Introducción: El síndrome de la cimitarra es una compleja anomalía congénita del desarrollo pulmonar, infrecuente y de múltiples variables. Se denomina así por su semejanza radiológica con la clásica espada torcida. Su característica definitoria es el drenaje pulmonar anómalo. Se asocia con diversas malformaciones cardiotorácicas y un amplio espectro de manifestaciones clínicas.
Serie de casos: Se reporta una serie proveniente de la base de datos del Hospital Infantil de México Federico Gómez, revisión del periodo 2009-2013. Se encontraron nueve pacientes con diagnóstico de síndrome de la cimitarra. Se recabaron del expediente médico las características demográficas, estado clínico y parámetros hemodinámicos reportados.
Conclusiones: En la presente serie llaman la atención ciertas diferencias entre el grupo de estudio y lo reportado en la literatura internacional. Se encontró que la mayoría de los pacientes fueron del sexo femenino, diagnosticados entre el primero y el vigésimo mes de vida. En el momento del estudio estaban asintomáticos; la mitad contaba con antecedentes de enfermedad respiratoria y el total con hipertensión pulmonar. La tercera parte del grupo requirió manejo quirúrgico.
Background: Scimitar syndrome is a rare and complex congenital anomaly of the lung with multiple variables and is named for its resemblance to the classical radiological crooked sword. Its defining feature is the anomalous pulmonary drainage. It is associated with various cardiothoracic malformations and a wide spectrum of clinical manifestations.
Case series: Nine patients diagnosed with scimitar syndrome found in the database of Hospital Infantil de México between 2009 and 2013 were reviewed. Demographic records, clinical status and hemodynamic parameters reported were collected.
