,539) | Women (N=61,882) |
|---|---|---|---|
| Age (years) | 70.7 | 68.5 | 73.2 |
| No Dx of ischemic heart disease | 87.38% | 84.05% | 91.29% |
| With Dx of ischemic heart disease | 12.62% | 15.95% | 8.71% |
| BMI (kg/m2) | 29.36 | 29.16 | 29.61 |
| Diastolic blood pressure (DBP) (mmHg) | 136.94 | 136.94 | 136.95 |
| Systolic blood pressure (SBP) (mmHg) | 77.03 | 77.20 | 76.84 |
| HbA1c (%) | 6.96 | 6.92 | 6.99 |
| LDLc (mg/dl), no Dx of ischemic heart disease | 113.83 | 111.88 | 115.86 |
| LDLc (mg/dl), with Dx of ischemic heart disease | 95.49 | 93.41 | 99.99 |
Dx represents diagnosis.
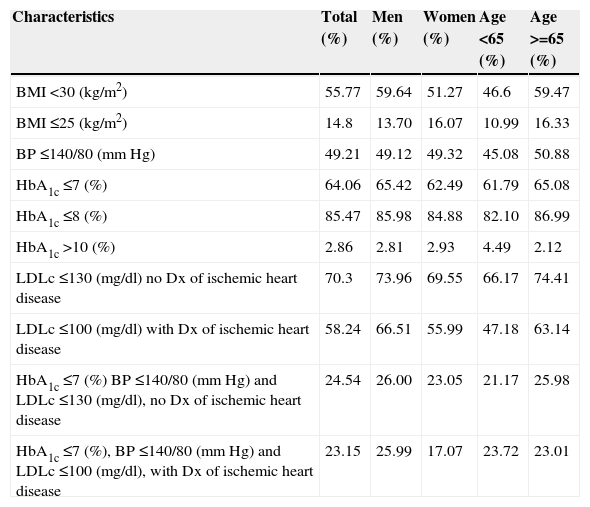
Control of the CVRF targets is outlined in Table 3. The complete data set for the three main control criteria (HbA1c, LDLc, and BP) was available for 72,539 (53.78%) patients, 63,402 in primary prevention and 8895 in secondary prevention. Of the patients without ischemic heart disease, only 24.54% had completed all control targets (HbA1c ≤7%, BP ≤140/80mmHg, and LDLc ≤130mg/dl), and it was almost the same proportion for the patients with ischemic heart disease (23.15% achieved target values) (HbA1c ≤7%, BP ≤140/80mmHg, and LDLc ≤100mg/dl). 55.77% obtained a value of BMI <30kg/m2 and only 14.8% values ≤25kg/m2.
Percentage (%) of population with diabetes type 2 who meet the objective values in the fourth year of the study.
| Characteristics | Total (%) | Men (%) | Women (%) | Age <65 (%) | Age >=65 (%) |
|---|---|---|---|---|---|
| BMI <30 (kg/m2) | 55.77 | 59.64 | 51.27 | 46.6 | 59.47 |
| BMI ≤25 (kg/m2) | 14.8 | 13.70 | 16.07 | 10.99 | 16.33 |
| BP ≤140/80 (mmHg) | 49.21 | 49.12 | 49.32 | 45.08 | 50.88 |
| HbA1c ≤7 (%) | 64.06 | 65.42 | 62.49 | 61.79 | 65.08 |
| HbA1c ≤8 (%) | 85.47 | 85.98 | 84.88 | 82.10 | 86.99 |
| HbA1c >10 (%) | 2.86 | 2.81 | 2.93 | 4.49 | 2.12 |
| LDLc ≤130 (mg/dl) no Dx of ischemic heart disease | 70.3 | 73.96 | 69.55 | 66.17 | 74.41 |
| LDLc ≤100 (mg/dl) with Dx of ischemic heart disease | 58.24 | 66.51 | 55.99 | 47.18 | 63.14 |
| HbA1c ≤7 (%) BP ≤140/80 (mmHg) and LDLc ≤130 (mg/dl), no Dx of ischemic heart disease | 24.54 | 26.00 | 23.05 | 21.17 | 25.98 |
| HbA1c ≤7 (%), BP ≤140/80 (mmHg) and LDLc ≤100 (mg/dl), with Dx of ischemic heart disease | 23.15 | 25.99 | 17.07 | 23.72 | 23.01 |
Dx represents diagnosis.
After the logistic regression analysis with data from year 4 (see additional material a), women were noted to be between 6% and 15% more likely than men to have the following tests: LDLc, HbA1c, BMI and BP. Age was also a significant factor regarding CVRF tests. The probability of having these tests increases up to the age of 69 for the HbA1c and LDLc assessment tests and up to 74 years of age for BMI and BP.
Men were more likely than women to meet target values for BMI, HbA1c and LDLc. Obesity was 25% more common in women than men. Gender was not significant in BP objective values. Also, women were 5% and 8% less likely to have good controls for HbA1c and LDLc, respectively. Age is also significant regarding good controls, the likelihood increases up to 69 years of age for HbA1c; up to 74 years of age for LDLc and BP and up to 79 years of age for BMI.
