Reference methods for the quantification of the glomerular filtration rate (GFR) are difficult to use in clinical practice; formulas for evaluating GFR based on serum creatinine (SCr) and/or creatinine clearance are used. The aim of this study was to quantify the correlation and concordance of GFR with creatinine clearance in 24-hour urine (GFR24) and Schwartz and Schwartz updated formulas.
MethodsCross-sectional study involving healthy pediatric patients and with chronic kidney disease (CKD) from 5 to 16.9 years. Linear correlation between GFR 24 and two formulas was evaluated with the Pearson correlation coefficient (r) and intraclass correlation coefficient (ICC).
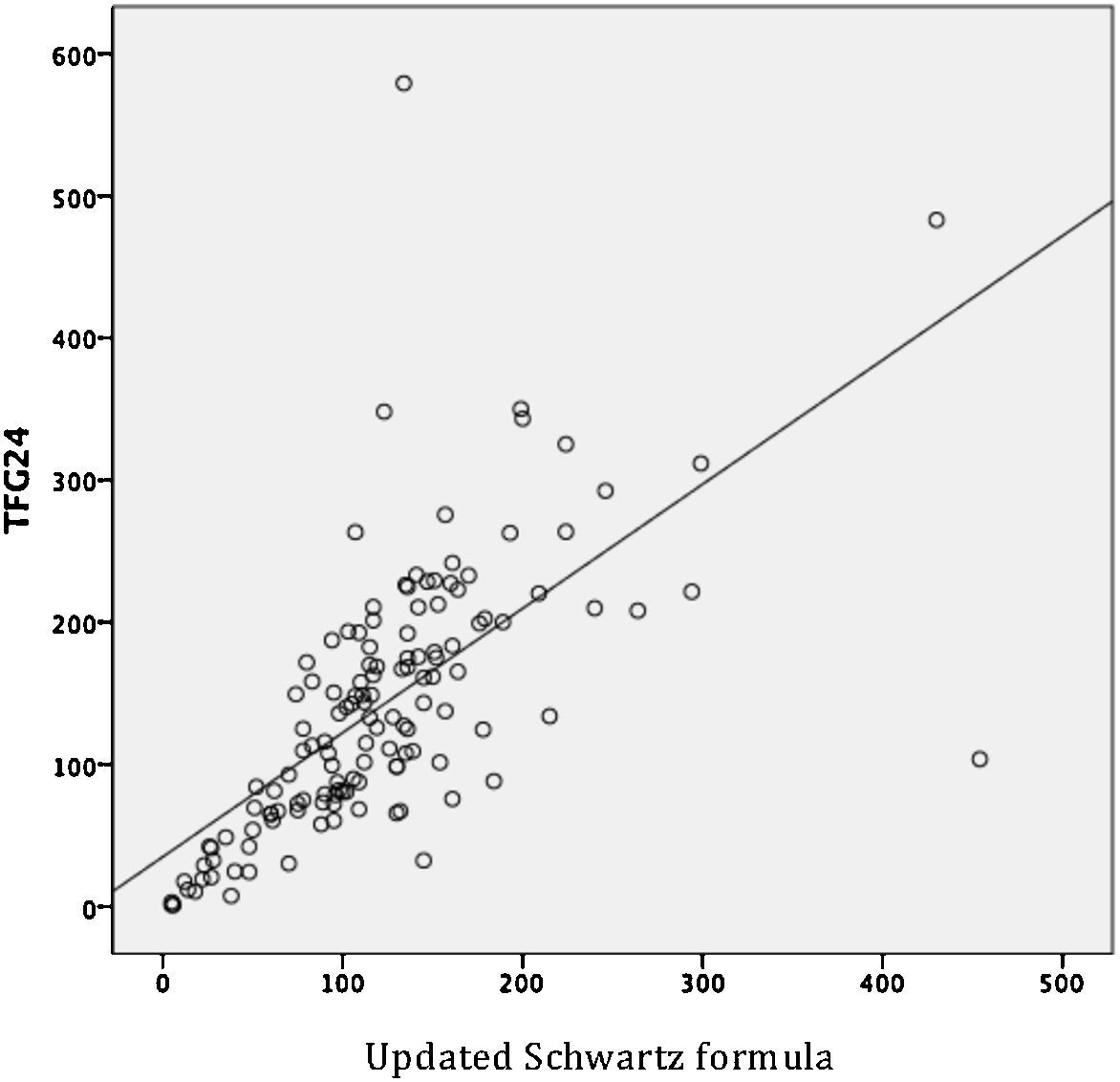
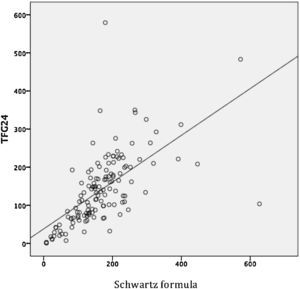
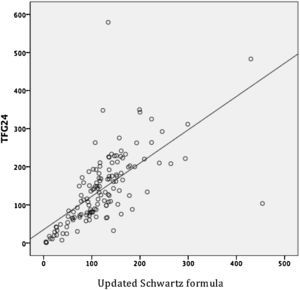
ResultsWe studied 134 patients, of which 59.7% were male. Mean age was 10.8 years. The average GFR24 was 140.34ml/min/1.73m2; 34.3% (n=46) had GFR <90ml/min/1.73m2. Moderate linear correlation between GFR24 and Schwartz (r= 0.63) and Schwartz updated (r= 0.65) formulas was observed. There was good concordance between the GFR24 and Schwartz (ICC= 0.77) and updated Schwartz (ICC= 0.77) formulas. Schwartz classical formula in patients with GFR24 ≥ 90ml/min/1.73m2 estimated higher values, while Schwartz updated underestimated values.