Conclusions: This case series called attention to certain differences between our group of patients and those reported in the international literature. Patients were predominantly female and were diagnosed between 1 and 20 months of life. All were asymptomatic at the time of the study. Half of the patients had a history of respiratory disease and all patients had with pulmonary hypertension. Surgical management was required in on-third of the patient group.
1. Introduction
Scimitar syndrome is characterized by an abnormal connection between one or more pulmonary veins and the systemic venous system. The vein in scimitar usually drains into the hepatic portion of the inferior cava, but can also flow into the suprahepatic vein, portal vein, azygos vein or directly into the right atrium (causing a left to right shunt).1
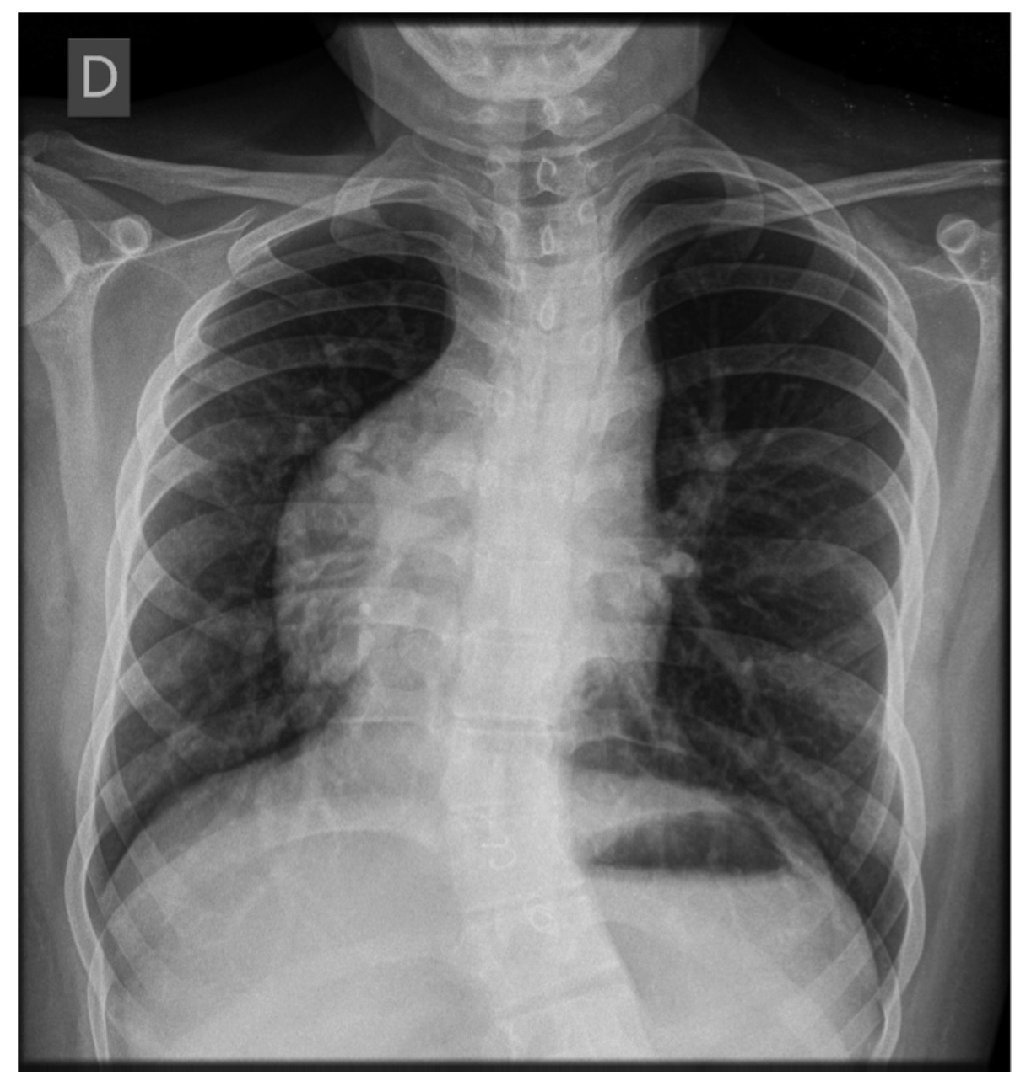
The word “scimitar” comes from the Italian derivation ‘scimitarra’, from the Persian shamsir, which refers to a curved Muslin or Oriental sword. It refers to the curvilinear opacity that the anomalous vein projects in the chest x-ray, which extends down from the right pulmonary hilum, bordering the cardiac silhouette to the homolateral cardiophrenic angle, resembling a scimitar (Fig. 1).1
Figure 1 Chest x-ray. Anterior-posterior imaging in which the cardiac silhouette and the apex towards the right is seen, suggestive of dextrocardia. Also observed is curvilinear opacity that extends from the right pulmonary hilum, surrounding the cardiac silhouette, towards the homolateral costophrenic angle, resembling a scimitar. Also seen is scoliosis with convexity towards the right and asymmetry of the chest cavity (image corresponding to a female patient 17 years of age).
