Acute colonic pseudo-obstruction, also known as Ogilvie syndrome, is a rare gastrointestinal syndrome in children. It is characterized by a marked dilatation of the colon evidenced by imaging and absence of mechanical obstruction. Patients typically present abdominal pain and distention, tympanic abdomen with peristalsis accompanied by nausea and vomiting. Up to 40% of patients can pass gas and have bowel movements. This syndrome is very rare in pediatric patients, and no cases have been reported in a post-renal transplant pediatric patient.
Case reportA 13-year-old male patient with a medical history of psychomotor retardation due to perinatal asphyxia and chronic renal failure secondary to bilateral renal hypoplasia was treated with peritoneal dialysis for one year until kidney transplantation. Currently, he is under immunosuppressive regimen. His condition began with mild abdominal pain accompanied by semi-liquid stools, and progressive distention up to 78cm of abdominal circumference in 72hours. Image studies were performed. Managed with prokinetic drugs without any improvement. Two exploratory laparotomies observed flanges, without evidence of any mechanical obstruction. An abdominal magnetic resonance was performed, where important intestinal dilatation was observed and no evidence of mechanical obstruction. Ogilvie's syndrome was diagnosed, and management with neostigmine was initiated, which led to symptom resolution.
ConclusionsThis syndrome is very rare in children. Therefore, there is little clinical suspicion and lack of management guidelines for diagnosis and treatment of patients of this age.
La pseudo-obstrucción colónica aguda, conocida también como síndrome de Ogilvie, es una condición gastrointestinal poco frecuente en pediatría. Se caracteriza por una marcada dilatación del colon en estudios de imagen y ausencia de obstrucción mecánica. Los pacientes se presentan clásicamente con dolor abdominal y abdomen distendido, timpánico, con peristalsis presente, acompañado de náusea y vómito. Hasta el 40% de los pacientes canalizan gases o evacúan. Este caso se reporta debido a lo raro que es este síndrome en pacientes infantiles y a que no hay casos reportados en un paciente pediátrico post trasplante renal.
Caso clínicoPaciente masculino de 13 años de edad con antecedente de retraso psicomotor posterior a asfixia perinatal e insuficiencia renal crónica secundaria a hipoplasia renal bilateral. Fue tratado mediante diálisis peritoneal durante un año hasta la realización del trasplante renal. Se encuentra en manejo con inmunosupresores. Inició su padecimiento actual al presentar dolor abdominal leve acompañado de evacuaciones semilíquidas, posteriormente presentó distensión abdominal progresiva de hasta 78cm de perímetro abdominal, por lo que se realizaron estudios de imagen. Se prescribieron medicamentos procinéticos, sin mejoría. Se realizaron dos laparotomías exploratorias en las que se observaron bridas, sin datos de obstrucción mecánica. Se realizó una resonancia magnética abdominal, encontrándose importante dilatación intestinal. Se diagnosticó síndrome de Ogilvie y se administró neostigmina, presentando resolución del cuadro clínico.
ConclusionesEste es un síndrome muy raro en la edad pediátrica, por lo que hay poca sospecha clínica y no existen guías de manejo para el diagnóstico y tratamiento en pacientes infantiles.
Acute colonic pseudo-obstruction, also known as Ogilvie's syndrome for being described by Ogilvie in 1948,1 is a gastrointestinal disorder characterized by a marked dilatation of the colon without a mechanical obstruction.2 Patients present classically with pain and abdominal distention, abdominal tympanic percussion with a conserved peristalsis, accompanied by nausea and vomit. Up to 40% of the patients pass gas or evacuate. In imaging studies, a dilatation of the colon without any signs of a mechanical obstruction can be observed.1
The mechanism by which this syndrome occurs is still unknown. The prevalent theory is that it is secondary to an imbalance of the autonomic innervation of the intestine, resulting in colonic atony.2
Colonic pseudo-obstruction is a diagnosis of exclusion. Among the differential diagnosis, fecal impaction, colonic or rectal tumors, sigmoid or cecal volvulus and toxic megacolon should be considered.3
The initial treatment includes bowel rest, intravenous fluids, electrolyte imbalance correction, stopping the administration of drugs that affect intestinal motility and decompression with a nasogastric tube.1 More aggressive treatments are necessary when no improvement with these measures is observed. The next step is using neostigmine, a reversible acetylcholinesterase inhibitor that augments intestinal muscle contractility.2 If this fails, a decompression by colonoscopy is performed, with a 70% rate of success, which requires a colonic decompression tube placement.2 Finally, if previous treatments are not effective, a cecostomy is performed, which should be carried out initially if any signs of ischemia, abdominal sepsis or perforation are present.4
Due to the rarity of this syndrome in pediatric patients and given that there are no reported cases of a pediatric post renal transplant, this case is important to the knowledge of this disease, to create management and treatment guidelines in pediatric patients.
