Background: In Mexico there is an important gap of information regarding the quality of care for neonates with necrotizing enterocolitis (NEC). This study aimed at evaluating the quality of care for neonates with NEC affiliated with the program Medical Insurance Century XXI (MIC-XXI), which is a branch of Seguro Popular.
Methods: From December 2011 to March 2012, a cross-sectional study took place in 61 hospitals of the Ministry of Health located in 22 Mexican states. A set of 16 quality indicators based on a literature review served for the evaluation.
Results: We reviewed 262 medical records of neonates with NEC. More than half were male and born by caesarean section; 55.8% were premature, 55.3% had low birth weight and 12.2% died. Regarding the quality of care, 72.5% were breastfed before being diagnosed with NEC. Most cases had abdominal radiography (90%), 75.0% had diagnosis of NEC according to Bell's criteria, but only 30% had reported symptoms that met the criteria for the recorded stage. Suspension of enteral feeding and administration of antibiotics reached 95.8% and 93.9%, respectively. Twenty six neonates underwent surgery, of which 34% had reported radiographic findings.
Conclusion: A wide margin exists to improve the quality of care of neonates with NEC in Mexican Hospitals.
1. Introduction
Necrotizing enterocolitis (NEC) is an acute gastrointestinal disease that occurs during the neonatal period and is a common cause of admission to neonatal intensive care units (NICU). This disease comprises intestinal necrosis and multiple organ failure. Ninety percent of neonates with NEC are premature. Almost 12% of infants born weighing <1500 g will develop NEC; among those, about 30% will not survive.1 Near-term and full-term infants also develop the disease. The worldwide prevalence rate of NEC among premature babies ranges from 0.3 to 2.4 per 1000 live births (LB), whereas it is 0.05 per 1000 LB among term neonates. Mortality rate due to NEC is 12.4 deaths per 100,000 LB.2
There is a different pattern of risk factors between NEC in premature and full-term infants. The main risk factors for NEC are prematurity, feeding the neonate with formula, intestinal ischemia, red cell transfusions and intestinal colonization by pathological bacteria.3,4 In newborns after 35 weeks' gestation the main risk factors are low Apgar scores, birth asphyxia, sepsis, or congenital cardiac or gastrointestinal anomalies.5 In late-term infants, the risk factors associated with NEC are early-onset sepsis, drug exposure, respiratory distress and being fed only with formula.6
There are several primary prevention strategies for NEC that include administration of corticoids to the mother during labor before preterm delivery. For preterm neonates the recommendations comprise feeding with human milk, liquid restriction and use of probiotics.7
Most NEC cases receive pharmacological treatment in neonatal intensive care units and between 20% and 40% require surgical treatment. However, up to 50% of those who undergo surgery may die due to complications. Once the diagnosis has being made, two thirds of NEC deaths happen with the first 7 days (mean 1 day). The main risk factors for death due to NEC are low gestational age, low birth weight, treatment with assisted ventilation and use of vasopressors at the time of diagnosis.8
Despite the progress in the neonatal care arena, prevalence of NEC has not decreased. This in part is due to the increase in the survival rate of very low birth weight premature neonates. These circumstances point out the importance of the provision of effective preventive care such as the implementation of feeding guidelines and availability and use of human milk9 along with medical and surgical treatment that must be congruent with current best medical practices.10,11
The Mexican government has in place different policies and programs to provide healthcare to infants and newborns. In December 2006, Seguro Popular launched the noncontributory health insurance program "Medical Insurance for the New Generation" that, in 2013, was renamed as Medical Insurance Century XXI (MIC-XXI). MIC-XXI aims at improving access and contributing to decrease impoverishment due to health causes through universal insurance for all children born after December 2006 who are not affiliated with a social security institution.12 Currently, six million children are affiliated with this program.13
MIC-XXI finances the treatment of NEC among several other conditions of neonates who receive care in hospitals affiliated with the Ministry of Health (MoH). These hospitals must be certified before being able to receive funds to provide healthcare to MIC-XXI beneficiaries. The certification implies that the hospital must have appropriately trained health personnel, availability of equipment, and having neonatal intensive care units. Nonetheless, the certification is a snapshot of the capability of the hospitals and there are no routine evaluations of the quality of care that these hospitals provide; in fact, the practice of evaluating the quality of care is incipient in pediatric hospitals in the country and has not been fully institutionalized.14
In Mexico, little is known about the current prevalence and mortality rates of neonates with NEC admitted to NICUs and no formal studies have been conducted to evaluate the quality of care for this condition. Lack of proper health information systems and of quality of care indicators along with a poorly developed culture of evaluation contribute to these circumstances. To bridge the gaps of clinical information regarding NEC care in Mexican hospitals, the main objective of this study was to evaluate the quality of care that neonates with NEC receive in hospitals affiliated with MIC-XXI.
