Acrodermatitis enteropathica is a low-incidence disease due to inherited or acquired zinc deficiency. It is characterized by acral dermatitis, alopecia, diarrhea and growth retardation. The dermatological condition may mimic a cutaneous fungal infection or other pathogen-related skin diseases.
Case reportWe report the case of a female patient of 7 months of age, who was sent to Centro Médico Nacional 20 de Noviembre for suspicion of immunodeficiency and cutaneous mycosis. Her condition began with dermatosis disseminated to the head, trunk and genital region; initial treatment with antifungal and broad spectrum antibiotics was given, without improvement. Upon admission, immunodeficiency and fungal infection were discarded. Acrodermatitis enteropathica was suspected, and corroborated later by low serum zinc levels. Immediately after the start of oral treatment with zinc, the patient showed improvement.
ConclusionsThere are multiple differential diagnoses of acrodermatitis enteropathica, which includes cutaneous infections. Therefore, the early recognition of the characteristic lesions favors suspicion, diagnosis and appropriate treatment.
La acrodermatitis enteropática es una enfermedad de baja incidencia que ocurre por deficiencia de zinc; puede ser hereditaria o adquirida. Se caracteriza por dermatitis acral, alopecia, diarrea y problemas de crecimiento. La afección dermatológica puede simular una infección micótica cutánea u otras enfermedades de la piel relacionadas con patógenos.
Caso clínicoSe informa el caso de una paciente de sexo femenino de 7 meses de edad, que fue enviada al Centro Médico Nacional 20 de Noviembre por sospecha de inmunodeficiencia y micosis cutánea. Inició con un cuadro clínico caracterizado por dermatosis diseminada a cabeza, tronco y región genital, por lo que recibió tratamiento inicial con un antifúngico y antibióticos de amplio espectro, sin presentar mejoría. A su ingreso se descartaron inmunodeficiencia e infección micótica. Se sospechó acrodermatitis enteropática, corroborándose el diagnóstico al encontrar niveles séricos de zinc disminuidos. La paciente presentó mejoría inmediata tras el inicio del tratamiento con zinc por vía oral.
ConclusionesEl diagnóstico diferencial de acrodermatitis enteropática es amplio e incluye infecciones cutáneas, por lo que el reconocimiento temprano de las características de las lesiones favorece la sospecha, el diagnóstico y el tratamiento adecuado.
Zinc is an essential trace element that fulfills multiple metabolic functions: it participates actively in the catalytic site of an important number of enzyme systems. Zinc is a structural ion which participates in certain biological membranes, and it is necessary for histone integrity. It is also a component of the DNA and RNA polymerases and of cytosolic enzymes involved in protein synthesis, for which it plays a central role in cell growth.1,2 Therefore, it is necessary for the proper functioning of various organs and systems, including the gastrointestinal tract, central nervous system, and integumentary system.
Zinc deficiency can be caused by different factors, such as inadequate intake, intestinal absorption problems or excessively high body weight losses, and certain specific diseases. Acrodermatitis enteropathica (AE) is the most representative zinc deficiency pathology resulting from a defect in the intestinal absorption or an inadequate supply.3
The case of an infant with AE is presented. AE diagnosis, although rare, is of great clinical relevance, and should be recognized promptly by primary care physicians for a timely treatment, lesions progression control, and complications prevention.
2Clinical caseA 6-month-old female infant from Sinaloa, Mexico, with young non-consanguineous parents. Born at term from a normoevolutive pregnancy by cesarean, without complications. She was exclusively breastfed until the third week of life. She underwent pyloric hypertrophy, for which a pyloromyotomy was performed. Subsequently, she was fed with starter formula. However, she presented allergy to cow's milk protein; thus, she was treated with an extensively hydrolyzed formula. As no improvement was seen, the formula was changed to an amino acid one. Among her medical history, the mother reported two episodes of pneumonia requiring hospitalization and recurrent gastrointestinal infection.