2Clinical caseA 13-year-old male patient, without any relevant family history, with a perinatal history of a twin pregnancy, which was delivered by a cesarean section and that required advanced reanimation maneuvers presented with altered psychomotor development due to perinatal asphyxia, for which he receives neurodevelopmental therapy since the age of two years. At 11 years of age, he was diagnosed with chronic kidney disease caused by bilateral renal hypoplasia, which was treated with peritoneal dialysis until the age of 12 years. A renal transplant was performed, with a right iliac fossa placement, keeping both hypoplastic kidneys with an immunosuppression treatment that included tacrolimus, prednisone, azathioprine and mycophenolate sodium, and chronic medication with ketoconazole, iron supplementation, trimethoprim/sulfamethoxazole. The present illness started three weeks before his admission, with intermittent mild abdominal pain of a burning quality localized to the epigastrium and irradiation to the mesogastrium. No triggering or attenuating phenomena was present; accompanied by three to four stool depositions a day, with loose, semi-liquid stools of a greenish color, without any mucous or blood, and non-fetid. The pain became progressive, up until 24hours before his admission, when it changed to moderate intensity, and incapacitating the patient, for which he attended the emergency unit. Clinical examination revealed a globose abdomen, with a right flank scar, depressible, with tenderness on deep palpation in the epigastrium and mesogastrium. Without any signs of an acute abdomen, tympanic to percussion, with a conserved peristalsis in the four quadrants. He was admitted to the hospital and pantoprazole was added to his chronic baseline treatment, and trimethoprim/sulfamethoxazole, iron supplementation and mycophenolate sodium were suspended.
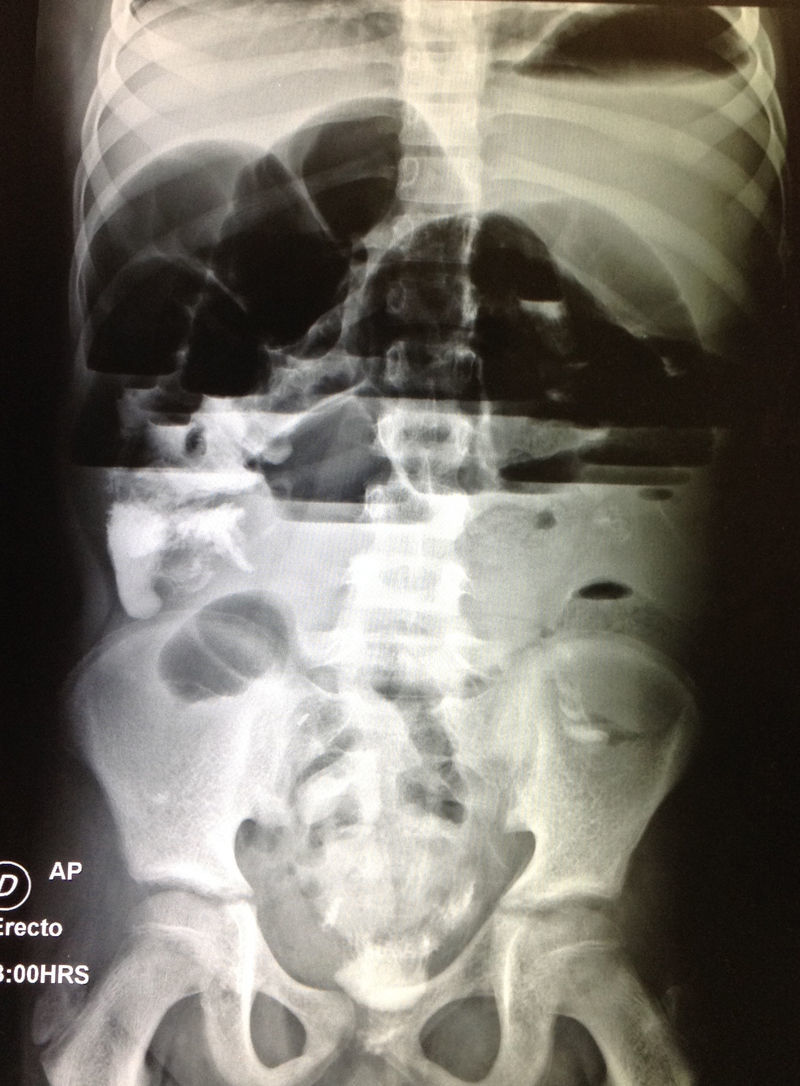
Complete blood count revealed anemia with a hemoglobin of 10.8g/dl, leukopenia of 1.6/μl and neutropenia of 0.54/μl, secondary to chronic kidney disease and immunosuppression. Urinalysis was normal. Results of the biochemical profile showed creatinine: 0.9mg/dl (estimated glomerular filtration rate: 107.3ml/min/1.73m2, which was within normal range), blood urea nitrogen: 20mg/dl, urea: 42.8mg/dl, total calcium: 8.9mg/l, phosphate 3.3mg/dl, albumin 3.4g/dl, GOT (AST): 11 U/l, GPT (ALT): 8 U/l, alkaline phosphatase: 98 U/l, lactate dehydrogenase: 297 U/l, sodium: 132.2 mEq/l, potassium: 3.63 mEq/l, chloride: 100.9 mEq/l. Tacrolimus levels of 5.6 ng/ml (normal dose within six months of the kidney transplant of 5 ng/ml). A contrast-enhanced abdominal tomography was performed, where only dilated intestinal loops and a kidney graft in a good state were observed. A gastrointestinal transit was performed, which did not show any signs of obstruction. During the first days of in-hospital stay, the pain was managed with butylhyoscine. However, abdominal distention progressively increased. Thus, a plain abdominal film was ordered, which showed air-fluid levels and intestinal distention (Fig. 1). A consultation with the adult surgery service was requested, which team was the same that participated in this patient's transplant, and they placed a nasogastric tube, which drained a fecaloid material. The patient was kept in observation with radiographic follow-up; nevertheless, he continued with pain and progressive abdominal distention of up to 78cm of the abdominal perimeter. An exploratory laparotomy was performed. This study revealed the presence of adhesions predominating at the level of the jejunum and ileum and a Meckel's diverticulum, which was resected and an anastomosis was performed. After surgery, the patient had hemodynamic instability and was transferred to the pediatric intensive care unit.