2. Methods
From December 2011 to March 2012, a cross-sectional study took place in 61 hospitals of the MoH located in 22 Mexican states. All these hospitals must have affiliation with the MIC-XXI and provide medical care to at least two NEC cases in the first semester of 2011. During that year, 505 neonates were admitted with diagnosis of NEC, of whom 11.9% died. The sampling design considered the total number of NEC cases who received care in these hospitals, from which a random sample of recently discharged cases was selected. It was decided to select up to four cases per hospital.
The variables of the study were the following:
Characteristics of the mothers—age, marital status, occupation (housewife or work outside the house), gravidity (nulliparous or multigravida), pre-existing chronic diseases and history of antenatal care that included attendance at MoH facilities, initiation of antenatal care during the first trimester of gestation and pregnancy complications.
Characteristics of the neonates with NEC—sex, gestational age (immature (<28 weeks), premature (28-37 weeks), term (>37 and ≤41), post-term (≥42 weeks) and birth weight. Type of delivery and characteristics of the hospital care— type of delivery (vaginal delivery, cesarean section), characteristics of the referral to the neonatal intensive care unit, length of stay and comorbidity.
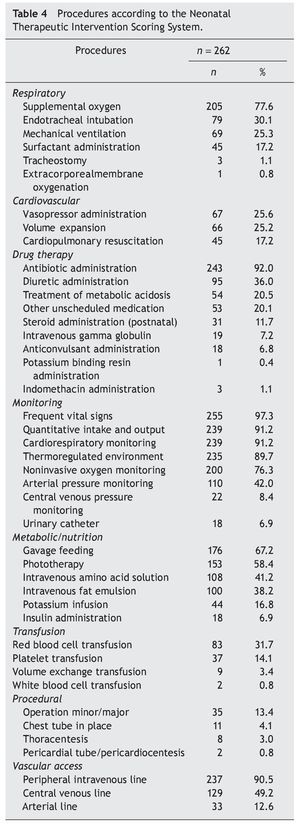
Severity of the neonatal disease measured through the Neonatal Therapeutic Intervention Scoring System (NTISS)15—The NTISS takes into account the therapeutic intensity and complexity to score the severity of the condition. It is based on the assumption that the treatment intensity correlates directly with the severity of disease. NTISS score is computed as the arithmetic sum of therapy points received by the neonate in a 24-h period, ranging from 0 to 47. The highest score means greater treatment intensity and, consequently, more severity of the neonate. The total NTISS score is the sum of eight subscores (respiratory, cardiovascular, drug therapy, monitoring, metabolic/ nutrition, transfusion, procedural and vascular access). The conditions of the neonate at hospital discharge were also documented.
Quality of care—A set of quality indicators served to evaluate the quality of NEC care. Three pediatricians, including one neonatologist, conducted the review of the literature and developed the set of 16 indicators. The review comprised clinical guidelines, systematic reviews and the protocol that MIC-XXI issued for NEC care. To propose the quality of care indicators, the literature was examined in terms of its scientific validity and local feasibility. The indicators addressed three fields: prevention, diagnostic procedures and treatment.
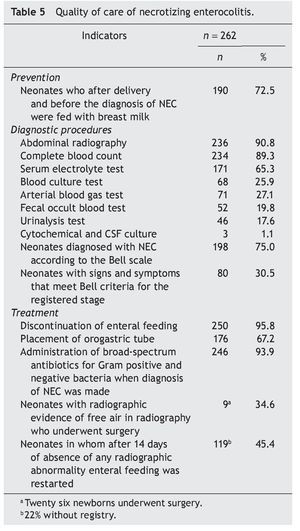
• Prevention focused on neonates who, after delivery and before the diagnosis of NEC, were fed with breast milk.
• Diagnostic procedures performed such as abdominal radiography, complete blood count, serum electrolytes, blood cultures arterial blood gas, fecal occult blood, urinalysis, cytochemical and CSF culture. The Bell scale was used to diagnose and classify neonates with NEC.
• Treatment criteria included discontinuation of enteral feeding, placement of orogastric tube, administration of broad-spectrum antibiotics for gram positive and negative bacteria when diagnosis of NEC was made, neonates who underwent surgery with radiographic evidence of free air in radiography and neonates in whom after 14 days of absence of any radiographic abnormality, enteral feeding was restarted.