At five months of age, she presented dermatosis disseminated to the head, neck, trunk, and genitalia, consisting of erythemato-squamous pink-red plaques, shiny, regular and well defined edges of one week of evolution. Also, she presented fever and general malaise and was admitted to the Pediatrics service in the Regional Hospital. During her stay, Acinetobacter baumannii and Klebsiella pneumonia were isolated from peripheral blood cultures. The patient received treatment with ceftriaxone, vancomycin, and caspofungin in addition to the administration of intravenous immunoglobulin for suspected immunodeficiency; no improvement in the skin lesions was observed. Consequently, she was referred to this unit with the diagnosis of cutaneous mycosis.
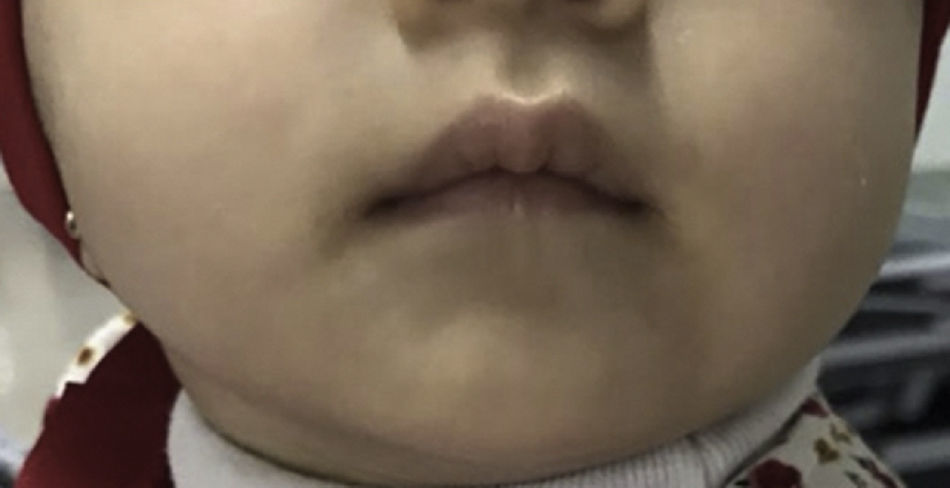
At admission, she weighed 6.3kg (p12.86, -1.13 SD), size 65cm (p45.96, -0.10 SD). Upon physical examination, disseminated dermatosis was observed on the head and trunk with symmetrical distribution, affecting upper eyelids, postero-superior aspect of auricular pavilions, perioral region, chin, anterior face of the neck, and antero-superior aspect of the trunk. The dermatosis consisted of pink-red erythemato-squamous plaques of bright appearance, regular and well defined edges, with fine white-on-the-surface scale and thicker towards the edges, easily removable, of two-week evolution. Glossitis and angular cheilitis were found in mucous membranes (Figure 1). The rest of the physical examination was normal.
Antibiotics and antifungals were suspended and total parenteral nutrition (TPN) was indicated because of the poor oral tolerance secondary to the described lesions. In the immunological evaluation, immunodeficiency was ruled out. Dermatology initiated topical emollients and performed a skin biopsy, which reported mild vasculitis with polymorphonuclear and eosinophilic infiltrates. Skin culture showed no fungal or bacterial development.
AE was suspected due to the clinical presentation. Therefore, serum zinc levels were determined. The report showed 54.07μg/dl, which confirmed the diagnosis. She started treatment with zinc gluconate orally at a dose of 15mg every 24hours. There was an immediate improvement of the skin lesions, observing disseminated dermatosis in the same topography, constituted by pink plaques, with regular and well-defined edges, symmetrical, with thin and easily detachable scales (Figure 2). TPN was suspended since oral tolerance was improved. During her stay, she remained without fever and blood cultures were reported with any growth. Acute phase reactants were negative, for which she was discharged alongside oral treatment with zinc gluconate in the same dose. Three months later, she was seen at the outpatient clinic finding a total resolution of the dermal lesions (Figure 3), asymptomatic, and without other pathological findings in the physical examination.