In the intensive care unit, the patient was stabilized, although he continued with abdominal distention, which raised the suspicion of post-operatory ileus. As the days went by and despite management with trimebutine, the pain and abdominal distention persisted without improvement. Therefore, the intestinal obstruction was suspected again. A second exploratory laparotomy was performed, in which adhesions and flanges were observed, without any signs of mechanical obstruction.
After surgery, the patient was kept under surveillance for several days, where he continued with abdominal distention despite management with erythromycin, cinitapride, amoxicillin/clavulanate, without clinical or radiological improvement. A magnetic resonance enterography was performed in which an important dilatation of the small and large intestine was observed, with abundant fluid within, without any signs of mechanical obstruction (Fig. 2). A consultation with pediatric gastroenterology was solicited, who suspected an acute colonic pseudo-obstruction, for which 1.5mg of neostigmine was administered, which decreased abdominal distention. Finally, an acute colonic pseudo-obstruction was diagnosed, for which two more doses of 1.5mg of neostigmine were administered. During his hospital stay, the patient presented clinical improvement, with a progressive decrease in abdominal distention and symptoms, as well as a progressive improvement of oral intake. The patient was discharged in a good clinical state.
3DiscussionOgilvie's syndrome is a very uncommon disorder in pediatrics;2 it occurs in adult patients with severe cardiac, neurologic and respiratory diseases, as well as renal insufficiency, hypothyroidism, and disseminated cancer or surgical conditions.1 Trauma patients with electrolyte disorders, sepsis,2 and post-renal transplant4 are also predisposed. Several medications have been related to Ogilvie's syndrome, among which vincristine,1 opioids,2 mycophenolate,5 steroids,4 calcium channel blockers3 and anticholinergics, such as butylhyoscine3 have been described.
This patient has a history of renal transplantation and having received drugs such as mycophenolate and prednisone as risk factors.4,5 Despite the administration of butylhyoscine during his hospital stay and the patient presenting with septic shock, the cause for the initial hospital admission is believed to be the acute colonic pseudo-obstruction syndrome and not a consequence of the administration of this medication. Besides, the patient was being treated with drugs that alter electrolytes, such as prednisone, which causes hypokalemia6 and trimethoprim/sulfamethoxazole, which can cause hypercalcemia.7 However, the patient did not present abnormalities in potassium levels. Trimebutine (spasmolytic) was also prescribed to the patient due to the antiserotoninergic activity, but there are no reports in the literature which associate this drug to acute colonic pseudo-obstruction.