2.1. Data collection method
Previously trained pediatricians gathered the information directly from the clinical records in a data collection instrument developed ad hoc. All the information was registered in a database. The Commission of Ethics and Research of Hospital Infantil de Mexico Federico Gomez authorized the study protocol.
2.2. Statistical analysis
The information was analyzed using descriptive statistics. The analysis was performed using the statistical package Stata 8.0 (Stata 8.0, Stata Corp., College Station, TX).
3. Results
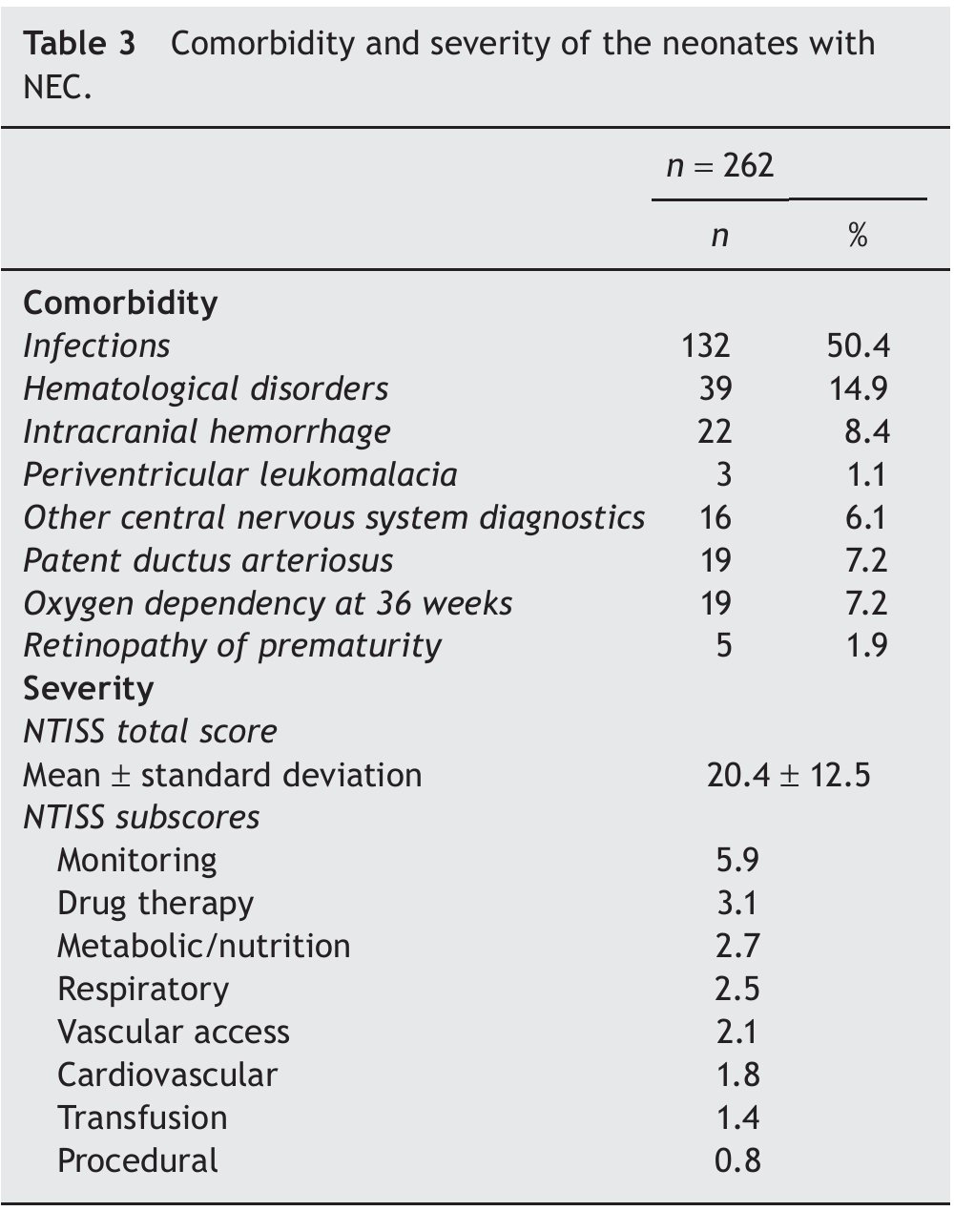
The study included 262 medical records of neonates diagnosed with NEC who were treated in neonatal intensive care units (NICU) of 61 MoH hospitals. Table 1 presents the characteristics of the mothers of these neonates; the median age was 23.5 years, most were single or divorced, and 80.9% were housewives. One third were nulliparous and most had received antenatal care in MoH facilities; less than half began antenatal care during the first trimester of gestation and almost 50% had pregnancy complications.
