Introducción: La toxoplasmosis causada por el Toxoplasma gondii se transmite a los humanos de manera transplacentaria, entre otras. Se estima que infecta a un tercio de la población mundial y está asociado con infección congénita y abortos. Solo son sintomáticos del 10 al 20% de los casos.
Caso clínico: Se presenta el caso de un recién nacido pretérmino referido a un hospital de mayor complejidad. Durante la hospitalización se realiza el diagnóstico de toxoplasmosis congénita con diversas manifestaciones sistémicas.
Conclusiones: La mayor parte de los casos de toxoplasmosis congénita suelen ser asintomáticos. Es necesario realizar pruebas diagnósticas y un examen físico completo ante la sospecha de la infección para detectar tempranamente todas las manifestaciones posibles.
Background: Toxoplasmosis, caused by Toxoplasma gondii, is transmitted to humans in several ways, such as transplacental spread. It is estimated that this parasite infects a third of the world population and it is associated with congenital infection and fetal loss. Only 10 to 20% of the cases are symptomatic.
Case report: We present the case of a pre-term newborn that had been referred to a tertiary care center. During the in-hospital period, diagnosis of congenital toxoplasmosis with many systemic manifestations was performed.
Conclusions: Most cases of congenital toxoplasmosis are asymptomatic. Diagnosis tests and a complete physical examination should be performed on all newborns with suspicion of infection to detect all possible manifestations as in the case reported.
1. Introduction
Toxoplasmosis is caused by Toxoplasma gondii, a protozoan parasite with a complex life cycle with three stages: tachyzoites, bradyzoites and sporozoites.1 Its definitive host is felines, including domestic cats. Transmission takes place in three ways: consumption of infected meat, ingestion of oocysts of cat’s feces, and transplacentally.1 It is estimated to infect a third of the world’s population and is associated with congenital infections and abortions.2