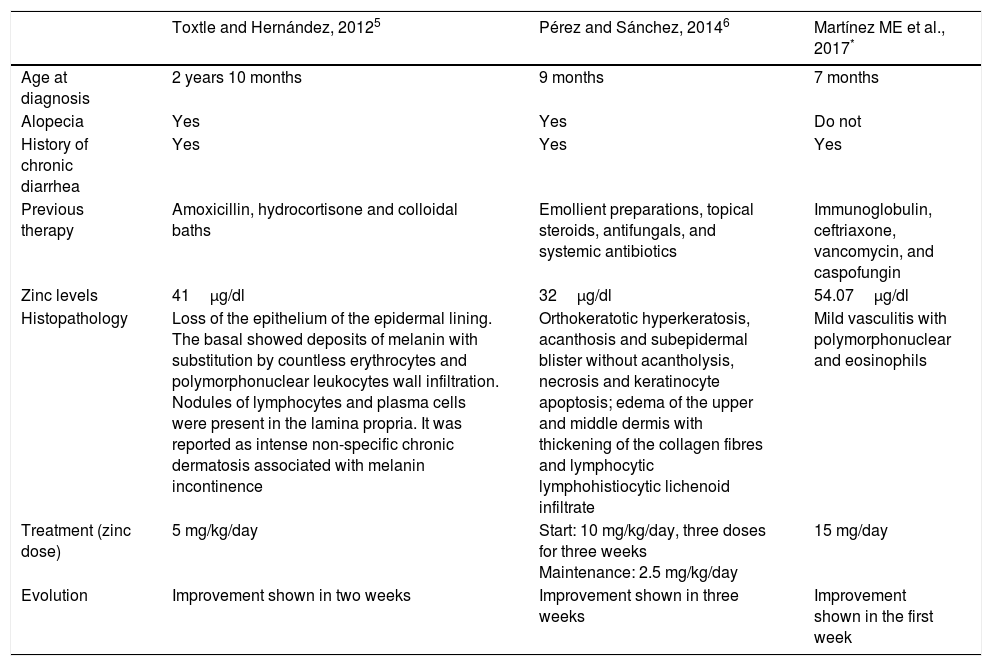
AE is a disease secondary to zinc deficiency, with an estimated incidence of 1:500,000 newborns, without preference for race or sex.4 In Mexico, two cases of AE have been reported earlier (Table 1).5,6
Case reports of patients with acrodermatitis enteropathica.
| Toxtle and Hernández, 20125 | Pérez and Sánchez, 20146 | Martínez ME et al., 2017* | |
|---|---|---|---|
| Age at diagnosis | 2 years 10 months | 9 months | 7 months |
| Alopecia | Yes | Yes | Do not |
| History of chronic diarrhea | Yes | Yes | Yes |
| Previous therapy | Amoxicillin, hydrocortisone and colloidal baths | Emollient preparations, topical steroids, antifungals, and systemic antibiotics | Immunoglobulin, ceftriaxone, vancomycin, and caspofungin |
| Zinc levels | 41μg/dl | 32μg/dl | 54.07μg/dl |
| Histopathology | Loss of the epithelium of the epidermal lining. The basal showed deposits of melanin with substitution by countless erythrocytes and polymorphonuclear leukocytes wall infiltration. Nodules of lymphocytes and plasma cells were present in the lamina propria. It was reported as intense non-specific chronic dermatosis associated with melanin incontinence | Orthokeratotic hyperkeratosis, acanthosis and subepidermal blister without acantholysis, necrosis and keratinocyte apoptosis; edema of the upper and middle dermis with thickening of the collagen fibres and lymphocytic lymphohistiocytic lichenoid infiltrate | Mild vasculitis with polymorphonuclear and eosinophils |
| Treatment (zinc dose) | 5 mg/kg/day | Start: 10 mg/kg/day, three doses for three weeks Maintenance: 2.5 mg/kg/day | 15 mg/day |
| Evolution | Improvement shown in two weeks | Improvement shown in three weeks | Improvement shown in the first week |
Zinc deficiency can occur because of genetically or acquired causes. The hereditary form corresponds to an autosomal recessive genetic defect, where a mutation in the SLC39A4 gene, located on chromosome 8q24.3 which encodes ZIP4, a transport protein exists, resulting in a deteriorated absorption of zinc and a subsequent deficiency. Up to now, 34 variants that affect the function of SLC39A4 have been described.4,7,8 The acquired form is associated with other entities such as malabsorption syndromes, inflammatory bowel disease, chronic pancreatitis, short bowel, celiac disease, cystic fibrosis or prolonged parenteral nutrition. Patients with malignant neoplasms, burns, and infections may have zinc deficiency due to an increase in the metabolic demand. Some drugs such as penicillin, diuretics, valproate, antimetabolites and iron can also produce a deficiency of this mineral.3
AE symptoms may appear on infants fed with formula during the first days after stopping breastfeeding. This indicates that human milk is a protector factor. Although cow's milk contains a greater amount of zinc than human milk, it lacks other low molecular weight proteins that are necessary for its absorption and bioavailability.9 This patient stopped breastfeeding by the third week of life, which may have contributed to the development of the disease.
