1. Summary of the clinical history (A-13-44)
We present the case of an 8-month-old female who was admitted to the Hospital Infantil de Mexico Federico Gomez (HIMFG) due to cough, dermatosis, and fever. The patient was referred from a second-level care pediatric hospital.
1.1. Family history
The patient’s mother was 19 years of age and the father was 20 years of age.
1.2. Social history
Nutrition. The patient was fed breast milk exclusively for 4 months and was weaned at 5 months with whole milk from this age.
Psychomotor development and immunizations. Vaccination profile was incomplete and a delay in psychomotor development was noted.
1.3. Perinatal and pathological history
The patient was hospitalized due to respiratory illness accompanied by nutritional deterioration and skin lesions. During that hospitalization, the patient was transfused with fresh frozen plasma and red blood concentrate.
1.4. Current illness
On arrival to the HIMFG the patient was found to have persistent respiratory symptoms and dermatosis, which was described as pruritic, disseminated to the arms and legs, chest and abdomen, well-defined papules, irregular, reddish to purple in color with necrotic zones.
Physical examination. The patient was pale with evidence of reported skin lesions. Pulmonary fields were hypoventilated with bilateral crepitations. The patient had hepatosplenomegaly and symmetrical edema in both legs. The patient weighed 6 kg with a length of 60 cm. Vital signs demonstrated fever.
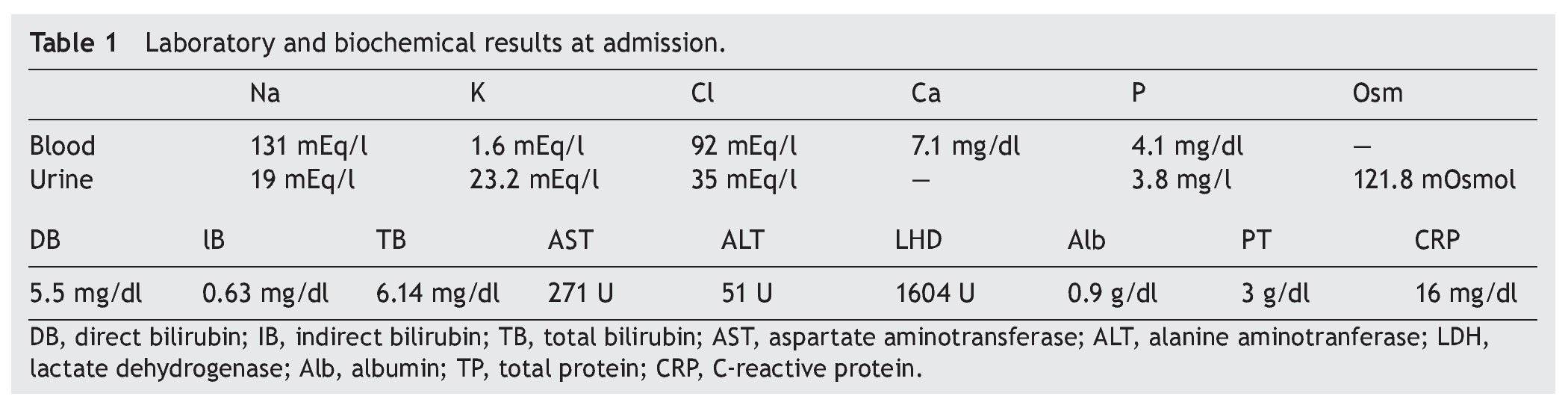
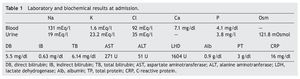
Laboratory and imaging studies. Laboratory results showed anemia (hemoglobin 5.9 g/dl), thrombocytopenia (52,000 platelets), and hypoalbuminemia 0.7 g/dl (Table 1). Coagulation times were prolonged and had electrolyte imbalance. On admission, the patient had elevated nitrogen with elevated creatinine as well as elevation in bilirubin (at the expense of direct bilirubin) and aminotransferasemia.
On admission she had respiratory failure and neurological deterioration, for which she required endotracheal intubation. A central venous catheter was placed for invasive monitoring. She was managed with vasoactive amines and base solutions and also required acute potassium correction.
Cardiology. The heart was structurally healthy with adequate right ventricular pressure and left ejection fraction of 60%.
Infectious disease. There was probable noninfectious vasculitis associated with leukocytosis, thrombocytopenia, anemia and coagulation disorder. Also found were toxic granulation and vacuolization of neutrophils for which cefepime and vancomycin were given.
Intensive care. Low cardiac output data were found for which vasopressor treatment with adrenaline, milrinone, norepinephrine and vasopressin was added. Taking into consideration shock refractory to catecholamines, hydrocortisone was started. Similarly, fluids, albumin and furosemide infusions were restricted. Ventilatory parameters increasingly required more pressure and volume.
During the patient’s evolution a left pleural effusion was found with bilateral alveolar infiltrate on x-rays. Thoracentesis was carried out, obtaining 50 mL of pale yellow fluid with exudative characteristics. From this point she required high-frequency ventilation to achieve normoxemia and normocapnia. No invasive cells were found in the fluid.
On her last day of life, the patient showed data of persistent anemia, thrombocytopenia, failure of coagulation times, hypofibrinogenemia, and bleeding at puncture sites. At this point she required transfusion of plasma, cryoprecipitates and erythrocyte concentrate. Despite these measures, the patient showed decompensated lactic acidosis with preserved anion gap. In addition, hyperglycemia was found and rapid insulin in microdoses was administered. She was also administered gamma globulin in a single dose. Hypokalemia observed at this point already had electrocardiographic impact.
The Department of Pediatric Surgery reported the patient to have ascites and abdominal hypertension requiring paracentesis; 2 mL of serous fluid was obtained. The Infectious Disease Department decided to change cefepime for carbapenem because of the history of prior management and to add amphotericin B lipid complex. A positive mannan antigen for Candida was found (negative for Aspergillus). Blood cultures were positive for Gram positive cocci.
The patient presented progressive deterioration with hypotension, bradycardia, oxygen desaturation and, finally, cardiorespiratory arrest unresponsive to advanced resuscitation maneuvers.
2. Case presentation
2.1. Coordinator (Dr. Salvador Villalpando Carrión)
This is a case that is increasingly more difficult to discuss because of the epidemiological and nutritional transition that our country is experiencing; therefore, it has much interest and clinical relevance.