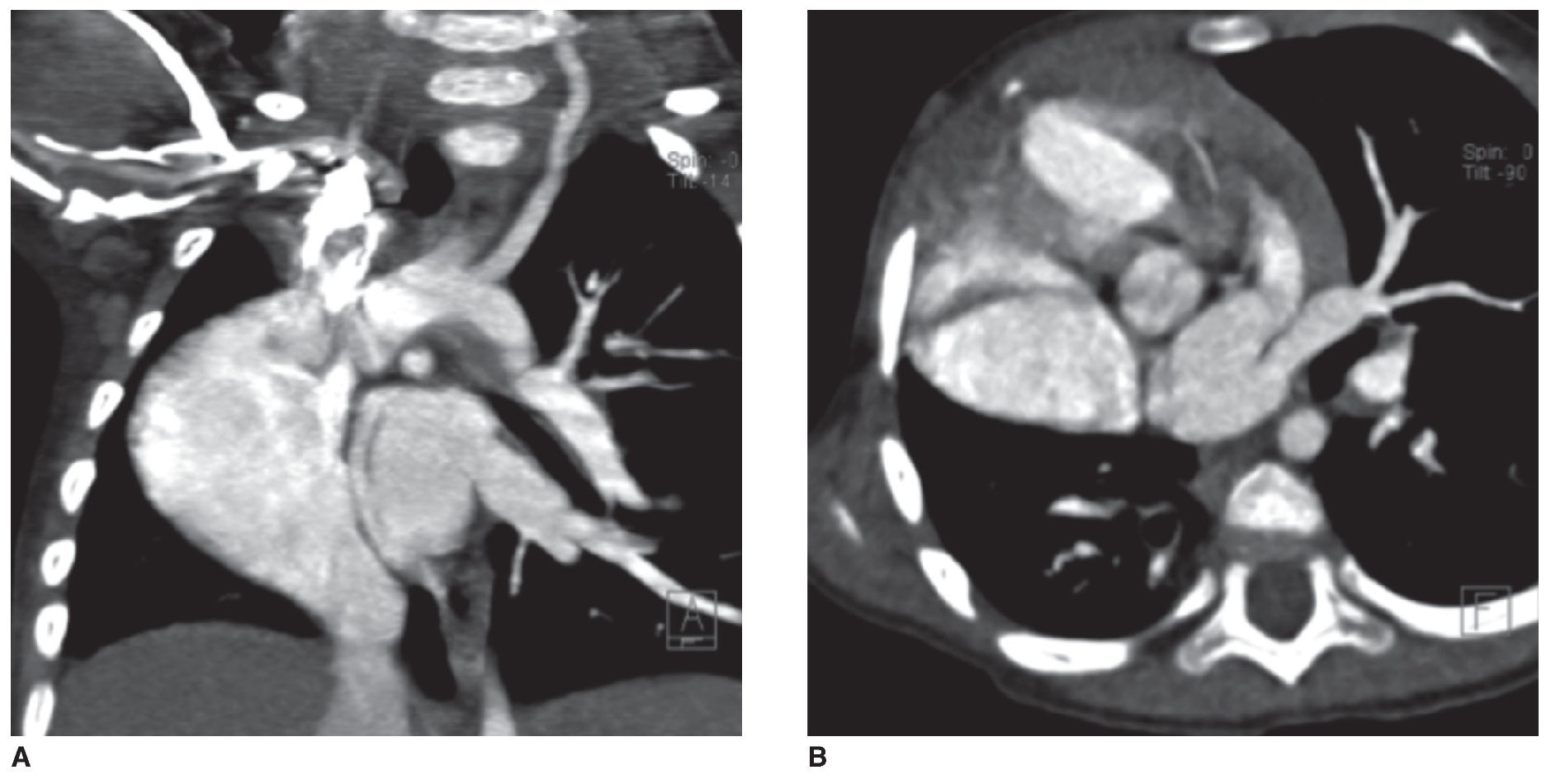
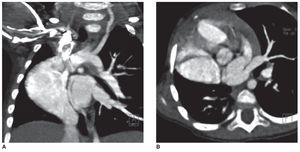
However, in some cases the scimitar sign may be absent, especially in cases with marked hypertrophy of the right atrium or in those associated with dextrocardia and hypoplasia of the right lung. This causes displacement of the mediastinum to the right and to elevation of the diaphragmatic dome (Fig. 2).2,3
Figure 2 Chest tomography. Window for contrasted mediastinum: coronal cut (A) and axial cut (B). Dextrocardia and right lung hypoplasia is observed giving rise to displacement of the mediastinum towards the right and mild elevation of the ipsilateral diaphragmatic dome. At the side of the cardiac silhouette one appreciates an abnormal vascular niche that corresponds to anomalous venous drainage (image corresponding to a female patient 20 months of age).