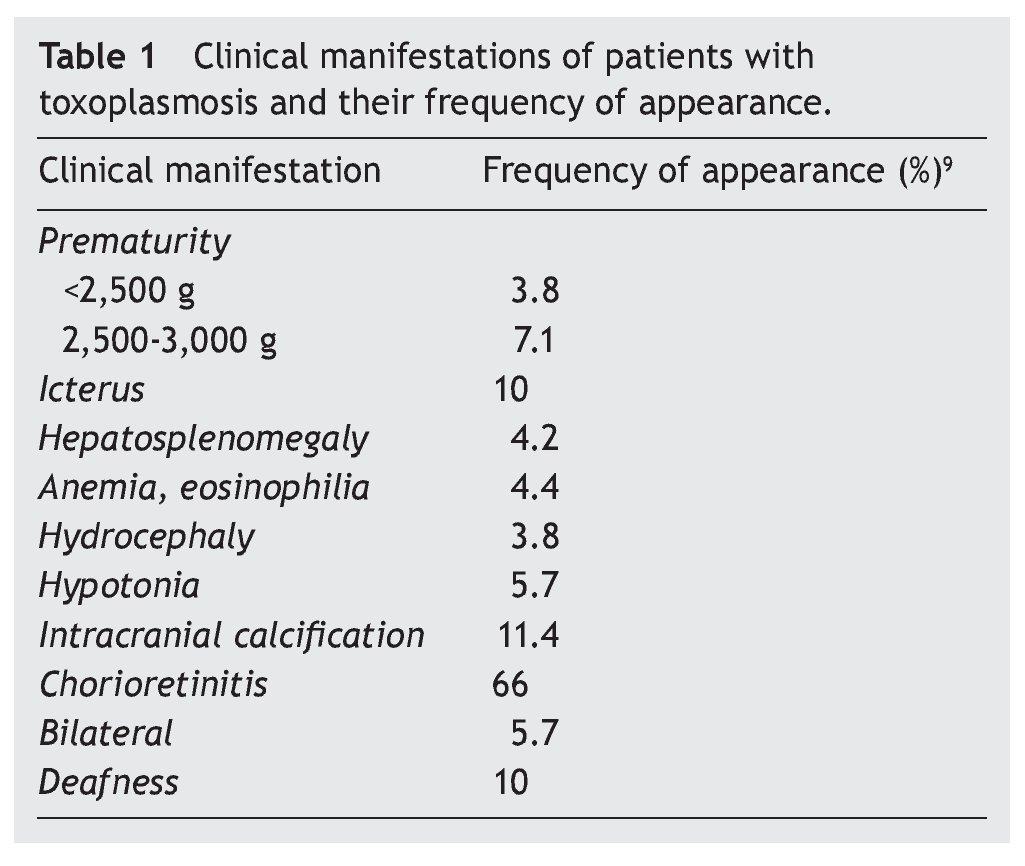
Of the total number of cases, only 10-20% are symptomatic. It is possible that the congenital infection presents itself as a neonatal disease. Symptoms depend on the time in which the infection is acquired, being more severe between 10 and 24 weeks of gestation.2 There is a classic triad of symptoms suggestive of toxoplasmosis. These include chorioretinitis, intracranial calcifications and hydrocephalus.1 Other manifestations include strabismus, blindness, seizures, psychomotor developmental delay, mental retardation, anemia, jaundice, rash and petechiae due to thrombocytopenia, encephalitis, pneumonitis, microcephaly, hepatomegaly, splenomegaly and nonspecific symptoms2,3 (Table 1). Toxoplasmosis is usually diagnosed by antibody detection.3
The objective of this work was to present a case in which the majority of the manifestations reported for toxoplasmosis were observed.
2. Clinical case
A 7-day old newborn was admitted after being transferred from a rural hospital. The patient is the product of a vaginal delivery, preterm at 32 weeks, weight 2,030 g and Apgar scores of 4 and 7. Physical examination found distended globular abdomen, hypotonia, scrotal sac hydrocele, cephalocaudal cyanosis, intercostal retractions and nasal flaring. The mother, 31 years of age, had urinary tract infection during the last trimester of pregnancy, which was treated. There was a history of prenatal care. Ultrasound revealed signs of severe polyhydramnios and fetal ascites.
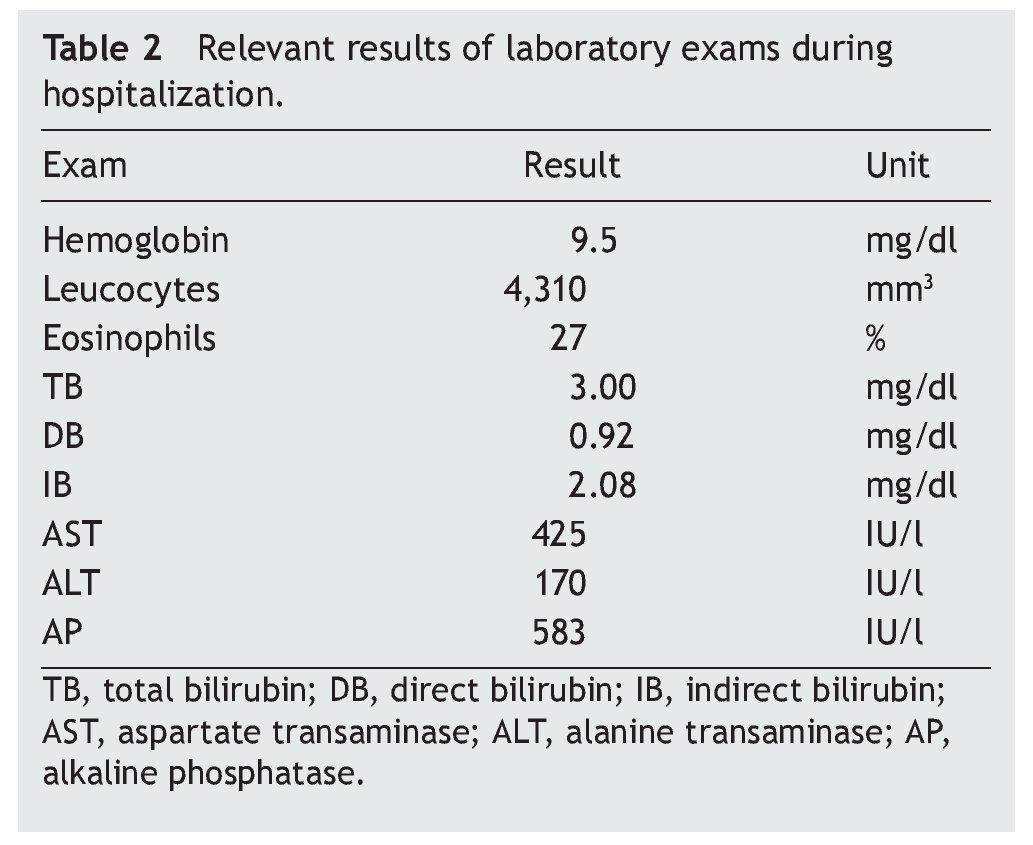
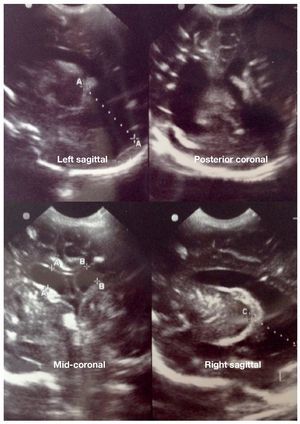
The patient was admitted with the diagnosis of congenital ascites, neonatal icterus and probable sepsis for which antibiotic treatment was given. Complement examinations were negative for neonatal sepsis, including negative Hemoccult. The patient had chorioretinitis and hydrocephaly with parenchymal calcifications (Fig. 1).