2.2. Imaging (Dr. Bertha Lilia Romero Baizabal)
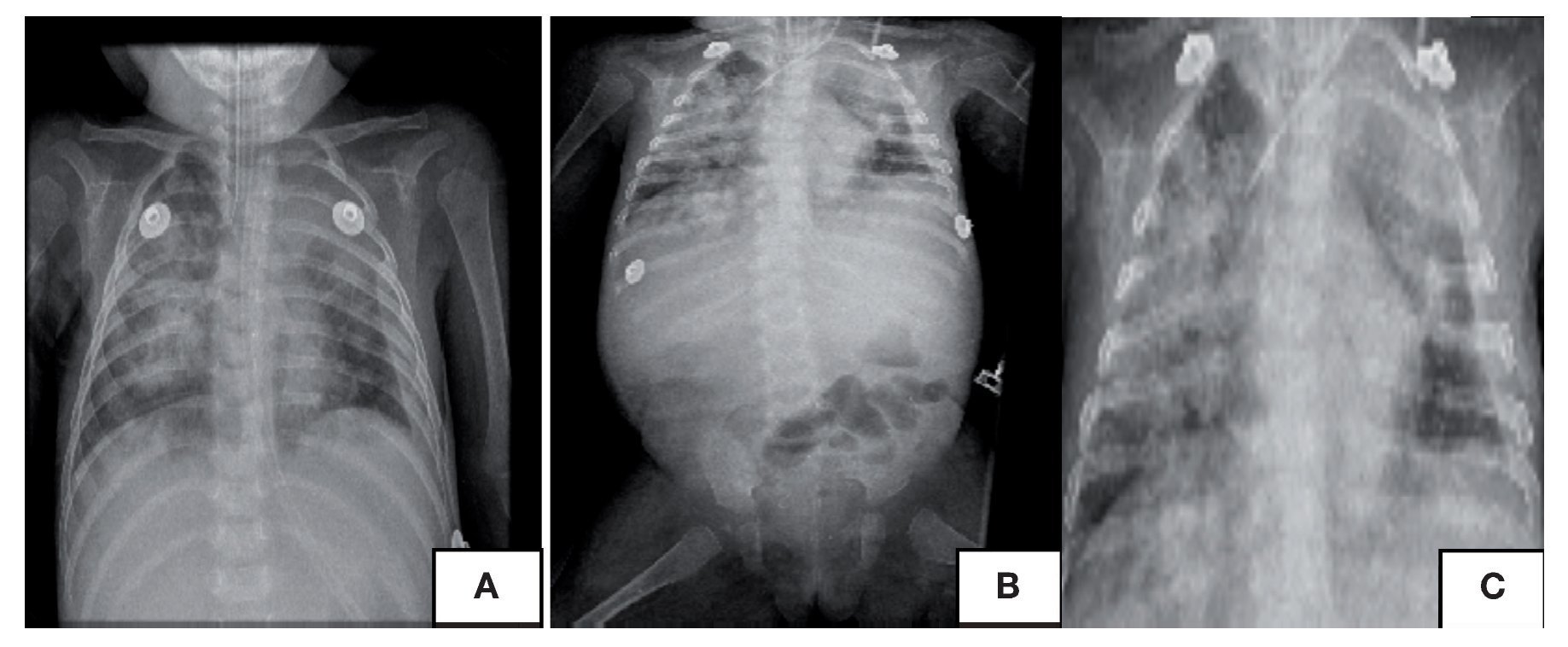
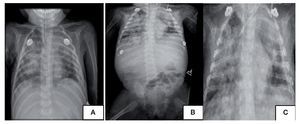
Radiological findings of the patient at only 48 h of hospitalization are shown. The first image is an AP view of the chest where a mixed infiltrate is observed, which does not allow for the cardiac silhouette on the right side to be clearly appreciated. The left side is appreciated, whereas on the right there is a completely complex infiltrate. Within this radiopaque infiltrate, discrete radiolucent images are also observed that probably translate to more severe lung damage. Towards the left side, in the apical region, a radiopaque image is seen suggestive of atelectasis. An endotracheal cannula is seen and the cardiophrenic and diaphragmatic angles are apparently preserved (Fig. 1A). The mentioned image was from the same day but at a different time. Greater radiopacity is observed at the left apical region. The cannula is noted to be higher and a catheter is identified, apparently jugular, from the left side that extends to the junction of the innominate vein with the superior vena cava. Abdominally, an intestinal gas pattern is notable, which is found displaced towards the pelvic region, iliac fossa and left flank. Also seen is an important decrease in bone density with thin cortical zones and widened medullary zones. This image shows radiolucent lesions within this infiltrate so that the possibility of important pulmonary destruction is not ruled out radiologically (Fig. 1B). The following image was taken moments before death. The cardiac silhouette is not able to be seen. The image suggests a probe in the esophagus and another over the trachea. A catheter is seen with its distal end at the junction of the right atrium with the inferior vena cava (Fig. 1C). The abdominal radiopacity we mentioned suggests an important liver growth. Radiological diagnoses are as follows:
Figure 1 Antero-posterior (AP) x-rays of the chest taken at different times. (A) Mixed infiltrate. (B) Greater radiopacity at the left apex and intestinal gas pattern as well as substantial reduction of bone density. (C) The cardiac silhouette is not shown.
• Mixed pulmonary pattern suggesting a complicated pneumonic process with probable lung destruction. However, the possibility of hemorrhage is not radiologically ruled out because of the infiltrate that is seen
• Hepatomegaly
• Osteopenia
2.3. Coordinator (Dr. Salvador Villalpando Carrión)
Due to the efforts from the Division of Auxilliary Services, we obtained information in a late manner which, unfortunately, was not recorded in the medical record. It is the result of two cultures taken just before the arrest, with a difference of 5 min. One was positive for Pseudomonas aeruginosa and the other for Stenotrophomonas maltophilia with Enterococcus faecalis.
3. Discussion (Dr. José Guadalupe Jaramillo Alvarado)
This is the case of an 8-month-old female infant admitted to the HIMFG for the first time 1 day before her death. She was previously hospitalized for 16 days in a second-level care hospital due to cough, kwashiorkor type malnutrition, purpura, dermatosis and fever. She was referred to the HIMFG because of vascular collapse and neurological deterioration. The following syndromatic diagnoses were made:
1. Respiratory infection syndrome based on cough with dyspnea and emesis, fever, pulmonary hypoventilation, crepitant rales, hypoxemia, fever, leukocytosis and bandemia.
2. Respiratory failure syndrome based on agonal respiration, hypoxemia, and neurological deterioration.
3. Purpuric syndrome based on skin lesions, paleness, petechiae, bleeding, prolonged coagulation times, thrombocytopenia and anemia.
4. Uremic syndrome based on elevation of urea nitrogen, elevation of creatinine and metabolic acidosis.
5. Psychomotor delay syndrome based on low caloric intake and neurological milestone delays such as being able to support her head at 6 months and inability to sit upright.
In agreement with the syndromatic diagnoses, the following medical diagnoses are made:
a. Multiple organ dysfunction syndrome based on respiratory, neurological, hematological, renal and hepatic insufficiency.
b. Fulminating purpura based on the purpuric syndrome, which generalizes and becomes petechial as well as the rapid progression or vascular collapse with low antithrombin.
c. Severe malnutrition based on low weight, edema and hypoalbuminemia.
d. Refractory septic shock based on upper respiratory infection syndrome and respiratory failure syndrome, systemic inflammatory response syndrome and multiple organ dysfunction unresponsive to inotropes.
Among the purpuric-petechial exanthems and vasculitis are fulminant purpura, septic shock syndrome and dengue. Because of the clinical form of presentation, it could be fulminant purpura due to the rapid progression to vascular collapse. The toxic appearance, with unstable vital signs, petechiae, purpura and fever could make one consider an invasive disease due to meningococcus, pneumococcus or Haemophilus influenzae, which present clinical pictures similar to fulminating purpura. The patient met the criteria for fulminant purpura:
i) Age between 0 and 14 years
ii) Process preceded by a banal infection
iii) Bleeding
iv) Abnormalities compatible with disseminated intravascular coagulopathy (DIC)
v) Capillary thrombosis of the affected sites
In order to detect an etiological agent, Gram stain of the skin lesions would have been advisable where the sensitivity is 72% compared with 22% for cerebrospinal fluid (CSF). Only a smear with toxic granulation and vacuolization of neutrophils is reported, which are observed in acute, mostly bacterial, infectious states such as the ones the patient may have presented.