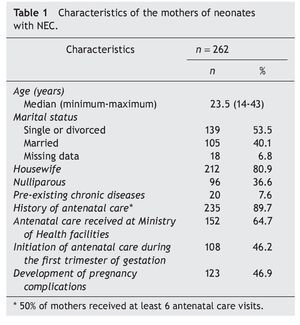
Table 2 shows the characteristics of the neonates. More than half of neonates were male and born by caesarean section; 55.8% were premature, 55.3% had low birth weight, and 17.9% weighted ≤1500 g. Most neonates with NEC were admitted to the NICU of the hospital where they were delivered; whereas 27% were transferred from another hospital, 60% were transferred by ambulance, 40% in incubator and 12% required mechanical ventilation during transportation. On average, the length of stay of a neonate with NEC was 24 days (range: 1-92 days. Regarding the health outcomes, most showed clinical improvement; however, 12.2% died and 2% had incomplete data.
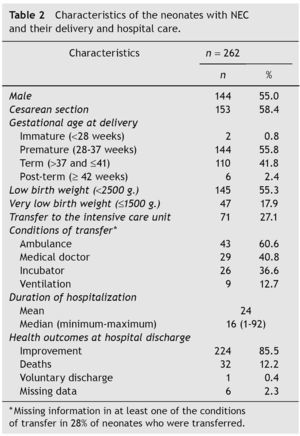
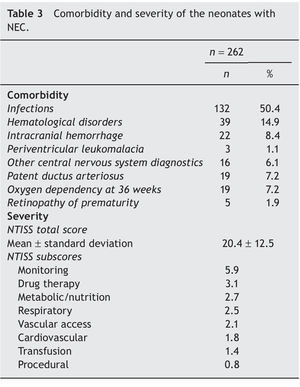
Table 3 describes the comorbidity and severity of neonates with NEC during the hospital stay. The most frequent comorbidities were infections (50.4%), hematologic complications (14.9%) and intracranial hemorrhage (8.4%). On average, the NTISS total score was 20.4 points.
Table 4 shows the therapeutic interventions received by newborns according to subscales of NITSS, which included respiratory, cardiovascular, drug therapy, monitoring, metabolic/nutrition, vascular access and transfusion. These interventions are congruent with the clinical conditions and comorbidities of neonates with NEC.
Table 5 presents the results of the quality of care evaluation using the set of indicators. Regarding the prevention component, 72.5% of neonates were fed with breast milk before being diagnosed with NEC. The component of diagnostic procedures showed that most cases had abdominal radiography and complete blood count (90% and 89%, respectively). The less performed tests were cerebrospinal fluid culture, urinalysis and fecal occult blood test; 75.0% of infants had diagnosis of NEC according to the Modifying Bell's staying criteria, but only 30% had reported signs and symptoms that met the criteria for the recorded Bell stage. Regarding the treatment component, the indicators that showed good performance were suspension of enteral feeding and administration of broad-spectrum antibiotics for Gram-positive and Gram-negative bacteria since the diagnosis of NEC was made. Other treatment indicators showed that the orogastric tube was placed in 67%. Of 26 neonates who underwent surgery, only in 34% was the radiographic finding reported and in 45% enteral feeding was restarted after 14 days of absence of any radiographic abnormality.
4. Discussion
The main findings show that there is a wide margin for improving the quality of care that neonates with NEC receive in Mexican MoH hospitals. The use of a set of indicators to measure QoC allowed identifying some key components in the areas of prevention, diagnostic procedures and treatment that can be improved. The health outcomes of the neonates in this group of hospitals were similar to what the literature reports in terms of mortality due to NEC complications; in the present study 12.2% of NEC cases died.
According to the literature, NEC occurs most frequently in preterm neonates with very low birth weight; in our study, 55.5% of neonates were premature and 42% were at term. This finding is consistent with other studies that reported an increased incidence of NEC in children born at term,16 especially among neonates admitted to the NICUs for conditions other than NEC such as congenital heart disease, polycythemia and bacterial sepsis, among others.17 Furthermore, most NEC neonates had comorbidities, primarily hematologic complications and infections.
The NTISS score reached on average 20 points. This finding depicts that neonates with NEC in the present study were at moderate to severe conditions. A previous study that validated NTISS in neonates hospitalized in NICUs in the U.S. reported an average score of 12. That study found that high NTISS score was associated with increased risk of death, longer length of stay and high costs of care.