The scimitar sign is one of the components of the hypogenetic lung syndrome, also known as partial anomalous pulmonary venous drainage or congenital pulmonary venolobar syndrome.1,4,5 It comprises 0.5 to 2% of congenital heart diseases1 and 3 to 5% of the cases of anomalous return of the pulmonary veins. An incidence of 1/3 cases per 100,000 live newborns has been described.6
Although the pathogenesis is unclear, the multiple associated lung malformations seem to suggest an alteration of the development of the pulmonary bud in the early stages of embryogenesis. The reason for its preferential location in the right lung is not known.2 It is frequently associated with hypoplastic right lung and hypoplastic or absent right pulmonary artery.2,3 Tracheobronchial changes, absence of inferior vena cava and accessory drainage may also be present2 as well as lung sequestration with anomalous arterial irrigation of the aorta or one of its branches to the right lung,2,7 septal defects (atrial as well as ventricular), coarctation of the aorta, dextrocardia, tetralogy of Fallot, ductus arteriosus, accessory diaphragm, diaphragmatic eventration or hernia.6 The literature has reported an interatrial communication in 60 to 70% of cases and other congenital heart diseases in19 to 31%.8
The age at the time of the diagnosis is variable. It can be classified as infantile (<1 year of age) or adult (>1 year of age). Occasionally, a third group is classified characterized by the association with complex congenital anomalies that modify the symptoms and the natural history of the syndrome.6,9