DiscussionAccording to the data observed in this study, management of T2DM has gradually improved and disease control tests have increased, as evidenced by process and outcome indicators. In the first year of study 2007–2008, the CVR assessment was carried out on 7.5% of patients with T2DM and four years later that figure reached 23.3%. Foot examinations also increased from 37.8% of individuals in 2007 to 46.4% of individuals in 2011.
In this study, the prevalence of this disease can be seen to increase annually, from 8.25% in September 2007 to 9.12% in September 2011. However, the prevalence observed in the Basque Country is lower than that observed in Spain24, where some data suggest that the prevalence in autonomous communities in the south of the country – such as Andalusia and the Canary Islands – is greater (13.3% and 12.4%, respectively). In recent years, several studies in Spain have analysed the characteristics and the level of management of patients with T2DM, although these studies are characterised by large differences in methodology and sampling4–6 and also differences in algorithms for criteria for the inclusion of population25,26, thereby making comparisons difficult.
Vinagre et al.14 conducted a cross-sectional study in primary health care centers in Catalonia (Spain) of a total population of 3,755,038 individuals aged 31–90 years at the end of 2009, where 286,791 patients (7.6%) had T2DM. All patients aged 31–90 years with a diagnosis of type 2 diabetes (International Classification of Diseases 10 [ICD-10] codes E11 and E14) before 1 July 2009 were included. Comparing with our results, they obtained means in Catalonia of: 137/76mmHg for BP, 113mg/dl for LDLc, 30kg/m2 for BMI and a prevalence of ischemic heart disease of 11% and our study returned a mean of 137/77mmHg for BP, 29kg/m2 for BMI and a prevalence of 13% of ischemic heart disease.
Considering the mean, the degree of control of HbA1c had a value of 6.96% in 2011, which is comparable to other studies carried out by Vinagre et al.,14 Saaddine et al.19 and Club Sicilia,21 which found values of 7.1%, 7.7% and 7.3% respectively.
The strength of our study is that it includes all patients with T2DM sourced from an administrative population database which contains almost 100% of the population of the Basque Country over 34 years of age, for each period. Furthermore, it is a study using data from 149,015 patients with T2DM, over four years and with four cross sections and a known prevalence of 9.12% in 2011, reaching 20% at ages over or equal to 75. The representativeness of the sample from a universal and public healthcare system, the good quality of records and the systematic recording by Osakidetza's healthcare personnel have enabled the construction of this reference database to be ideal for monitoring risk factors as well as the management and prevalence of T2DM in our region.
The data recorded in the last cross section, namely HbA1c, BMI, LDLc and compliance with the optimal values of HbA1c, BP, and LDLc were slightly better than previously published data in other Spanish studies14 except for BP values, which were similar. However, in both studies, the values reported were better in males compared to females; also, the population of 65 years of age or over has better control of the disease than younger patients.
Our study had certain limitations. The administrative databases only contain information about the problems for which people seek medical attention. Therefore, the prevalence of diabetes can only reflect known cases and excludes the presence of cases that are unknown to patients or their doctors. Another limitation in the study was the lack of data for some variables that were not properly recorded by healthcare professionals. Although the data are consistent with previous findings, there is still a risk of bias in the results of this study, as an under-diagnosis and underreporting of data for T2DM or other associated conditions could have occurred. Finally, calculation of the progression time of the disease was not possible as our healthcare system began to digitalise medical records in 1998. Therefore, if a patient was diagnosed before 1998, we could not obtain the initial date of diagnosis.
ConclusionsThe results of this study are, to some extent, similar and comparable to those of previous publications in Spain and elsewhere. The availability of the data on clinical practice at primary care level may have important implications for diabetes care. The information obtained should allow current clinical practice to be evaluated based on the results of the process and the outcome of diabetes treatment. These results could be explained by early detection and appropriate treatment provided by primary care practitioners, and the support by the management system whose objectives are compatible with clinical practice guidelines.
Furthermore, this study may serve for the future development of a specific diabetes register in the Basque Country. The information provided is organised, accessible and timely to develop appropriate indicators to epidemiological surveillance and monitoring of diabetes and its complications.
To reduce the burden of this disease, health policies should be implemented toward promoting the optimal management of this condition and associated CVRF, as well as public health interventions that address their determinants.
FundingThe funding organisation, Sanofi, had no role in the design and conduct of the study, the collection, management, analysis and interpretation of data, or the preparation, review and approval of the manuscript.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that they have followed the protocols of their work center on the publication of patient data.
Right to privacy and informed consentThe authors declare that no patient data appear in this article.
Conflict of interestThe authors declare no conflict of interest.
The authors wish to acknowledge the support received from Ricardo Samper Ochotorena as well as the funding collaboration and support received by Sanofi, in connection with increasing diabetes awareness.