ConclusionsThere is moderate correlation and good concordance between the GFR24 and Schwartz and Schwartz updated formulas. The concordance was better in patients with obesity and lower in women, patients with hyperfiltration and normal weight.
Los métodos de referencia para cuantificar la tasa de filtración glomerular (TFG) son poco accesibles en la práctica clínica. Para evaluar la TFG se utilizan fórmulas basadas en la creatinina sérica y/o aclaramiento de creatinina. El objetivo de este estudio fue cuantificar la correlación y concordancia de la TFG con depuración de creatinina en orina de 24 horas (TFG24) y fórmulas de Schwartz y Schwartz actualizada.
MétodosEstudio transversal analítico que incluyó pacientes de 5 a 16.9 años, sanos y con enfermedad renal crónica. Se evaluó la relación lineal entre la TFG24 y ambas fórmulas con el coeficiente de correlación de Pearson (r) y la concordancia con el coeficiente de correlación intraclase (CCI).
ResultadosSe estudiaron 134 pacientes, 59.7% de género masculino, la edad promedio fue 10.8 años. La TFG24 promedio fue 140.34ml/min/1.73m2; el 34.3% (n=46) presentaron TFG<90ml/min/1.73m2. Se observó moderada relación lineal entre la TFG24 y las fórmulas de Schwartz (r= 0.63) y Schwartz actualizada (r= 0.65). Hubo buena concordancia entre la TFG24 y fórmula de Schwartz (CCI= 0.77) y de Schwartz actualizada (CCI= 0.77). En pacientes con TFG24 ≥ 90ml/min/1.73m2 la fórmula de Schwartz clásica estimó valores mayores de TFG, mientras que Schwartz actualizada subestimó los valores.
ConclusionesExiste moderada correlación y buena concordancia entre la TFG24 y fórmulas de Schwartz y Schwartz actualizada. Con ambas fórmulas la concordancia fue mayor en pacientes con obesidad y menor en mujeres, pacientes con hiperfiltración y con peso normal.
Chronic kidney disease (CKD) is defined as the abnormality of structure or renal function which persists for more than three months and has implications on health. The diagnosis is established by the presence of a decrease in the glomerular filtration rate (GFR) < 60ml/min/1.73m2; or the presence of one or more renal failure markers, such as albuminuria, abnormalities in the urine sediment, electrolyte imbalance due to tubular disorders, histological abnormalities, structural alterations or history of transplantation, irrespective of GFR level.1
The reference methods for the estimation of GFR use the renal clearance of exogenous substances such as insulin and chromium-51-ethylenediamine tetraacetic acid (51Cr-EDTA), iohexol iothalamate. However, they are invasive high-cost methods and difficult to implement in practice both in studies of scrutiny and monitoring of patients with CKD.2–4Different conditions such as gender, muscle mass, a high protein diet, intake of drugs or the presence of chemical interference (glucose, bilirubin) can influence the values of serum creatinine. Therefore, its accuracy to estimate GFR alone is not suitable given the heterogeneity of results and the variability in its ability to predict GFR.1,5
For the initial evaluation of GFR, it is recommended to use formulas based on serum creatinine SCr and patients with filtration rates of < 60ml/min/1.73 m2, and to confirm the results of additional measurements of clearance of cystatin C.1,5,6 The quantification of SCr should be performed using tests that comply with international reference standards and that are comparable with the isotope dilution mass spectrometry (IDMS).1,7
Since 1976, Schwartz formula has been used to estimate GFR in patients under 18 years of age. However, due to the implementation of new methods that replaced the Jaffé reaction to quantify the SCr, the formula has been less used because it overestimates the GFR.4,8–12 In 2009, Schwartz et al. proposed an updated formula to be used when the measurement of Scr is performed by enzymatic methods.4
Normal GFR values depend on the age, gender and height, and are approximately 126.5 ± 24ml/min/1.73 m2 in children from two to five years of age, and 116.7 ± 20.2ml/min/1.73 m2 in scholars and adolescents.3,13 Quantified or estimated GFR could be classified as normal (GFR ≥ 90ml/min/1.73 m2), mild decrease (GFR ≥ 60-89ml/min/1.73 m2), moderate decrease (GFR 30-59ml/min/1.73 m2), severe decrease (GFR 15-29ml/min/1.73 m2) or indicative of renal failure (GFR < 15ml/min/1.73 m2).1 Glomerular hyperfiltration is an absolute increase of the GFR value of more than two standard deviations (SD) above the expected mean value for healthy individuals or a GFR > 140 ml/min/1.73 m2.14,15
The CKD has increased its frequency worldwide. It has been estimated that in Mexico, in urban areas, the prevalence of patients with GFR < 15ml/min is 1/142 per million people, a frequency similar to the one recorded in industrialized countries. Based on this information, it is estimated that only one in four patients requiring renal replacement therapy have access to treatment.16
In Mexican children under 15 years of age, a prevalence of CKD of 0.7% has been quantified by applying the criteria of the Kidney Disease Outcomes Quality Initiative.17 However, in the general population, the most commonly used screening tests are based on the decrease in GFR determined from SCr as endogenous marker and indicator of renal damage. Moreover, this measurement cannot estimate the actual frequency and severity of CKD.