The infantile variant has a worse prognosis and more severe symptoms such as shortness of breath, cyanosis, frequent respiratory infections and growth failure. Repeated bouts of bronchitis have even been reported to be associated with bronchiectasis.1,2,6,8
In the adult group with a favorable prognosis, the diagnosis is often incidental. Patients are asymptomatic or present with mild symptoms such as systolic heart murmur, progressive dyspnea or repeated respiratory infections. Clinical follow-up of these patients without invasive diagnostic studies is indicated.2,6,8,9
The association with heart defects presents itself with a 36% frequency in adults and up to 75% in children. The clinical picture depends on the severity of the right pulmonary dysgenesis, recurrent infections, degree of left to right shunt, associated congenital heart diseases and the magnitude of the pulmonary hypertension.6 The association with the latter two increases the risk of congestive heart failure and death.8
In less than 50% of the cases there are symptoms of pulmonary hypertension1 although pulmonary hypertension results in being the most important prognostic factor in the patient’s progress. It may be linked with high resistances in the pulmonary vascular bed (in which the circulation does not adapt itself after birth) and an important short circuit between the abnormal arteries originating in the abdominal aorta, which irrigate the inferior portion of the right lung.8
It is caused by stenosis of the anomalous pulmonary vein (most common), reduction of the right pulmonary vascular bed or increase of pulmonary blood flow due to the existence of associated intracardiac defects.6
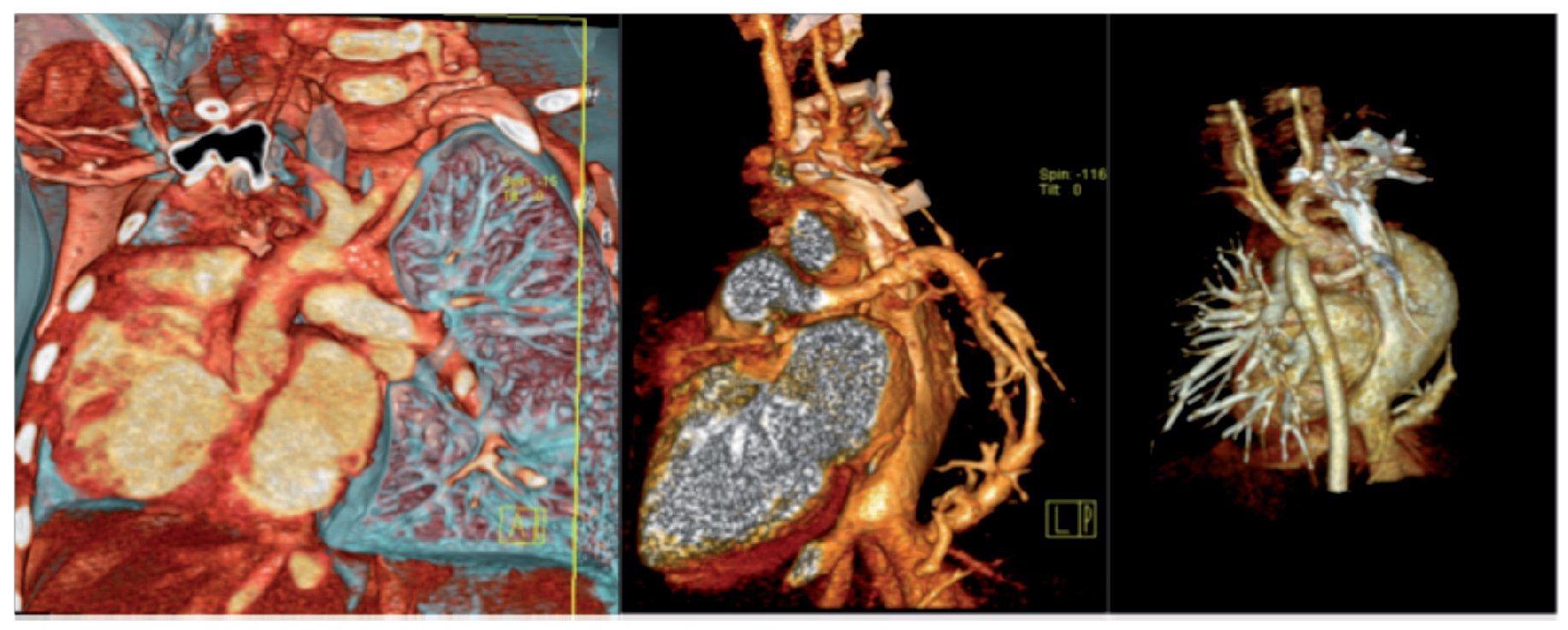
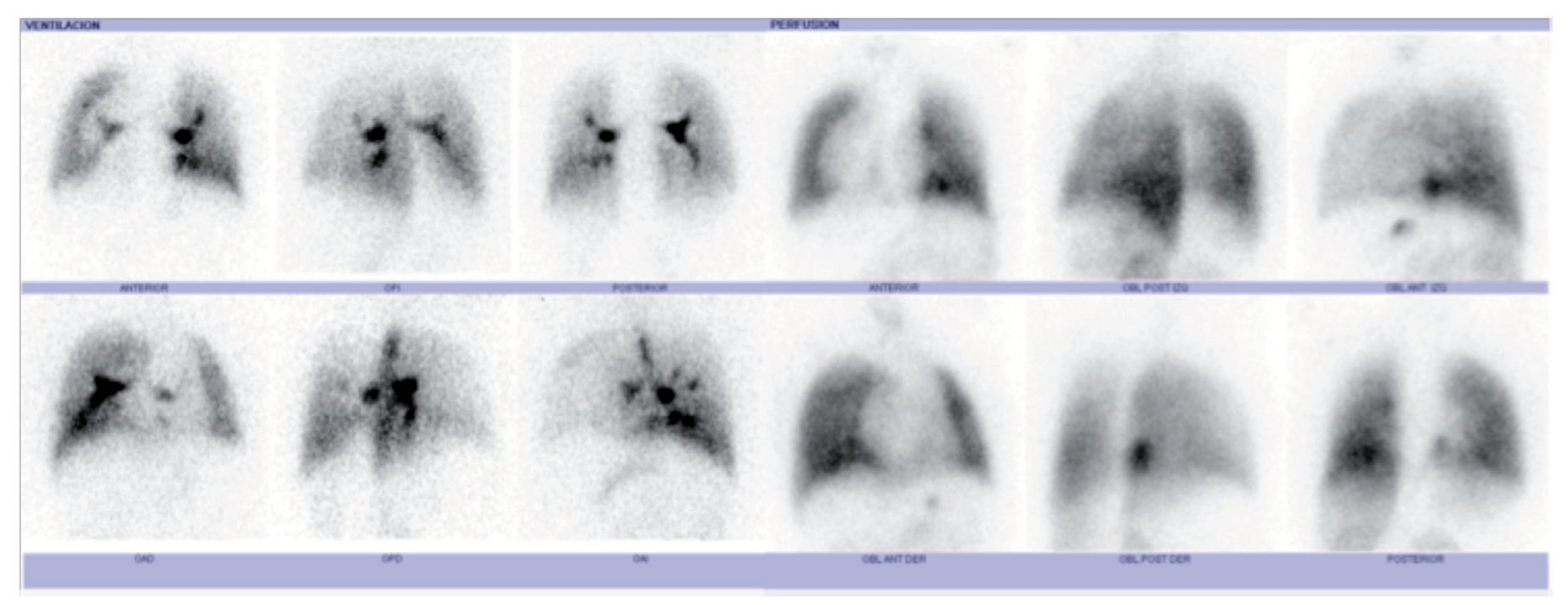
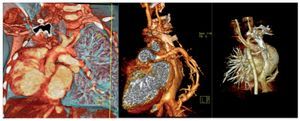
Among the complementary imaging studies, in addition to chest x-ray, are the angiotomographies, which help to detect heart, pulmonary and vascular anomalies (Fig. 3)2; ventilation/perfusion scan, which reports on the characteristics of pulmonary perfusion (Fig. 4); and MRI, adequate for the identification of the collateral aortopulmonary artery and venous anomalies (pulmonary and systemic).6
Figure 3 Angiotomography of the chest with reconstruction technique. Anomalous pulmonary venous drainage is observed (scimitar vein). The study corresponds to the same patient reported in Figure 2.
Figure 4 Lung scan. Decreased right lung ventilation is observed as well as decrease in perfusion in both lungs with right predominance (same patient reported in Figure 1).
Diagnosis may be suspected by fetal echocardiogram. Two-dimensional echocardiogram and color Doppler can evaluate pulmonary pressure, left to right shunt and associated heart diseases. However, cardiac catheterization is considered to be the reference standard to confirm the diagnosis (especially when surgery is indicated), in addition to ruling out associated malformations.6 When clinical symptoms persist or worsen or if there is elevation of the pulmonary artery