Poor prognostic factors for the patient were immuno-compromise due to malnutrition, shock, coma, ecchymotic purpura, leukopenia, thrombocytopenia and low fibrinogen. According to the described clinical evolution, she apparently began with an upper airway infection. Subsequently, a bacterial infection was added. This has been noted in 25-30% of patients who develop bronchopneumonia. With respect to the pyuria, it is not reported in the clinical history or in the urinalysis, which would point to a urinary tract infection.
With regard to nutritional status, the expected weight for the patient’s age was 8,310 kg and the patient weighed 6 kg at the time of admission. Knowing that the weight is unable to be evaluated due to the edema and visceromegaly, malnutrition is classified as severe in all patients with edema and classified as kwashiorkor.
The mortality risk increases as the degree of malnutrition is high, with the weight for age and measurement of the mid-arm circumference better correlated. The cause of the malnutrition could be low caloric intake because the requirements for age were 120 kcal/kg/day and the patient received 75 kcal/kg/day. Also, the patient was given whole milk, with greater protein content, causing a greater solute load. Therefore, if the infant did not receive an adequate amount of fluids, dehydration would be the result, as in this case.
The deficiency of essential fatty acids, biotin, zinc, niacin, vitamins A, C, E, K, riboflavin, pyridoxine, folic acid, vitamin B12, and iron may cause generalized dermatitis, petechiae, purpuric lesions, and bruising, such as that presented by the patient. This is similar to “purpura of the malnourished” described by Dorantes et al. in the HIMFG>50 years ago.1
Hypokalemia could have been secondary to the malnutrition itself because of the chronic lack of nutrients, which was perpetuated with the use of medications such as insulin, diuretics and amphotericin. In short, the patient was admitted to the HIMFG 1 day before her death, with severe malnutrition, multiorgan failure based on renal, neurological, and hematological parameters, liver failure with hemodynamic instability probably due to an infectious cause, without response to inotropes or antibiotics, resulting in cardiorespiratory arrest.2-7
Final diagnoses
• Fulminating purpura
• Kwashiorkor malnutrition
• Bronchopneumonia
• Psychomotor delay
• Refractory septic shock
• Multiorgan failure
Probable cause of death
¿ Refractory septic shock
¿ Multiorgan failure
3.1. Evaluation and analysis of medications (Dr. Luis Jasso Gutiérrez)
As far as the history and what it mentioned about meningococcemia, it should not have been ignored. On the other hand, it is difficult to understand that the patient had kwashiorkor malnutrition as she was being fed maternal breast milk, at least during the first 4 months of life.
3.2. Pediatric Gastroenterology and Nutrition (Dr. José Guadalupe Jaramillo Alvarado)
With regard to the malnutrition, although she was breast fed for 4 months, one must consider that the mother, 19 years of age, fed her whole milk from the age of 4 months. This caloric intake could have caused the malnutrition. With regard to the etiology, the patient had a rapid and progressive vascular collapse. One the causes of fulminant purpura is meningococcus, but one cannot rule out pneumococcus or Haemophilus influenzae.8-11
She must also be considered as a patient with severe malnutrition from the moment she presented edema. It is necessary to manage the nutrition and caloric intake that infants receive from day to day and also control electrolytes, otherwise they can cause a retrograde syndrome and leading to death due to cardiac insufficiency.
3.3. General Directorate (Dr. José Alberto García Aranda)
Although there is insistence that it is kwashiorkor, one must take into consideration that this patient died 1 day after being admitted to the HIMFG. There was not sufficient time to develop cardiac insufficiency, which is the principal cause of death in children with kwashiorkor. The diagnosis does not coincide, but the comments from pathology are awaited to clarify this issue.
3.4. Gastroenterology (Dr. Liliana Worona Dibner)
This clinical picture is similar to that of a patient with cystic fibrosis fed exclusively breast milk and with a tendency for hypoalbuminemia and edema. The association with the pulmonary problems this patient had suggests this diagnosis. The clinical history does not describe prior respiratory problems and only makes reference to the latest respiratory problem she had. Perhaps this is a secondary malnutrition as an underlying condition. One ought to consider, among the differential diagnoses, cystic fibrosis.
4. Pathology (Dr. María Argelia Escobar Sánchez)
The outer habitus of the child is shown. Skin lesions are immediately noted. Her weight was 6 kg vs. 8.3 kg expected weight; length was 60 cm vs. 70 cm expected for age. The skin lesions, mainly localized in the extremities and the abdomen, are purpuric, but she also had lesions with loss of skin and an eschar in the sacrum. Another notable situation was the presence of edema at the level of the facies, extremities and genitalia (Fig. 2).
Figure 2 Photograph of the exterior habitus of the patient, with weight of 6000 g vs. 8200 g and numerous purpuric and necrotic skin lesions.
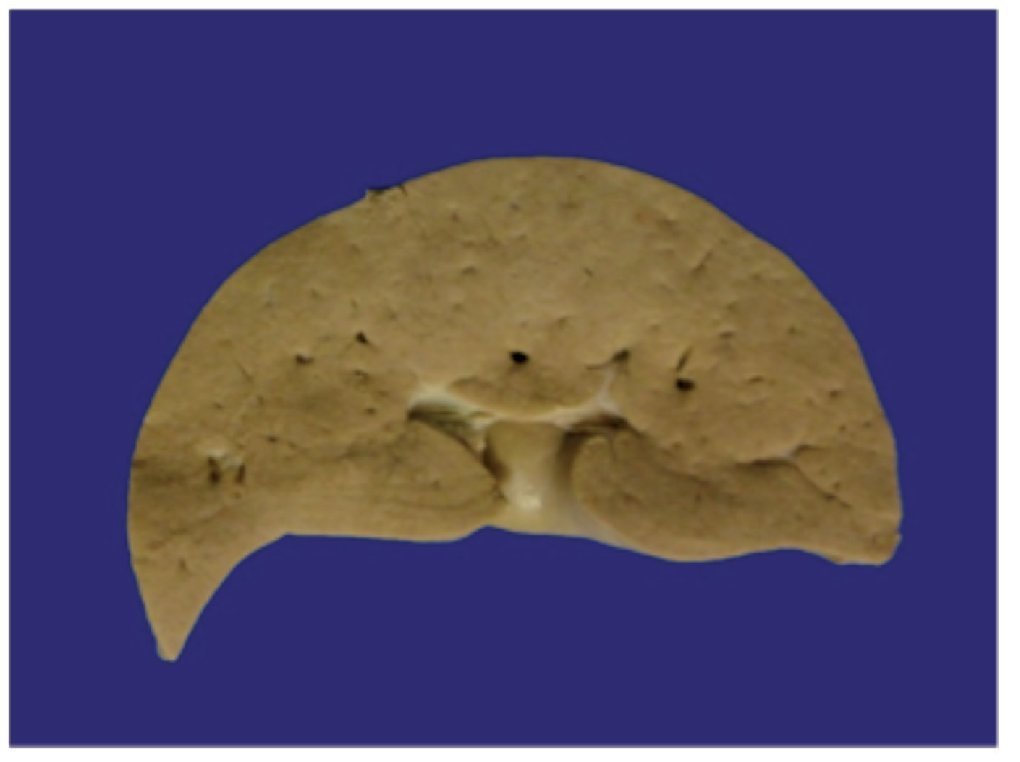
There were 60 mL of fluid obtained from the peritoneal cavity. There was no fluid in the pleural or pericardial cavities. The liver occupied almost the entirety of the abdominal cavity (there was also dilation of some of bowel loops). The liver weighed 350 g vs. an expected weight of 250 g and was yellowish-brown in color. It could be folded onto itself, which translates to the amount of steatosis present (Fig. 3).