Figure 1 Multiple periventricular calcifications and increase in size of ventricles are observed. Severe noncommunicating hydrocephalus and multiple parenchymal calcifications are diagnosed.
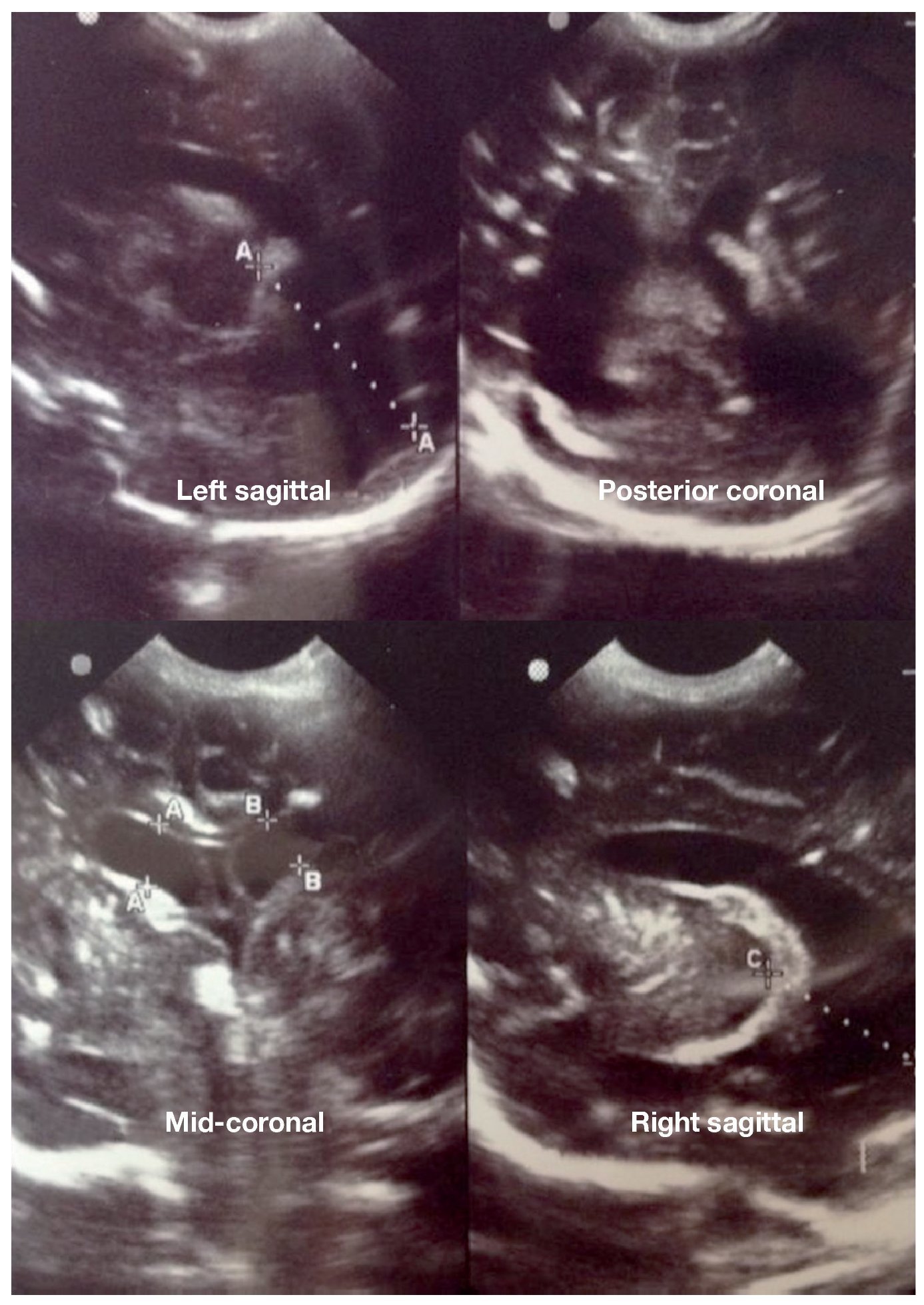
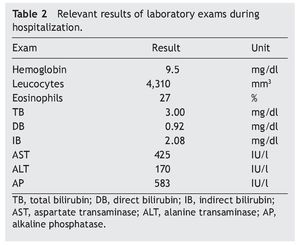
During the patient’s hospitalization, varied results were found for laboratory tests (Table 2). Due to suspected TORCH infection, consultation with the Infectious Disease Department was requested who performed serological tests for cytomegalovirus (CMV) and toxoplasmosis on the patient and the mother. The mother had positive IgG results for CMV and toxoplasmosis, and the patient showed IgM positivity for toxoplasmosis. Other proposed diagnoses were encephalitis, hepatitis, neonatal cholestatic syndrome, pericarditis and peritonitis. At 1 month of age the patient was admitted to the intensive care unit (ICU) due to periods of apnea, fever of 39 oC, desaturation to 77%, marked weight deficit and diabetes insipidus.
The patient was discharged with a diagnosis of systemic toxoplasmosis and being treated with a guarded prognosis.
3. Discussion
Congenital toxoplasmosis is a rare disease in our environment because obligatory screening for TORCH diseases in pregnant patients is carried out.4 The severity of the case will be greater or lesser in accordance with the time in which the disease is acquired during gestation. Generally, the disease has little symptomatology and may in fact be asymptomatic.5 When it exists it is mainly focused on the central nervous system or the retina.1 In toxoplasmosis the classic triad of chorioretinitis, hydrocephalus and intracranial calcifications that occurs in <1/10 cases is described.6 Only few cases present systemic disease.