pressure on indirect determination by two-dimensional echocardiography, angiographic study is recommended.7,8 In the majority of asymptomatic patients, scimitar syndrome is the manifestation of an isolated lesion. Conservative management is recommended as the prognosis is good.2,6 Correction of the associated heart defects may provide a benign evolution comparable with those of the primary isolated forms.8,10
Association with right pulmonary hypoplasia generally has low blood flow; therefore, surgical correction of the anomalous pulmonary venous return should be considered only when the drainage in scimitar syndrome causes considerable pulmonary overload.8
2. Case series
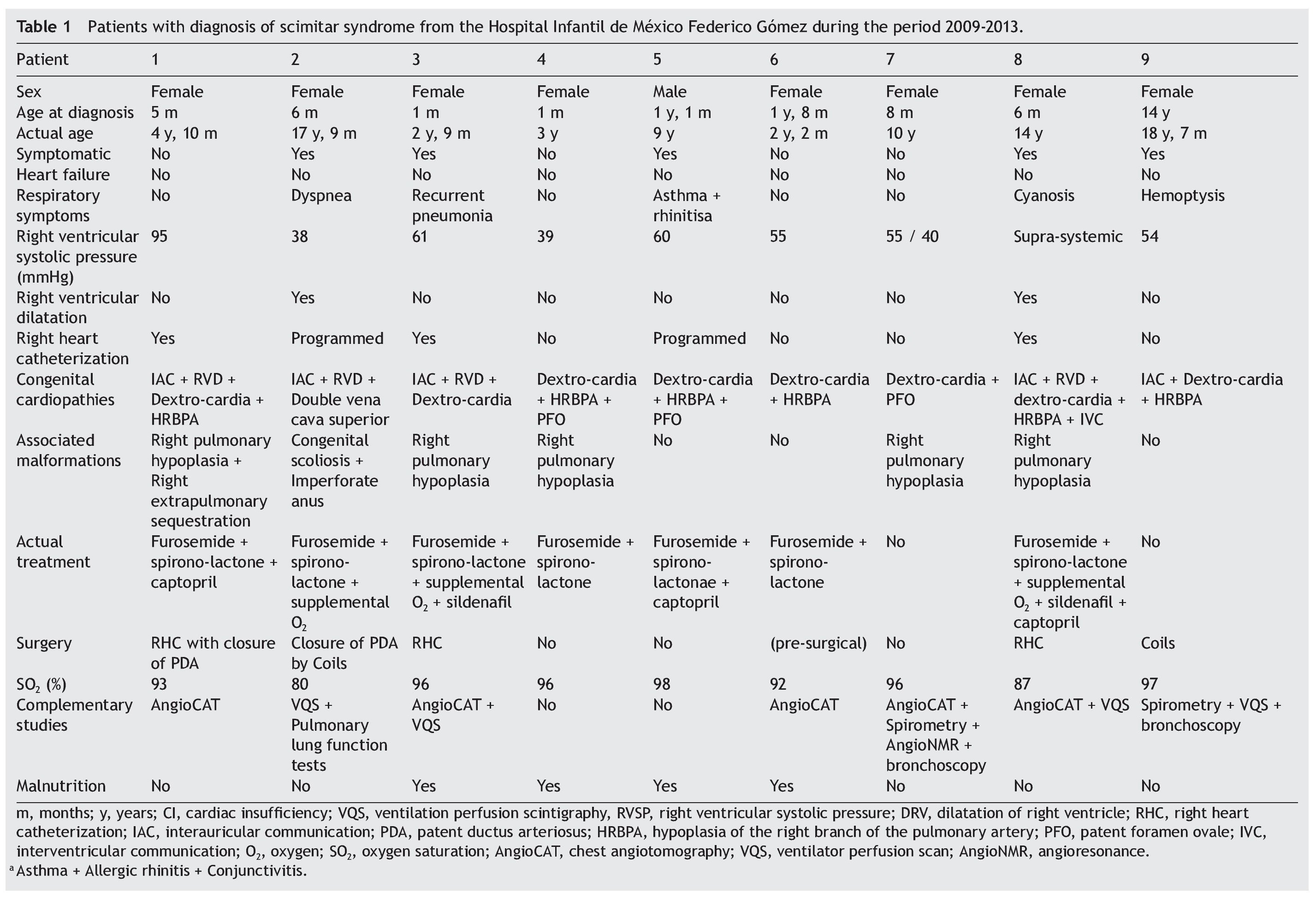
The Hospital Infantil de México Federico Gómez (HIMFG) database for the last 5 years was reviewed. Clinical files of nine patients with diagnosis of scimitar syndrome who had been evaluated during the period from 2009-2013 were found (Table 1). The group had eight female patients with ages between the first month of life and 14 years of age (median of 6 months) at the time of the diagnosis and age from 3 to 18 years (median 9 years) at the time of the study.
The nine patients were reported to be asymptomatic at the time of the last entry on the record. Five patients had a history of respiratory disease (recurrent pneumonia, asthma, hemoptysis, dyspnea) and oxygen saturation reported with a pulse oximetry between 80 and 98% (median 96%) during the last consultation. Four patients had diagnosis of malnutrition.