Figure 3 Macroscopic photograph of the liver that is noted to be yellowish-brown in color.
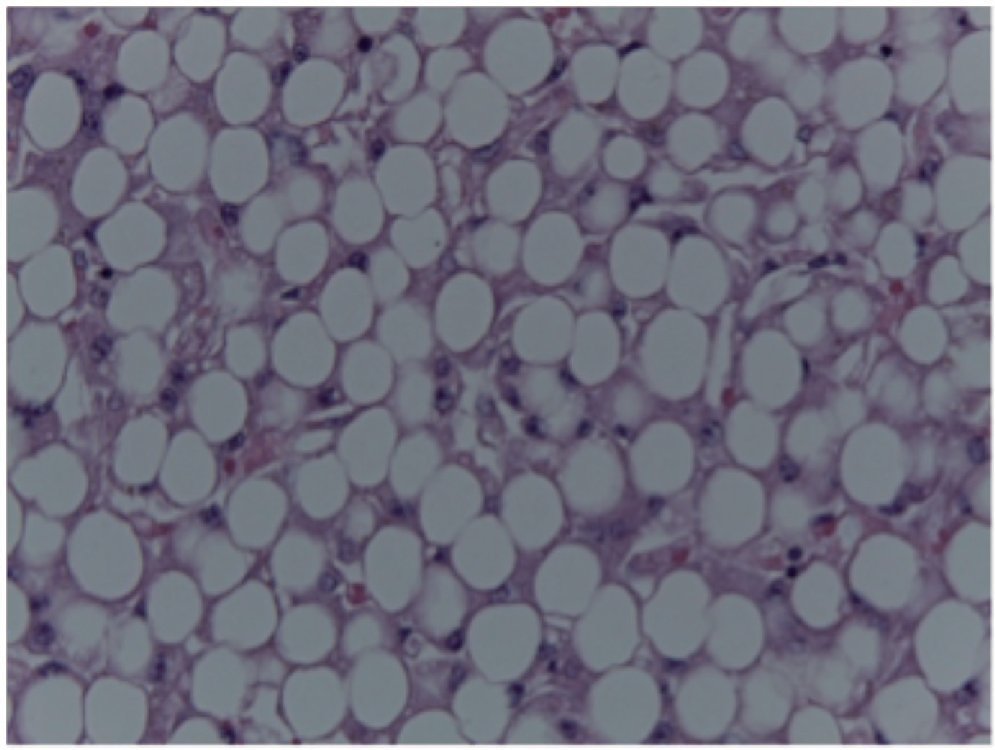
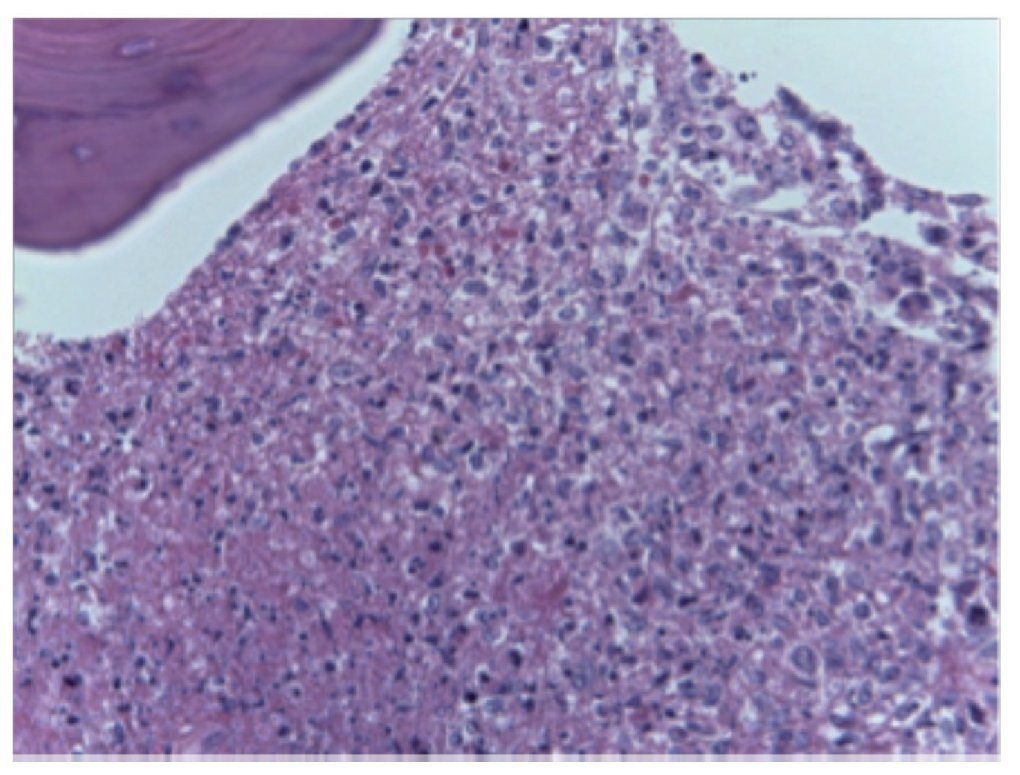
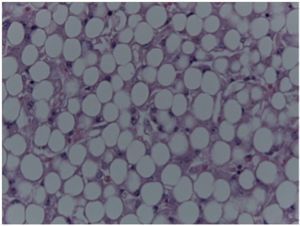
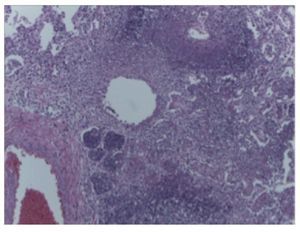
Histological cuts showed a fatty liver. There were two porta spaces seen. Between these spaces, transformation to panlobular macrovesicular steatosis was seen practically in 100% of the liver parenchyma. Transformation to fatty liver is a rarely seen condition. We can see this condition mainly in malnutrition, in alcoholic steatosis, and in some metabolic diseases due to fatty acid storage. However, ultra-structure studies were done and no alteration was found that would suggest a metabolic disease of fatty acids that could cause steatosis of this magnitude.
The presence of steatosis associated with malnutrition, edema and alterations that were found in all the organs appear to be secondary to kwashiorkor type malnutrition. In this case the histological image is completely compatible with this type of malnutrition in contrast to marasmus-type malnutrition in which the main characteristic is loss of muscle mass. In kwashiorkor type malnutrition there is important visceral involvement and lymph depletion that causes secondary immunosuppression.
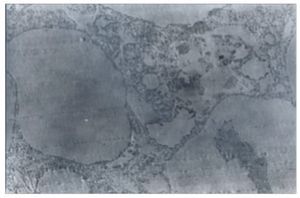
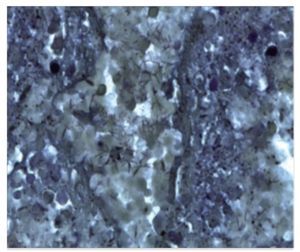
In another photograph, the porta space can be seen, which did not present alterations, and again steatosis with practically no healthy hepatocytes (Fig. 4). Numerous cuts were done to see the ultrastructure. Only the presence of steatosis was noted. There was no other change that would suggest another type of pathology (Fig. 5). Based on clinical history, weight, edema, hypoalbuminemia and liver changes, the following were considered:
Figure 4 Panlobular macrovesicular steatosis. Fatty liver (HE x40).