The objective of this study was to quantify the concordance of the GFR measured from clearance of creatinine in 24-hour urine, Schwartz formula, and updated Schwartz formula.
2MethodsAn analytic cross-sectional study was conducted in the Hospital Civil Dr. Juan I. Menchaca (HCGJIM) in the city of Guadalajara, Jalisco, Mexico. The study period was from March 1st to December 31st, 2014. The project was approved by the Ethics and Research Committees of the Institution (log 030/15). The HCGJIM is an institution that provides health services to a population with limited economic resources, located in the Western of Mexico.
2.1Inclusion and exclusion criteriaPatients from 5 to 16 years 11 months of age from the outpatient clinic and pediatric nephrology of the HCGJIM of both genders, healthy and with CKD at different stages were included. The sampling was non-probability because of the inclusion of volunteers. For the calculation of the sample size, a table of Montecarlo simulations with the intention of obtaining a Pearson correlation of 0.80 (error in the estimate of 0.05) and a 0.90 confidence level was used.18
Patients with paraplegia, amputees, liver disease, collagen diseases or a history of consumption or administration of cephalosporins, cimetidine, trimethoprim/sulfamethoxazole, ascorbic acid or corticosteroids within one week before the start of the study were excluded since these drugs alter the levels of SCr.
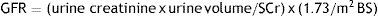
2.2Collection and processing of samplesGFR was estimated in all patients with creatinine clearance in 24-hour urine, Schwartz formula, and updated Schwartz formula. The blood samples to quantify the SCr were taken in 8-hour fast and consisted of a minimum volume of 7ml. The Jaffé method standardized by IDMS was used (UniCel® DxC 600/800 Systems and SYNCHRON®). Results were expressed in mg/dl. For the determination of creatinine clearance, 24-hours urine was collected starting with the second sample after 6 o’clock in the morning. From the total sample collected, an aliquot was taken to measure urinary creatinine in mg/dl. Patients who presented values of urinary creatinine outside normal ranges were excluded as an improper collection of urine. The reference values for urinary creatinine were the following: patients ≤ 8 years, 0.11-0.68g/24h; 9 to 12 years, 0.17-1.41g/24h and patients ≥ 13 years, 0.29-1.87g/24h.3,19 Before the collection of the samples, the guardians of the patients signed the appropriate informed consent.
2.3Estimation of GFRTo calculate GFR from creatinine clearance, the product of creatinine present in urine (mg/dl) x the volume of urine (ml/min) was divided by the concentration of plasmatic creatinine (mg/dl) and was corrected to an area of body surface (BS) of 1.73 m2:
DuBois formula20 was used for the estimation of body surface area:
In the classic Schwartz formula (GFR = k x height (cm)/SCr (mg/dl)), the constant (k) value was different depending on the age of the patients: 0.55 for children under 13 years of age, and 0.57 and 0.70 for males and females older than 13 years old, respectively.8 In the updated Schwartz formula (GFR = 0.413 x height(cm)/SCr (mg/dl)), k value was 0.413 for every sample.9,21
Patients were weighed and measured, and their body mass index was estimated (BMI = weight (kg)/height(cm)2). Measurements were performed by the same person using calibrated scales and stadiometers. Depending on the age and BMI percentile22, the patients were classified as underweight, healthy weight, overweight and obese. They were also classified according to the GFR, considering the following reference values: normal (GFR 90-140ml/min/1.73 m2), mild decrease (GFR ≥ 60-89ml/min/1.73 m2), moderate decrease (GFR 30-59ml/min/1.73 m2), severe decrease (GFR 15-29ml/min/1.73 m2), and indicative of kidney failure (GFR < 15ml/min/1.73 m2).1,23 Measurements of GFR > 140 ml/min/1.73 m2 were recorded as hyperfiltration.14
2.4Statistical analysisFrequencies and percentages were estimated from the qualitative variables; for quantitative variables, mean, standard deviation and ranges were calculated. The GFR values estimated from GFR24, Schwartz formula and updated Schwartz formula were compared, and the mean differences (MD) were quantified with 95% confidence intervals (CI) and p value. P value ≤ 0.05 was considered significant.