All patients had an echocardiogram performed. Also, in the last medical note, all were reported to have pulmonary hypertension (with right ventricular systolic pressure of 38 to 95 mmHg). Two patients had right ventricular dilatation and three also had cardiac catheterization performed.
Association with dextrocardia was reported in the group (eight patients), hypoplasia of the right branch of the pulmonary artery (seven patients), right pulmonary hypoplasia (five patients), interatrial communication (five patients), patent ductus arteriosus (four patients), permeable foramen ovale (three patients), lung sequestration (two patients), interventricular communication (one patient), double superior vena cava (one patient), vicariant circulation of the descending aorta to the right lung (one patient), scoliosis (one patient), and imperforate anus (one patient).
At the time of the study, two patients were managed expectantly and the rest were being treated for pulmonary hypertension (diuretic and/or vasodilator). Of these, three were reported to be on supplemental oxygen during their last physician visit, and two had had catheterization (of the three reported with this procedure).
Among the complementary studies performed on this group, the following were reported: angiotomography (five patients), lung scan (four patients), spirometry (three patients), plethysmography (one patient), bronchoscopy (one patient), angioresonance (one patient). Diagnosis was not documented by fetal echocardiogram or with magnetic resonance.
3. Discussion
In the present series of cases seen at the HIMFG, there were differences and similarities observed with what has been reported in the international literature. The group studied was predominantly female with a ratio of 8:1, which differs from what is reported in the literature (1.4:16) and could be attributed to the reduced size of the group.
The average age for the diagnosis reported in the literature is from 7 months.6 Age at the time of diagnosis in these patients had a median of 6 months and was as early as the first day of life and as late as a case diagnosed at the age of 14 years. Therefore, at the time of the diagnosis ages of presentation were shared both in the infantile group (66.6%) as well as the adult group (33.3%).
Although the literature reports that almost half of the patients were asymptomatic,6 the totality of the group was reported to be asymptomatic at the last medical evaluation. There were no deaths reported, even though two-thirds of the group was diagnosed during the pediatric stage and one-third required surgical treatment. Because the study group is affiliated with a third-level hospital, it is impossible to assure that the reason for not finding symptomatic patients was because all had responded adequately to treatment provided or because patients with more severe forms of presentation died before being referred to this type of hospital.
Asthma and hemoptysis were reported within the history of respiratory compromise; the former has not been reported as part of the natural evolution of the disease and the latter has been associated with pulmonary hypertension more than with scimitar syndrome.
All patients in this group had pulmonary hypertension compared with 60% reported in the literature.6 Mild, moderate and severe hypertension was present in equal proportions (three for each group). There were no patients reported with heart failure. The difference in the number of patients with pulmonary hypertension and the absence of heart failure can be associated with congenital heart disease and the size of the sample.
In this group, the association with tracheobronchial disorders, absence of inferior vena cava, aorta coarctation, tetralogy of Fallot, accessory diaphragm, eventration or diaphragmatic hernia was not documented. Incidence of an imperforate anus was reported, a condition which is not routinely reported in the literature to be associated with scimitar syndrome. The patient was also documented with a superior double vena cava and scoliosis (Figs. 1 and 4). The remainder of the associations in our patients coincides with what has been reported.
Although it is an uncommon anomaly, it is important to remember that the diagnostic suspicion is established with a simple chest x-ray (scimitar sign) in patients who range from being asymptomatic to seriously ill.
Conflict of interest
The authors declare no conflict of interest of any nature.
Received 5 January 2015;
accepted 5 January 2015
☆ Please cite this article as: Jaramillo González C, Karam Bechara J, Sáenz Gómez J, Siegert Olivares A, Jamaica Balderas L. Síndrome de la cimitarra: serie de casos. Bol Med Hosp Infant Mex. 2014;71:367-372
* Corresponding author.
E-mail: mipediatrafavorito@yahoo.com (C. Jaramillo González).