Figure 5 Ultrastructure that shows steatosis (x50).
Principal diagnosis
• Acute severe malnutrition (kwashiorkor type) (6000 g vs. 8200 g)
Concomitant disorders
• Hepatomegaly (350 g vs. 250 g)
• Panlobular macrovesicular steatosis that affected 100% of the liver parenchyma (fatty liver)
On the other hand, it may be that this malnutrition has conditioned a secondary immunodeficiency. For this reason, the patient presented infectious lesions at the pulmonary level.
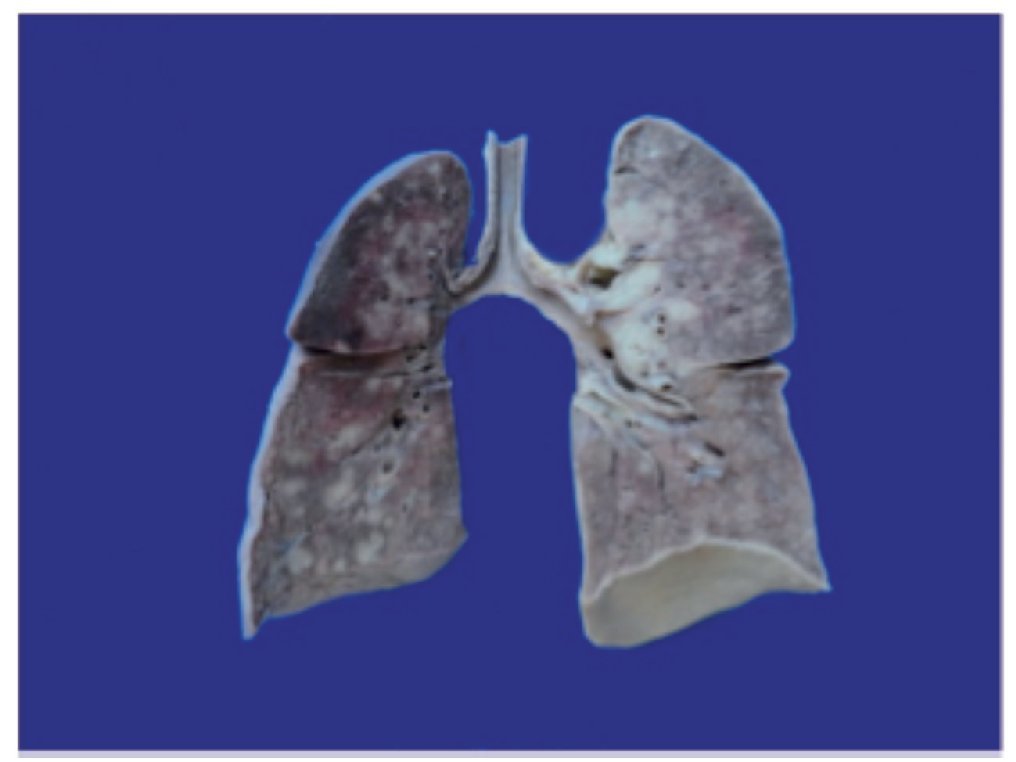
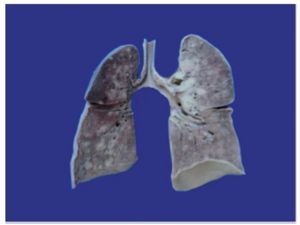
The tracheal cut showed loss of epithelium, i.e., acute ulcerated tracheitis. The lungs weighed 140 g vs. an expected weight of 110 g. Hemorrhagic areas can be appreciated on the pleural surface, especially in the upper lobe, and nodular lesions in both lungs. At the cut it was noted that the parenchyma had been substituted by hemorrhage and by these nodular lesions that on average measured 1 cm in diameter (Fig. 6).
Figure 6 Macroscopic photograph that shows the cut surface of the lungs with extensive areas of congestion, predominantly of the upper lobe of the left lung and multiple nodular lesions that on average measure 1 cm in diameter.
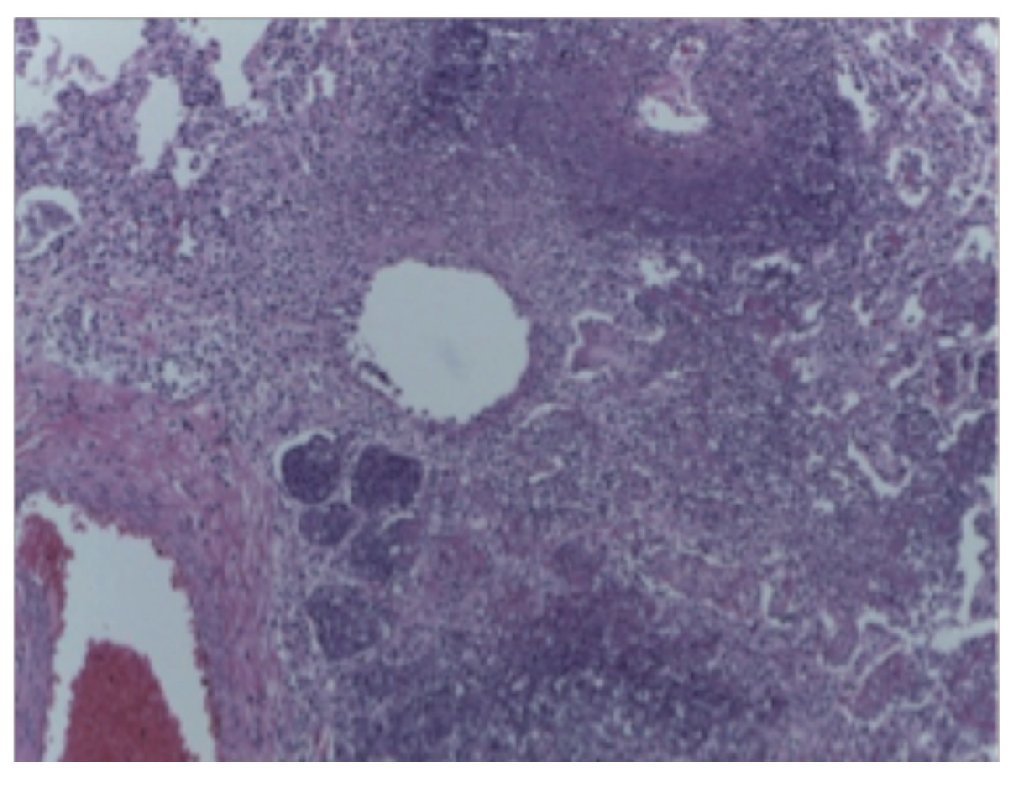
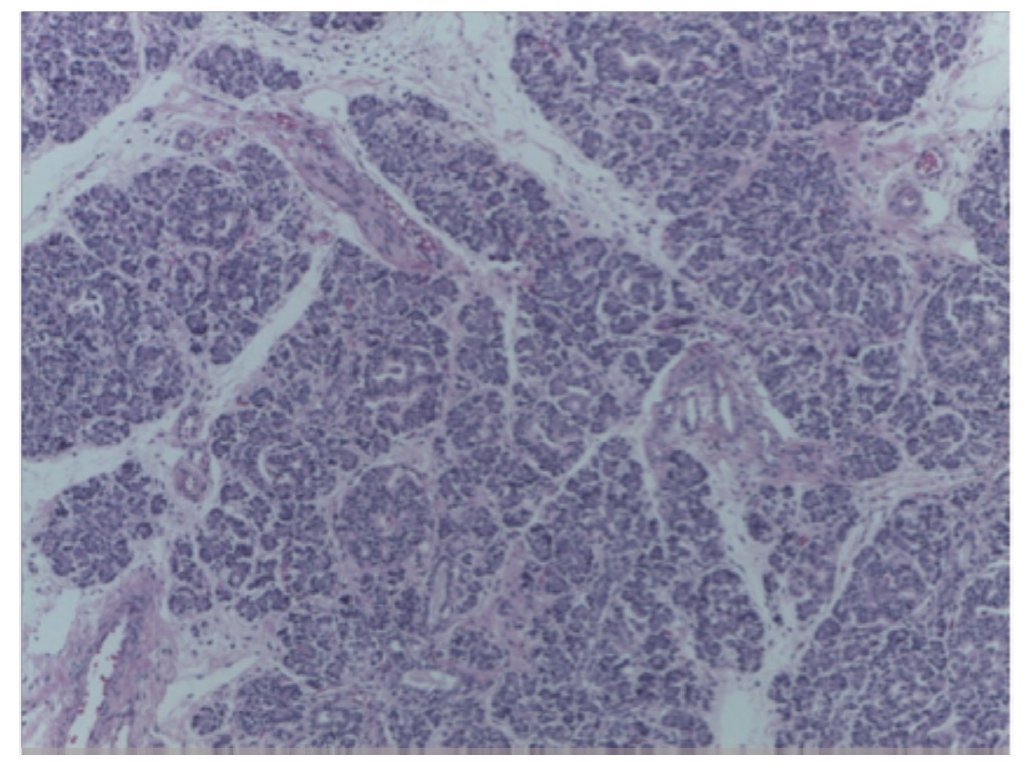
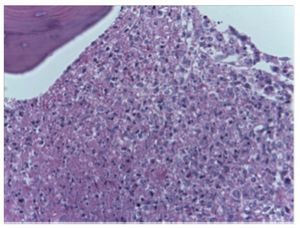