Treatment for NEC is determined by local practices including the training of medical doctors and availability of supplies and equipment in the NICUs. In the Mexican health sector context this represents a wide variability that should be considered to perform evaluations or set standards. It is worth mentioning that the average length of stay in the present study was 24 days, which is less than the average length of stay of 49 days that has been reported in the U.S.18 Studies in other countries have found that the quality of care in NICUs is variable among hospitals,19-21 and that high quality care consistent with scientific evidence is linked with better health outcomes which, in turn, contribute to reduce mortality in this age group.
Measuring quality requires instruments that are valid and feasible. The proposed indicators may be the groundwork in the development of quality of care indicators for neonates with NEC in Mexican hospitals. It is worth completing its validation through a robust method such as the RAND-UCLA22 method that combines systematic literature review and a process that scores the validity and feasibility of the indicators by an expert group. According to the RAND-UCLA validation method, the indicator should assume that those healthcare professionals who deliver the services close to the indicator provide better quality than those who do not. In addition, an indicator is considered feasible when there is a high probability that the information for it was available in a typical clinical record. Indeed, if such information was missing, this would signal poor quality of care. For example, according to the literature, one of the indicators important for the prevention of NEC is the indication of probiotics to preterm infants; however, in the MoH hospitals probiotics are not available; thus, this indicator is not feasible. It is advisable for the MoH to consider the possibility of introducing probiotics, given the evidence of its preventive effect. A meta-analysis of 16 controlled clinical trials, which included 2842 preterm infants, found that enteral probiotic supplementation significantly reduces the incidence of severe NEC (stage II or higher) (RR 0.35, 95% CI, 24-0, 52 95) and mortality (RR 0.40, 95% CI 0.27, 0.60).23
It was not possible to assess whether antenatal steroids were given during preterm delivery because this information is not routinely registered in the NICU records, but in the mothers' clinical records. Administration of antenatal steroids aims at decreasing the risk of respiratory distress syndrome and this condition is associated with increased risk of NEC. From this perspective, it is crucial to develop effective strategies of continuous care with a preventive approach for premature neonates which includes, among others, strategies to improve data recording, e.g., use of prenatal steroids. Unfortunately, most MoH hospitals do not have electronic health records and the information was gathered from paper records. Lack of continuity in the management and registration of clinical information is an important gap to run routine evaluations of the quality of care.
The quality of care of NEC at MoH hospitals in Mexico requires improvements in all areas of the process of care: prevention, diagnosis and treatment. Although most neonates received human milk before being diagnosed with NEC, there are no explicit feeding guidelines. The current rules of operation of MIC-XXI comprise an important investment in milk banks in several hospitals of the MoH. The availability of human milk, along with the implementation of feeding guidelines, would help to decrease the severity and mortality of NEC.
The protocol that MIC-XXI issued for NEC care24 indicates that its treatment should be performed according to the Bell registered stage, which is a worldwide recommended criterion; nevertheless, a third of the neonates did not have the diagnosis based on this classification. Furthermore, only 30% of medical records had symptoms and signs that met the Bell criteria. This finding is worrisome given that this could translate to some deficiencies in the treatment of 70% of the neonates.
In this study, 20% of neonates required surgical treatment, which gives us an idea of the potential for complications in these children and the resources it implies. This figure is congruent with the assumption that between 20 and 40% of neonates with NEC would require surgical treatment. However, it was noticeable that one third of the neonates who underwent surgical treatment did not have a record of radiographic finding (presence of air) to justify the surgical procedure.
Among the study limitations, it is relevant to mention that the results are not generalizable to all health institutions in Mexico. The study was focused on MoH hospitals that were providing care to MIC-XXI affiliates. Also, the indicators should be validated with further rigor; the fact that these neonates had different comorbid conditions makes it more difficult to define generalizable indicators. The methodology used in this study can be replicated to evaluate and compare the quality of care in other hospitals in Mexico and other countries.
The evaluation of the quality of care for neonates with NEC in MoH hospitals indicates that there is wide margin for improvement. It is advisable to strengthen the implementation of clinical practice guidelines for NEC at NICUS, but also to facilitate the institutionalization of the evaluation of the quality of care in Mexican public hospitals.
Conflict of interest
The authors declare no conflict of interest of any nature.
Received 11 December 2013;
accepted 12 December 2013
* Corresponding author.
E-mail:ljasso@himfg.edu.mx (L. Jasso-Gutiérrez).