The Pearson correlation coefficient (r) was used to evaluate the linear relationship between the GFR calculated from creatinine clearance in 24-hour urine, Schwartz formula, and updated Schwartz formula. Concordance was determined using the intraclass correlation coefficient, which according to GFR estimates the correlation levels examining probable sources of variability (patients, observers, and measurement). Concordance values are from 0 to 1. They were considered very good if they were > 0.9, good 0.71-0.90, moderate 0.51-0.70, poor 0.31-0.50 and null < 0.31.
The concordance of the GFR obtained was calculated with Schwartz formula and updated Schwartz formula from creatinine clearance in 24-hour urine in subgroups of patients depending on gender, BMI, and stage of kidney disease. For the calculations, IBM SPSS Statistics Version 20 software was used.
3ResultsOne-hundred and thirty-four patients were included in the study, 59.7% male (n = 80) and 40.3% female (n = 54). The mean age was 10.8 years (minimum 5, maximum 16, SD 3.6). According to the BMI, 10.4% (n= 14) presented underweight, 55.2% (n = 74) normal weight, 20.1% (n = 27) overweight and 14.2% (n = 19) obesity. Before the study, 12.7% (n = 17) were known to have CKD.
The average of GFR values measured from creatinine clearance in 24-hour urine (GFR24) was 140.34ml/min/1.73 m2 (maximum 579.3, minimum 0.926). Depending on the GFR24, it was noted that 65.6% (n = 88) presented normal or increased GFR; 18.7% (n = 25) mild decrease; 6.7% (n = 9) moderate decrease; 4.5% (n = 6) severe decrease and 4.5% (n = 6) values indicative of renal failure; 47% (n = 63) presented GFR > 140ml/min/1.73 m2.
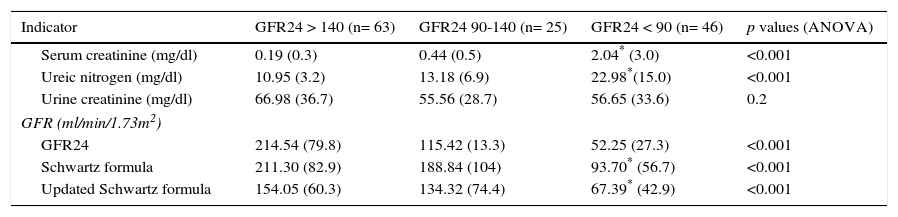
Statistically significant differences in the values of SCr, urea nitrogen and GFR estimated from Schwartz formula and updated Schwartz formula were observed (Table 1) when classifying the patients as normal (n = 25), glomerular hyperfiltration (n = 63) or with decreased GFR (< 90 ml/min/1.73 m2) (n = 46). Interestingly, to distinguish between normal subjects and patients with decreased GFR, Schwartz formula and updated Schwartz formula overestimated the GFR24 value, while to differentiate normal subjects from patients with hyperfiltration, Schwartz formula overestimated and updated Schwartz formula underestimated the GFR24 value.
Mean and standard deviation of biochemical indicators and GFR from Schwartz formula and updated Schwartz formula according to GFR24.
| Indicator | GFR24 > 140 (n= 63) | GFR24 90-140 (n= 25) | GFR24 < 90 (n= 46) | p values (ANOVA) |