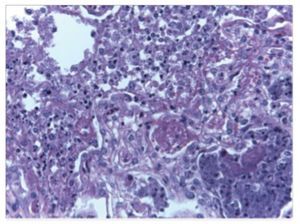
Lung cuts showed the pleura with extensive inflammatory infiltrates comprised of neutrophils. There were also lymphocytes, suggestive of an infectious process of the lungs. The five pulmonary lobes were found to be totally affected and had an extensive basophilic type necrosis affecting the alveoli and also the vascular walls. This is one of the lesions characteristic of Gram negative bacterial infections. Klebsiella pneumoniae and Pseudomonas aeruginosa were isolated in postmortem cultures, which relates to a basophilic or dirty necrosis. At a higher intensification one can see the vascular lesion and, in contrast to a vasculitis associated with an autoimmune process, there is no inflammatory infiltrate in the wall. Only a coagulative (not fibrinoid) necrosis is seen (Fig. 7).
Figure 7 Lung parenchyma with extensive basophilic necrosis (HE x20).
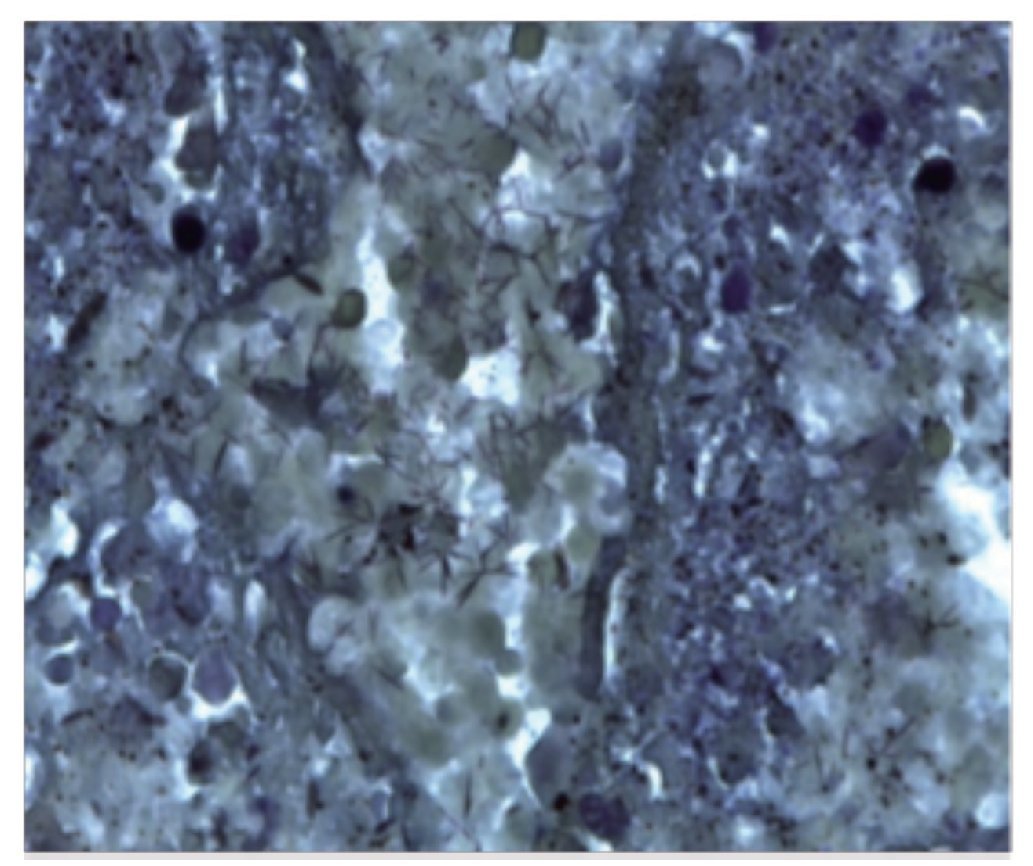
A number of special stains were done because in some of the alveoli a foamy infiltrate suggestive of an infection by Pneumocystis jirovecci was seen. PAS and Grocott stains were done in which no fungi or parasites were found, only bacteria. Numerous cocci and bacilli bacterial colonies were observed in the Gram stain (Fig. 8).
Figure 8 Bacterial colonies (Gram x40).