The case presented is naturally complex because of the number of clinical manifestations observed in the patient. Usually it originates from a maternal infection during the first trimester of pregnancy. The classic triad previously mentioned of hydrocephaly, chorioretinitis and intracranial microcalcifications was present. Also, a variety of symptoms were found that are present in a very limited number of cases such as hepatosplenomegaly and hypotonia. Multiple publications have described different findings and, in many cases, findings that are nonspecific.7,8 In fact, the disease itself could be the cause of the patient’s prematurity.
The prevalence of clinical manifestations in patients with toxoplasmosis may be variable. However, the appearance of icterus, intracranial calcifications, chorioretinitis and hydrocephaly tend to be more common8,9 (Table 1).
It is very important that during the diagnosis other etiologies that could explain the clinical picture be ruled out. As in the case presented, it should be differentiated from other intrauterine infections. Once an early diagnosis is made, timely treatment may be given to decrease possible complications. An evaluation of the mother as well as the child is recommended and should include ophthalmological examination, neurological examination (including cerebrospinal fluid examination) and hearing exam, as well as corresponding serological studies.5,7
Conflict of interest
The authors declare no conflict of interest of any nature.
Acknowledgments
Dr. Yhuri Carreazo Pariasca (Pediatrician) and Dr. Carlos Huertas Félix (Neonatologist).
Received 9 September 2014;
accepted 18 November 2014
☆ Please cite this article as: Beltrán-Flores S, Flores-Arriaga J, Lema-Correa M. Toxoplasmosis congénita. Bol Med Hosp Infant Mex. 2014;71:373-376
* Corresponding author.
E-mail: mlemacorrea@gmail.com (M. Lema-Correa).