|---|---|---|---|---|
| Serum creatinine (mg/dl) | 0.19 (0.3) | 0.44 (0.5) | 2.04* (3.0) | <0.001 |
| Ureic nitrogen (mg/dl) | 10.95 (3.2) | 13.18 (6.9) | 22.98*(15.0) | <0.001 |
| Urine creatinine (mg/dl) | 66.98 (36.7) | 55.56 (28.7) | 56.65 (33.6) | 0.2 |
| GFR (ml/min/1.73m2) | ||||
| GFR24 | 214.54 (79.8) | 115.42 (13.3) | 52.25 (27.3) | <0.001 |
| Schwartz formula | 211.30 (82.9) | 188.84 (104) | 93.70* (56.7) | <0.001 |
| Updated Schwartz formula | 154.05 (60.3) | 134.32 (74.4) | 67.39* (42.9) | <0.001 |
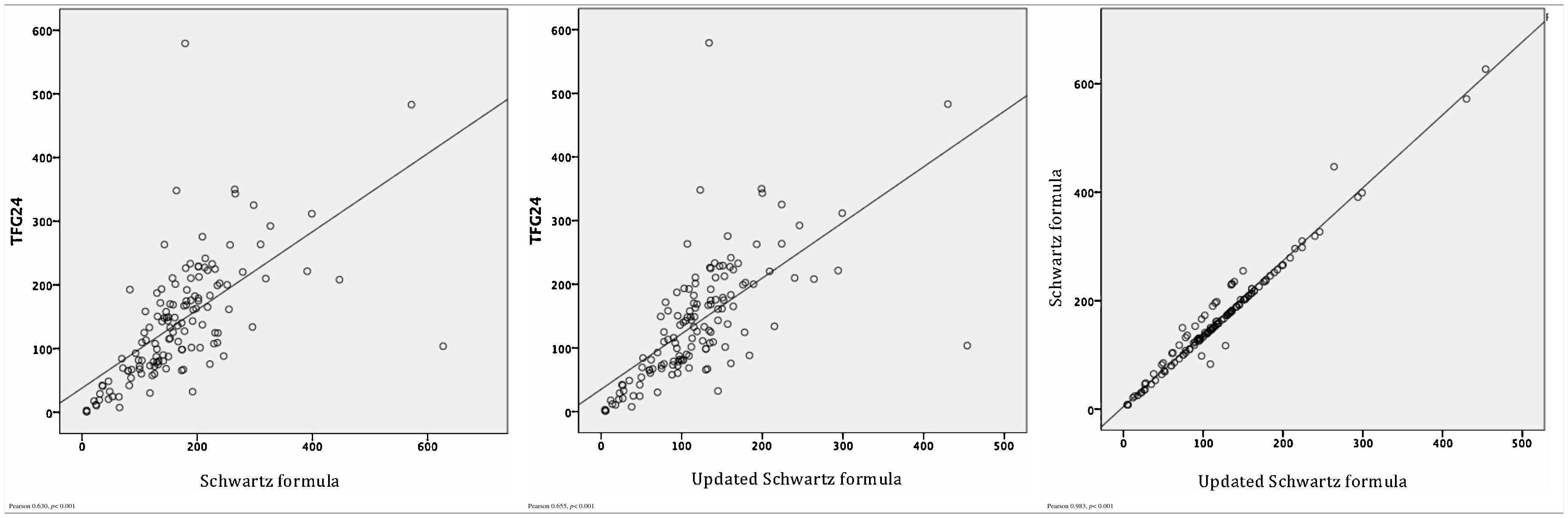
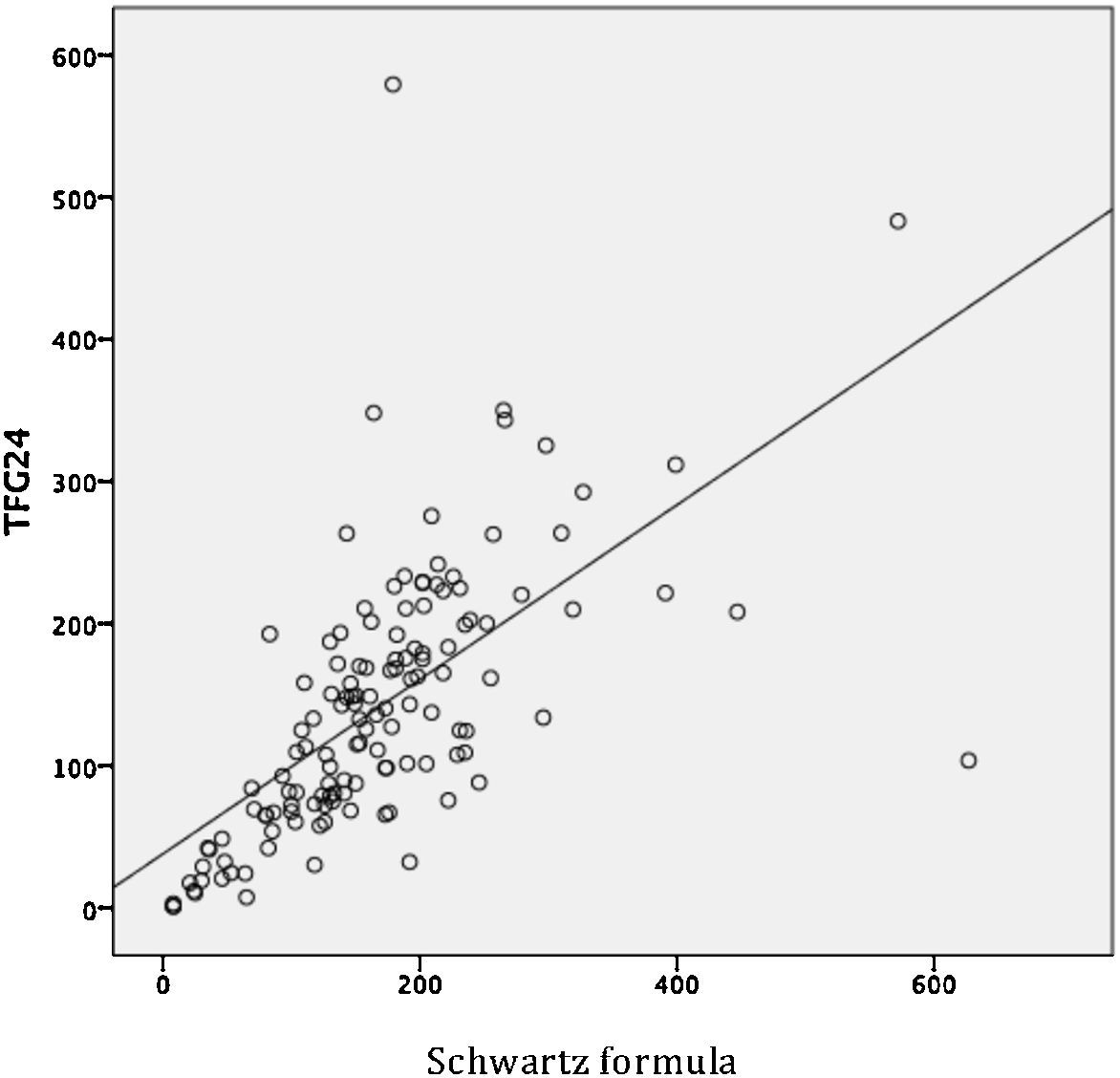
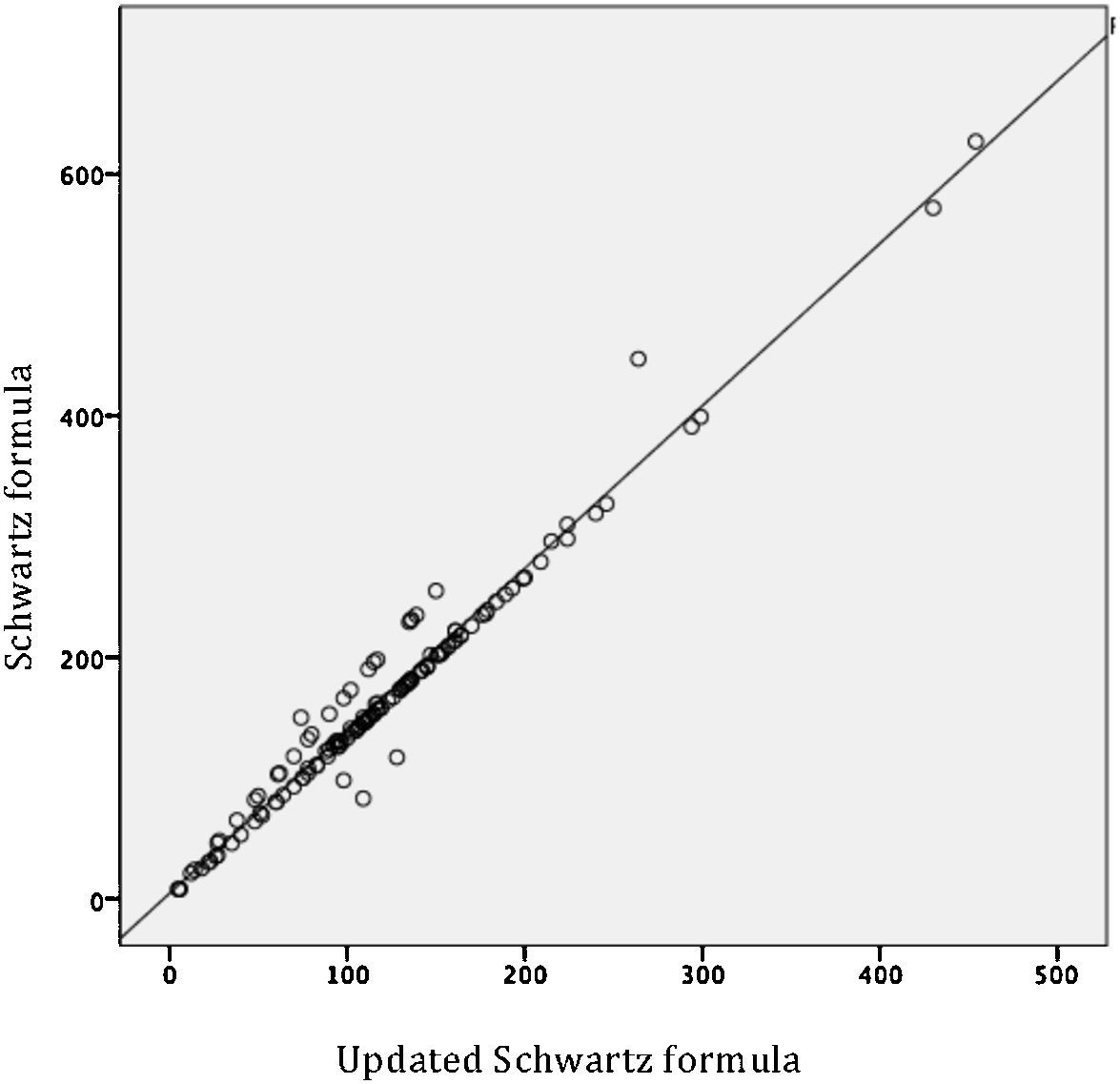
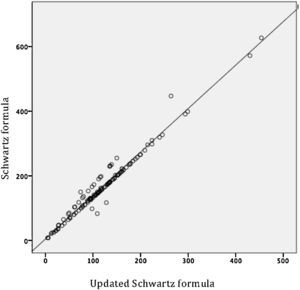
By evaluating the linear relationship between the three estimators of the GFR, a moderate relationship between GFR24 and Schwartz formula (r = 0.630, p < 0.001), and GFR24 and updated Schwartz formula (r = 0.655, p < 0.001) were observed. The indicator was adequate to evaluate the relationship between Schwartz formula and updated Schwartz formula (r= 0.983, p < 0.001) (Table 2). However, the MD between GFR determined from both formulas was significantly different (MD 46.1, 95% CI 41 to 51.1; p < 0.001), which demonstrated that a good linear correlation is not indicative of reliability.