The ultrastructure was examined, looking for viral inclusions that may not have been seen due to the necrosis; however, only bare nuclei were seen. PCR was done on the pulmonary parenchyma (in the clinical laboratory) and no viral infection was confirmed. With these findings the following concomitant diagnoses were made:
• Necrotizing pneumonia due to Gram negative and positive bacteria
• Acute fibrinopurulent pleuritis
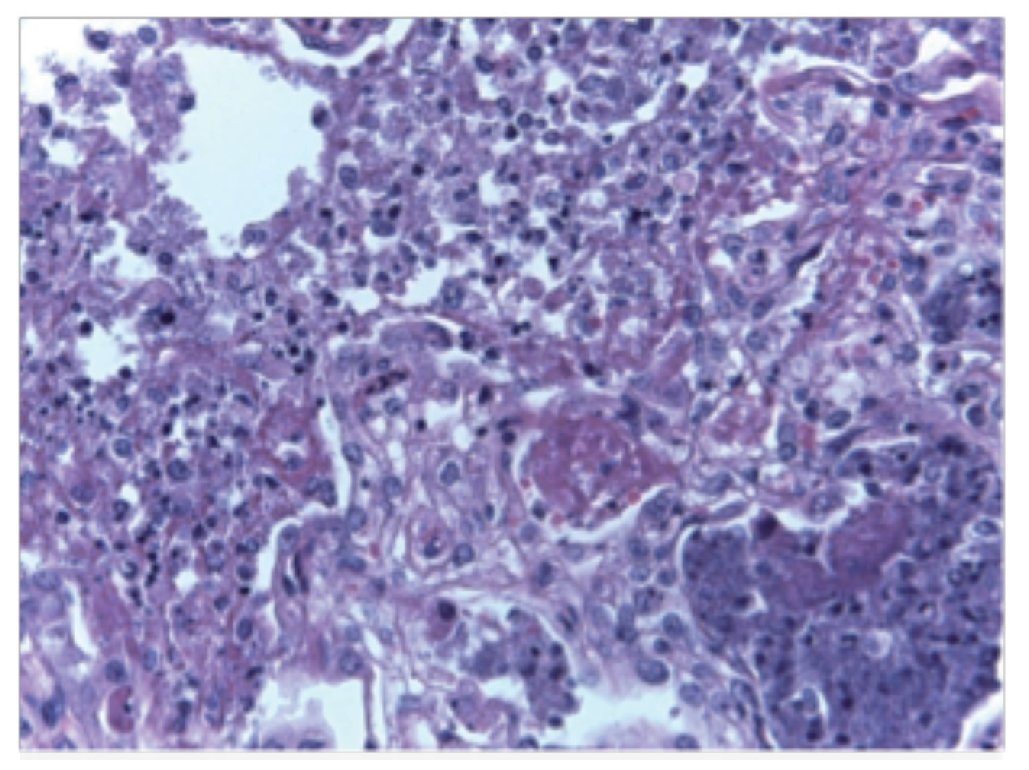
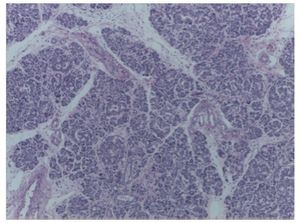
As previously mentioned, it was believed that this patient was immunocompromised. Figure 9 shows a cut of the bone marrow, which confirms that the patient had osteopenia.
Figure 9 Necrosis of the bone marrow stroma (HE x20).
Very thinned trabecula and cavities with ~90% cellularity are seen. The presence of bone marrow stroma necrosis is notable, which is secondary to bone marrow shock. In the better preserved areas, erythroid precursors and some myeloid elements with arrest in the maturation were observed, i.e., myelodysplasia secondary to the infectious process. Lymph nodes showed lymphoid depletion. The secondary lymphoid follicles are not able to be seen, which should have been present in the cortex; however, areas of necrosis secondary to shock are seen. The presence of some residual follicles in the cortex was more evident in the immunohistochemical stains. The expression of CD20 was seen, which are B lymphocytes. In the paracortex, which is the zone of T lymphocytes, expression of CD3 and CD4 is seen.
Within the organs of the mononuclear phagocyte system, the spleen weighed 40 g vs. an expected 30 g. Macroscopically it showed no alterations and microscopically also showed decrease in the lymphoid tissue of the white pulp.
The thymus showed acute involution and dilatation of the corpuscles of Hassall in addition to the presence of some hemosiderophages and decrease in cortical lymphocytes.
Based on these findings the following diagnoses were made:
• Ischemic necrosis of the bone marrow and myelodysplasia
• Ischemic necrosis of the lymph nodes with lymphoid depletion
• Congestive splenomegaly (40 g vs. 30 g) with lymphoid depletion
• Acute involution of the thymus
The following findings were made in the remainder of the organs. Edema was noted in the stomach and esophageal mucosa. Macroscopically the pancreas did not show any changes. Histologically, the esophageal mucosa was integral and there was congestion of the submucosal vessels.
The gastric mucosa was also integral and there was vascular congestion in the submucosa. The cuts of the small intestine at different levels showed the wall of the intestine with its folds preserved and only some areas of congestion. Significant villous atrophy, an important finding for the diagnosis of kwashiorkor type malnutrition, was observed. The colon had mucosal edema; however, its morphology was preserved macroscopically. The reduction of associated lymphoid tissue is notable as well as the presence of lymph node neurons both in the submucosal plexuses as in the myenteric.
The cuts corresponding to the pancreas showed normal architecture, without data suggestive of cystic fibrosis. The exocrine and endocrine tissues were without changes and only areas with steatonecrosis were seen in the peripancreatic adipose tissue (Fig. 10).
Figure 10 Normal architecture of the pancreas (HE x10).
The kidneys weighed within the expected range (60 g vs. 60 g). They were lobulated and the vesical mucosa was edematous. At the cut, the cortex-medulla relationship was preserved and important areas of congestion were seen at the medullary level. The different histological cuts of the cortex and those of the medulla showed glomeruli of normal histological characteristics and the presence of some calcifications in the lumen of the tubules as well as some bacterial colonies and loss of tubular epithelium.
CNS had a weight of 700 g vs. 780 g. Widening of the circumvolutions was observed, secondary to atrophy and malnutrition. The different cuts showed a structurally normal brain, only with loss of the cortex-white matter relationship. Histological cuts showed neurons with data of hypoxia, eosinophilia of the cytoplasm and pyknosis of the nuclei.
The patient had various different skin lesions. She had orthokeratotic hyperkeratosis, basal pigmentation and mild vacuolation. These data are nonspecific and can be seen in different states of nutritional deficit such as niacin, thiamin and other nutritional deficiencies. In other areas corresponding to the acute lesions, a total loss of the epidermis and the flat keratinized stratified epithelium with areas of necrosis is able to be seen. However, extravasation of the erythrocytes was not seen, which represents histological data of purpura. I believe that the first lesions are nonspecific as they can be present in any nutritional deficit and the acute lesions are secondary to shock.
There was also anatomic data of shock, with contraction bands in the smooth muscles of the gastrointestinal tract and colliquative necrosis of cardiomyocytes. Retention of secretions was also observed in the lumen of the ducts of the pancreas. It does not resemble that which is seen in cystic fibrosis where the mucus is found in a concentric, not amorphous, shape such as in this case, which can be secondary to shock or dehydration. Also seen was retention of secretions in the lumen of the ducts of the salivary glands and fibrin thrombus in the lumen of the small vessels (Fig. 11).
Figure 11 Fibrin thrombus (HE x20).
Based on these findings the following diagnoses were made:
• Intestinal atrophy
• Steatonecrosis
• Nephrocalcinosis
• Cerebral atrophy (700 g vs. 780 g)
• Skin necrolysis
• Changes compatible with dermatitis due to nutritional deficit
Anatomic data of shock and DIC are the following:
• Acute tubular necrosis
• Acute alveolar damage
• Hypoxic encephalopathy
• Colliquative myocytolysis
• Ischemic hypoxic visceral myopathy
• Retention of secretions
• Fibrin thrombus
No alterations were found in the remainder of the organs. The ovary had normal histological characteristics with primary and secondary follicles. Cut of the adrenal gland showed that the gland was intact. This information supports that this was not an infection due to meningococcus because one of the characteristics of an infection due to pneumococcus is massive necrosis of the adrenal gland, i.e., Waterhouse-Friderichsen syndrome.