Early symptoms of AE include the appearance of erythematous plaques, dry and scaly skin, and eczema. Usually, the initially affected areas are acral skin, periorificial, face, scalp and genitalia. This cutaneous dermatitis deteriorates rapidly and may be accompanied by paronychia, inflammatory dermatitis on the palms, and wrinkles on the fingers. There may be affection to the mucous membranes, mainly with glossitis, stomatitis and angular cheilitis.10 As described in the literature, this patient presented skin involvement of the ears, eyelids and mouth, with mucosal involvement manifested by glossitis and angular cheilitis. Similarly, she presented lesions in the neck, trunk, and perineal area.
Diarrhea is one of the most variable symptoms of AE. If it occurs and is exacerbated, it could lead to an electrolyte imbalance.9 In the clinical history of this patient, multiple gastrointestinal infections characterized by no blood diarrhea where mentioned. This symptom is a crucial figure for the diagnosis of AE. Therefore, it should be explored thoroughly questioning when zinc deficiency is suspected.
The initial suspicion of primary immune deficiency in this patient was based on the history of two hospitalizations for community-acquired pneumonia. However, it must be considered that zinc deficiency affects multiple aspects of the immune system, primarily its development and function of cells that mediate innate and adaptive immunity. Phagocytosis, intracellular death, and cytokine production are also affected by zinc deficiency.11
The diagnosis is mainly clinical supported by laboratory tests by measuring serum zinc levels. Normal zinc levels in the general population are 70-110μg/dl.9 In Latin American children, from 82-280μg/dl.12 Molecular genetic tests can identify a mutation in the SLC39A4 gene, confirming AE genetic diagnosis.
The differential diagnosis includes contagious impetigo, candidiasis, psoriasis, and other skin diseases related to pathogens. The reference diagnosis of this patient was a cutaneous mycosis. The presentation form of this entity are rounded, well-defined macules, with easily removable fine scales on their surface. Color varies from pink, orange, and white, with lesions that are distributed through the thorax, shoulders, arms, abdomen, lumbar region and neck, and are infrequent in the lower extremities and face.13 Skin mycosis was discarded since these characteristics were not observed in the patient. Other differential diagnoses are seborrheic dermatitis, Stevens-Johnson syndrome, atopic dermatitis, and erythema multiforme.
The lesions of AE do not show specific histopathological characteristics. In this patient, vasculitis was reported, which has not been described earlier for this disease.
Zinc supplementation is the basis for the treatment of AE. The recommended dose is 1-2mg/kg/day. Zinc acetate, zinc gluconate, and zinc sulfate are some examples of available zinc supplements that may be effective in the treatment of AE. In severe cases of zinc deficiency, intravenous administration of 10-20mg of zinc chloride is recommended. Some symptoms improve even before the normalization of serum zinc level. Diarrhea usually stops within 24hours, skin lesions begin to improve within the first 24hours, and severe skin infections are cured in a week.9 In the presented case improvement was observed following the zinc gluconate treatment with remission of lesions after one week of administration.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that they have followed the protocols of their work center on the publication of patient data.
Right to privacy and informed consentThe authors have obtained the written informed consent of the patients or subjects mentioned in the article. The corresponding author is in possession of this document.
FundingNone.
Conflict of interestThe authors declare no conflicts of interest of any nature.
Please cite this article as: Martínez-Bustamante ME, Peña-Vélez R, Almanza-Miranda E, Aceves-Barrios CA, Vargas-Pastrana T, Morayta-Ramírez Corona ARR. Acrodermatitis enteropática. Bol Med Hosp Infant Mex. 2017;74:295–300.