In patients with GFR24 ≥ 90ml/min/1.73 m2 (n = 88), the updated Schwartz formula underestimated values of the GFR24 (MD -37.94, 95% CI -54.7 to -21.19, p < 0.001), while the classic Schwartz formula estimated higher values (MD 18.5, 95% CI -1.5 to 38.6, p < 0.07).
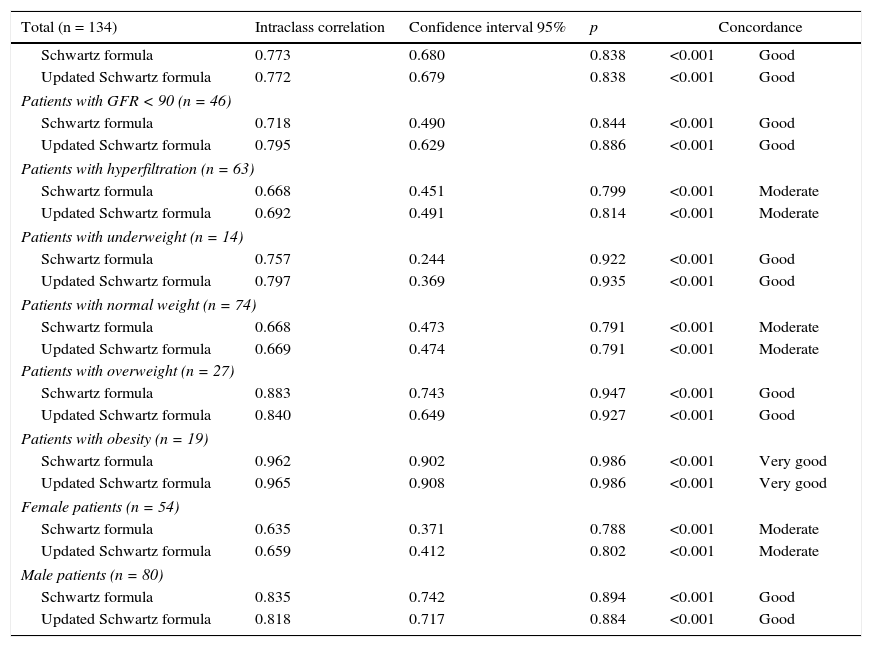
Using the intraclass correlation coefficient (ICC), a good concordance between the GFR24 from Schwartz formula (ICC= 0.77) and updated Schwartz formula (ICC= 0.77) was quantified. In the subgroup analyses, it was observed that the concordance of the GFR24 and Schwartz formula (ICC= 0.96) and updated Schwartz formula (ICC= 0.96) was very good in obese patients, while the concordance was moderate in patients with hyperfiltration, healthy weighted and females (Table 3).
Concordance of GFR24 from Schwartz formula and updated Schwartz formula.
| Total (n = 134) | Intraclass correlation | Confidence interval 95% | p | Concordance | |
|---|---|---|---|---|---|
| Schwartz formula | 0.773 | 0.680 | 0.838 | <0.001 | Good |
| Updated Schwartz formula | 0.772 | 0.679 | 0.838 | <0.001 | Good |
| Patients with GFR < 90 (n = 46) | |||||
| Schwartz formula | 0.718 | 0.490 | 0.844 | <0.001 | Good |
| Updated Schwartz formula | 0.795 | 0.629 | 0.886 | <0.001 | Good |
| Patients with hyperfiltration (n = 63) | |||||
| Schwartz formula | 0.668 | 0.451 | 0.799 | <0.001 | Moderate |
| Updated Schwartz formula | 0.692 | 0.491 | 0.814 | <0.001 | Moderate |
| Patients with underweight (n = 14) | |||||
| Schwartz formula | 0.757 | 0.244 | 0.922 | <0.001 | Good |
| Updated Schwartz formula | 0.797 | 0.369 | 0.935 | <0.001 | Good |
| Patients with normal weight (n = 74) | |||||
| Schwartz formula | 0.668 | 0.473 | 0.791 | <0.001 | Moderate |
| Updated Schwartz formula | 0.669 | 0.474 | 0.791 | <0.001 | Moderate |
| Patients with overweight (n = 27) | |||||
| Schwartz formula | 0.883 | 0.743 | 0.947 | <0.001 | Good |
| Updated Schwartz formula | 0.840 | 0.649 | 0.927 | <0.001 | Good |
| Patients with obesity (n = 19) | |||||
| Schwartz formula | 0.962 | 0.902 | 0.986 | <0.001 | Very good |
| Updated Schwartz formula | 0.965 | 0.908 | 0.986 | <0.001 | Very good |
| Female patients (n = 54) | |||||
| Schwartz formula | 0.635 | 0.371 | 0.788 | <0.001 | Moderate |
| Updated Schwartz formula | 0.659 | 0.412 | 0.802 | <0.001 | Moderate |
| Male patients (n = 80) | |||||
| Schwartz formula | 0.835 | 0.742 | 0.894 | <0.001 | Good |
| Updated Schwartz formula | 0.818 | 0.717 | 0.884 | <0.001 | Good |
GFR24, glomerular filtration rate from creatinine clearance in 24-hour urine.