Postmortem cultures were positive for the following pathogens:
• Klebsiella pneumonia, Escherichia coli and Pseudomonas aeruginosa in the small intestine, colon and CSF
• Enterococcus faecalis in blood culture and liver
• Staphylococcus epidermidis in spleen
• Stenotrophomona maltophilia in the liver, left lung and CSF
It is believed that the patient had kwashiorkor type malnutrition and secondary immunodeficiency. The infectious process became complicated and she developed sepsis and septic shock due to Gram positive and Gram negative bacteria. There are no histological data that support cystic fibrosis or metabolic disease.
4.1. General Directorate (Dr. José Alberto García Aranda)
This is a clinical picture of malnutrition that is uncommon. It must be specified why the skin lesions are due to nutritional disorders because the kwashiorkor type malnutrition presents itself in children >1 year of age and the skin lesions are described as pellagrous lesions or pellagra. They have been described for 100 years and the lesions the patient presented did not look like pellagra. They appeared more like purpuric lesions.
4.2. Pathology (Dr. María Argelia Escobar Sánchez)
For the diagnosis of pellagra to be made, there are currently the following criteria: diarrhea, malnutrition, dementia, dermatitis and death. In this case it is difficult to make that diagnosis because the patient was <1 year of age and could not be evaluated for dementia. It was mentioned that there were some areas of the skin better preserved. Nonspecific changes are similar to different pathologies where there are nutritional disorders. These are characterized by hyperkeratosis, basal hypopigmentation and other types of lesions with presence of epidermal necrosis, i.e., lesions considered secondary to septic shock.
4.3. Gastroenterology (Dr. Liliana Worona Dibner)
At the level of the liver, in addition to steatosis that continues to point to cystic fibrosis of the pancreas because steatosis observed in cystic fibrosis is secondary to malnutrition, did the liver have some other alteration?
4.4. Pathology (Dr. María Argelia Escobar Sánchez)
The liver, in addition to the steatosis, did not have other alterations. It had a normal appearance. The ultrastructure was analyzed to try to rule out some primary disease of the liver. What is mentioned is that the steatosis could be a histological pattern of hepatic lesion; however, this was ruled out. On the other hand, the pancreas was normal, both the endocrine as well as the exocrine portions.
4.5. Gastroenterology (Dr. Liliana Worona Dibner)
Can cystic fibrosis be ruled out from the histological point of view?
4.6. Pathology (Dr. María Argelia Escobar Sánchez)
Yes. The pancreas is normal and retention of secretions is not characteristic of cystic fibrosis. The criteria indicate that the secretions should be in a concentric manner. Also, it is not a specific finding as the retention of secretions could be seen in different conditions such as malnutrition, dehydration and shock.
4.7. Gastroenterology (Dr. Liliana Worona Dibner)
It would be ideal to have genetic counseling and follow the family because one should consider, as a possibility, cystic fibrosis.
5. Final comments
5.1. Coordinator (Dr. Salvador Villalpando Carrión)
Taking into consideration secondary immunodeficiency in kwashiorkor type malnutrition, which is no longer seen, what role does vaccination play and what role can meningococcus have on the deterioration that the patient presented during the last 15 days?
5.2. Infectious Disease Department (Dr. Sarbelio Moreno Espinoza)
We are obliged to consider the pathogens of both immuno-compromised patients as well as immunodepressed patients. The immunodepressed condition does not exempt them from pathogens presented by immunocompetent patients. Therefore, vaccination against pneumococcus and against Haemophilus influenzae is very important. However, a patient with all the characteristics mentioned leads one to think of the usual pathogens. With regard to toxic shock, it is feasible to think of meningococcus although it is not very prevalent in Mexico. It should not be ruled out, but it is not as frequent in such early ages and there is little evidence of its existence. It was demonstrated that the adrenal glands were normal. It is more logical to think that due to the immunodeficiency, she had a translocation of bacteria from the gastrointestinal tract, which caused septic shock and multiorgan failure. I have no doubt that the pathogens that played a role were Gram negative. Regarding the scheme of antibiotics, the patient initially was treated with cefepime and vancomycin and then later was changed to a carbapenem. These pathogens were covered. However, a pathogen that was not taken into consideration and that we often see in patients this seriously ill was Stenotrophomona maltophilia, which is sensitive to quinolones or to trimethoprim with sulfamethoxazole.
5.3. Immunology laboratory (Dr. Ernesto Calderón Jaimes)
The possibility of meningococcemia can reasonably be eliminated. In these patients, imprints of septic thrombi can be made and thereby see the microorganisms. On the other hand, it is worth speculating what happened with the lipid metabolism. When this type of steatohepatitis with an exaggerated fat transformation is seen, the pathway of fatty acid synthesis is interrupted and this causes an alteration that prevents lipid metabolism. With regard to the skin lesion, there is no clear idea about what type they were or of the type of purpura.
5.4. Coordinator (Dr. Salvador Villalpando Carrión)
The patient arrived with these evidently purpuric lesions that do not show histological purpuric criteria, but we have a patient who is profoundly malnourished. In this context, due to the purpuric lesions and the lesions seen in the bone marrow in a patient who is immunocompromised, how should they be managed?
5.5. Hematology Department (Dr. Io Daiela Castillo Martínez)
Kwashiorkor cases were described in the 1950s and 1960s and, in fact, there is a publication by Dr. Samuel Dorantes.1 It should be mentioned that the term “purpura” is a clinical diagnosis in which there are ecchymotic lesions and petechiae of the skin; however, we will not delve into the pathology criteria because it is probable that clinically the patient did present with purpura. These lesions are described in up to 3% of patients with kwashiorkor, but in patients with a good general status. In this patient it does not look like purpura of malnutrition; however, it is noteworthy that these lesions were described 15 or 18 days prior to her admission. She probably had these lesions at the beginning (20 days before) when she did have a better general status, and it is purpura of the malnourished. When the patient was admitted to the hospital, it is likely that she already had a fulminant purpura because in <24 h she had lesions, skin necrosis and data of DIC, which finally lead to multiorgan failure. Infectious causes, autoimmune causes and protein C deficiency, antithrombin, etc. would need to be considered.
5.6. Coordinator (Dr. Salvador Villalpando Carrión)
Finally, there were images of fatty liver found in children with kwashiorkor and some photographs depicting lipogranulomas that arise in obesity and other diseases. There are currently other methods to study patients with kwashiorkor which, fortunately, is increasingly less frequent.
Conflict of interest
The authors declare no conflict of interest of any nature.
Received 21 April 2014;
accepted 30 April 2014
☆ Please cite this article as: Villalpando Carrión S, Romero Raizabal BL, Jaramillo Alvarado JG, Moreno Espinoza S, Castillo Martínez ID, Escobar Sánchez MA. Desnutrición tipo Kwashiorkor. Bol Med Hosp Infant Mex. 2014;71:377-386
* Corresponding author.
E-mail:villalpandoca@himfg.edu.mx (S. Villalpando Carrión).