Ogilvie's syndrome in post-renal transplant adult patients is well documented. In a retrospective study of 550 renal-transplant patients, seven developed the syndrome acutely, and the literature showed that 78 patients developed the syndrome post-transplantation.3 Nevertheless, there are no reports of Ogilvie's syndrome in post-transplant pediatric patients. In adults, a tendency for an increased incidence in patients with chronic kidney disease has been observed due to certain factors such as aluminum antacid ingestion, inactivity, dehydration, electrolyte disorders and the use of high steroids doses.8 Other important risk factors include obesity (>30kg/m2) and the use of narcotics as analgesics4 and the previously mentioned immunosuppression.
Among the complications of Ogilvie's syndrome, intestinal ischemia and subsequent spontaneous perforation (3-15%), peritonitis and a high associated mortality (> 50%) are encountered.1 In immunosuppressed patients subjected to a renal transplant, mortality ranges between 60-100%.5 In children, mortality is not defined due to the low incidence of the syndrome in the pediatric age and the age-related variability in the size of the colon.5 In this case, two exploratory laparotomies were performed, which were justified by the apparent signs of obstruction and acute abdominal distention. Nevertheless, during surgery, flanges were observed without any signs of occlusion. Moreover, despite adhesiolysis, the patient's symptoms persisted. Imaging studies, including magnetic resonance and intestinal transit, did not reveal signs of obstruction either. After the laparotomies, a postoperative ileus was suspected. Nevertheless, the days after surgery, the patient had normal peristalsis and evacuations,9 and, given the lack of response to medical treatment with prokinetics such as clavulanate, erythromycin or cinitapride, a diagnosis of postoperative ileus was discarded. On the other hand, patients who suffer Ogilvie's syndrome present with abdominal distention with a normal peristalsis and 40% of the cases present with normal evacuations. These data, additionally to an imaging study which showed a significant abdominal dilatation without any signs of obstruction, along with clinical resolution of the illness with neostigmine, confirmed Ogilvie's syndrome as the final diagnosis.1
Neostigmine is a parasympathomimetic reversible acetylcholinesterase inhibitor, which is believed to increase colonic contractility by stimulating the parasympathetic nervous system.2 It has been well-tolerated, and the typical adverse effects include abdominal pain, increased salivation, vomit, and diaphoresis. In some cases, patients can present symptomatic bradycardia that may require atropine, or bronchospasm, for which a cardiorespiratory surveillance may be necessary, with vital signs and electrocardiogram up to 30minutes after drug infusion.1 Several contraindications to neostigmine include mechanical obstruction, evidence of ischemia or intestinal perforation, pregnancy, cardiac arrhythmias, severe bronchospasm, or renal insufficiency.1 Hence, the importance of ruling out any signs of obstruction with an MRI, and checking that the transplanted kidney is functioning adequately. In pediatric patients, the use of 0.1mg of neostigmine has been described, with increases of up to 0.05mg every 20minutes, until gastrointestinal motility recovery and a decrease of the abdominal distention or up to a maximum dose of 0.05mg/kg2. In this patient, the maximal dose was nearly administered, 0.04mg/kg, requiring three doses, which resulted in an obvious improvement both clinically and radiologically (Fig. 3), which was progressive so finally his discharge was decided.
In the management of Ogilvie's syndrome, neostigmine has evidence of efficacy from multiple studies. In a 10-year retrospective study in adults, this medication showed an efficacy of 60-94% with an 11% of recurrence. Colonoscopic decompression has shown a better efficacy of > 90% and a recurrence of 11%.10 Nevertheless, this is not the first choice procedure, given the high risk of complications (1-5%), with colon perforation being the most serious.2 For that reason, in this patient that had many risk factors for a complication, combined with the high mortality related to having a colonic perforation, treatment with neostigmine was started, having a good response, without the need of colonoscopic decompression.
Given that Ogilvie's syndrome is infrequent, especially in pediatric patients, there is little clinical suspicion. Furthermore, an increased risk of multiple surgical procedures often unnecessary, or other failed treatments, long hospital stays, or in the worst case, complications of the disease such as ischemia, peritonitis or intestinal perforation, can be catastrophic in a transplanted patient with immunosuppression. Unlike adult patients, in which there is more information about this syndrome, in the pediatric age group, there is a need of clinical guidelines for the diagnosis and treatment. Hence, the importance of reporting this case, since it is necessary to keep it in mind as a differential diagnosis, always striving for the benefit of the patient.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that no patient data appear in this article.
Right to privacy and informed consentThe authors declare that no patient data appear in this article.
Conflict of interestThe authors declare no conflict of interest of any nature.
To the medical and nursing team of Hospital San José for their support and participation in the evaluation of this patient.
Please cite this article as: Mier EEA, Díaz PT, Fernández OSJ, Mier SG, Valdes CA. Pseudo-obstrucción colónica aguda (síndrome de Ogilvie) post-trasplante renal. Bol Med Hosp Infant Mex. 2016;73:250–255.