According to the Ministry of Health Guidelines for Clinical Practice24 for the early detection of CKD in patients under 18 years of age, the estimation of GFR from Schwartz formula or by quantifying the creatinine clearance in 24-hour urine is suggested.
In this study, it was demonstrated that the GFR24 showed good correlation with both Schwartz formula and updated Schwartz formula. However, it was also noted that in patients with GFR24 ≤ 140 ml/min/1.73 m2 both formulas overestimated the values of GFR24, which is important since these tests are used as screening to detect early CKD. However, the difference between the means of the estimations is heterogeneous, and therefore the sensitivity is variable, which results in undetected CKD events using the formulas.
Deng et al.10 evaluated the accuracy and concordance of fourteen different formulas to estimate GFR in children, including the updated Schwartz formula, using the iohexol clearance as reference test. Updated Schwartz formula showed good correlation (r= 0.77, p < 0.001), with an accuracy of 65%. The formulas that showed greater accuracy and better performance were the ones that included values of SCr, cystatin, gender, and growth parameters.
In pediatric patients of the HCGJIM, a moderate correlation between the GFR24 and Schwartz formula (r= 0.630, p < 0.001), and updated Schwartz formula (r= 0.655, p < 0.001) was shown, but the results were not compared with any reference method for the estimation of GFR. SCr is the most commonly used endogenous marker to estimate GFR, and in recent decades the Schwartz formula has been the most used. However, when using these tests, the clinician should be aware of the risk of false negative results; therefore, considering the simultaneous use of other clinical or biochemical indicators, especially in patients with high risk of CKD9 is suggested.
Gheissari et al.4 observed in healthy children aged seven to 18 years (n = 712) a high concordance (MD 0 ± 12.7ml/min/1.73m2) between the GFR from updated Schwartz formula and Schwartz combined formula, which includes the values of SCr, cystatin, gender, and growth parameters. The percentage of agreement between both formulas to identify patients with GFR < 60mL/min/1.73m2 was 85% (K = 0.85; 95% CI 0.69-1).
Pottel et al.11 noted that the updated Schwartz formula is useful in healthy children aged 6 to 14 years, but they suggest that the constant (k) should be adapted to the age in younger children. Using the determination of GFR with 51Cr-EDTA as a reference test, and a cut-off point of < 90ml/min/1.73 m2, the sensitivity, and specificity of the updated Schwartz formula were 63.4% and 62.9%, respectively, with an area under the curve of 0.739 ± 0.03. The same authors noticed that a linear relationship between the age of one to fifteen years and the GFR adjusted value (r2= 0.994) exists, and not adjusted to the body surface area (r2= 0.932).
From the available formulas based on the SCr to estimate GFR, the United States National Kidney Disease Education Program (NKDEP) has suggested that the updated Schwartz formula is the most suitable.3,4 Moreover, it is a fast, cheap and easy method to implement.19 However, its limitations in patients with high risk of CKD must be acknowledged due to the possibility of false negative results.4,23
Forty-seven percent of the patients in the HCGJIM included in this study had GFR > 140 ml/min/1.73 m2; hence, they were classified as glomerular hyperfiltration patients. It is noteworthy that there is still no consensus on the cut-off point for classifying patients with this condition, and cut-off points from 125 to 175ml/min/1.73 m2 have been applied.15
Although the glomerular hyperfiltration may occur in healthy individuals with a high-protein content diet, it can be an early indicator of kidney disease. For this reason, medical surveillance is recommended. In this study, it was observed that 13 of 19 obese patients had glomerular hyperfiltration (OR 2.8, 95% CI 1.04-8.8, p = 0.04), which has been reported elsewhere.15,25,26
The limitations of this study are the absence of a reference test or other kidney damage indicators to compare the GFR from clearance of creatinine in urine in 24hours, Schwartz formula and updated Schwartz formula. Another limitation was the medium size sample, which turned into a significant problem in the subgroup analyses.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that no patient data appear in this article.
Right to privacy and informed consentThe authors have obtained the written informed consent of the patients or subjects mentioned in the article. The corresponding author is in possession of this document.
FundingNone.
Conflict of interestThe authors declare no conflict of interests of any nature.
Please cite this article as: Salazar-Gutiérrez ML, Ochoa-Ponce C, Lona-Reyes JC, Gutiérrez-Íñiguez SI.Concordancia de la tasa de filtración glomerular con depuración de creatinina en orina de 24 horas, fórmulas de Schwartz y Schwartz actualizada. Bol Med Hosp Infant Mex. 2016;73:181–187.